ORIGINAL RESEARCH article
Adolescents’ mental health at school: the mediating role of life satisfaction.

- Lab for Developmental and Educational Studies in Psychology, “R. Massa” Department of Human Sciences for Education, University of Milano-Bicocca, Milan, Italy
In this study, we further developed prior research on risk and protective factors in adolescents’ mental health. More specifically, we used structural equation modelling to assess whether relationships at school with teachers and peers, and life satisfaction predicted mental health in a large sample of adolescents, while also testing for age and gender invariance. The sample comprised 3,895 adolescents ( M age = 16.7, SD = 1.5, 41.3% girls), who completed self-report instruments assessing their perceived life satisfaction, student-teacher relationship, school connectedness and mental health. Overall, the results suggested that life satisfaction acted as a mediator between adolescents’ positive school relations and their mental health. Outcomes were invariant across genders, while quality of school relations and mental health declined with age. Limitations of the study and futures lines in mental health research among adolescents are briefly discussed.

Introduction
According to the World Health Organization, mental health is ‘ a state of well-being in which every individual realizes his or her own potential, copes with the normal stresses of life, works productively and fruitfully, and is able to make a contribution to her or his community ’ ( World Health Organization, 2005 , p. 12). This definition recognises mental health as a dimension of overall health that spans a continuum from high-level wellness to severe illness, emphasising the key role of positive feelings, a sense of mastery and positive functioning ( Galderisi et al., 2015 ).
Adolescence is widely known to be a sensitive period of exposure to a range of mental disorders whose incidence has been increasing in recent decades ( Patton et al., 2014 ; Erskine et al., 2015 ). Indeed, approximately 20% of school students are now affected by diagnosable mental illnesses, with half of all mental issues developing by 14 years ( Ford et al., 2003 ; Gore et al., 2011 ). Data from studies with adolescents indicate that anxiety, depression, eating disorders, bipolar disorder, personality disorders, psychosis, addictive disorders, substance abuse, suicide attempts and self-harm are all becoming more frequent among this demographic ( Paus et al., 2008 ; Twenge et al., 2018 ; Burstein et al., 2019 ). In most cases, disorders of this kind remain undetected and, consequently, untreated until later in life ( Kessler et al., 2007 ; Patel et al., 2007 ). Furthermore, depression in young people is a highly prevalent illness worldwide, and suicide is the third most frequent cause of death among adolescents in the United States and Europe ( World Health Organization, 2012 ; Keyes et al., 2019 ; Twenge, 2020 ).
The literature shows that adolescent mental health is influenced by both individual attributes and the everyday life contexts where adolescents grow up, including school, which is a key developmental setting ( Weare and Nind, 2011 ; Cefai and Cavioni, 2015 ). Students who experience mental health difficulties at school tend to exhibit poor school adjustment, reduced concentration, low achievement, problematic social relationships and a higher rate of health risk behaviours, such as substance use, school dropout and incurring expulsion ( Valdez et al., 2011 ; Suldo et al., 2014 ; Farina et al., 2021 ).
Recent research also suggests that older adolescents may suffer a decline in mental health outcomes, with older girls reporting poorer mental health than older boys ( Inchley et al., 2020 ). This evidence has led to growing awareness of the need to address adolescents’ mental health requirements by identifying the factors that can promote or hinder their mental health in the school setting ( Eccles and Roeser, 2011 ; Cavioni et al., 2020a ). Accordingly, the aim of this study was to investigate the role of life satisfaction and school relations, as protective and risk factors for mental health, in a large sample of adolescents.
Protective and Risk Factors Associated with School Mental Health in Adolescence
Protective factors for mental health may be defined as individual and environmental characteristics that foster healthy development but also reduce the negative impact of risk factors for mental health issues ( Deković, 1999 ; O’Connell et al., 2009 ). In contrast, mental health risk factors can increase a person’s chances of developing psychological illness ( World Health Organization, 2012 ). In this research, we examined three factors that impact on adolescents’ mental health. The first is an individual factor, life satisfaction, while the second and third are school contextual factors, namely, student-teacher relationship and sense of community at school. Indeed, the literature on adolescent mental health is notably lacking in research on how the contextual factors associated with quality of school relationships interact with individual characteristics, such as life satisfaction, to shape mental health outcomes ( Torsheim and Wold, 2001 ; Craig et al., 2020 ). In the next section, we review the existing research findings for each of these key factors.
Individual Factor: Life Satisfaction
Life satisfaction is defined as ‘the global assessment of a person’s quality of life according to his own chosen criteria’ ( Andrews and Withey, 1976 , p. 478). Numerous studies have found that adolescents with higher levels of life satisfaction display better school adaptive functioning, in terms of self-efficacy, self-esteem, engagement, academic achievement, social acceptance and peer relationships, as well as lower levels of school absenteeism, dropout and behavioural problems ( Proctor et al., 2009 ; Fergusson et al., 2015 ). Conversely, adolescents with low life satisfaction are more likely to display internalising and externalising problems, social stress and substance abuse ( Zullig et al., 2001 ; Haranin et al., 2007 ).
Contextual Factors: Student-Teacher Relationship and Sense of Community at School
At the contextual level, multiple school-related factors have been associated with positive mental health outcomes in adolescents. More specifically, student-teacher relationship and sense of school community are known to serve as key protective factors via the provision of emotional and social support and safe environments ( Eccles and Roeser, 2011 ). Overall, such contextual factors are associated with a lower likelihood of negative mental health outcomes, such as perceived stress, health complaints and unhealthy behavior ( Lemma et al., 2014 ). In turn, adolescents with better mental health tend to display higher levels of attainment, decision-making ability, problem-solving skills and academic achievement ( Bonell et al., 2014 ; Suldo et al., 2014 ).
With regard to the student-teacher relationship, past research has generally assessed its positive and negative aspects and their implications for a wide range of student mental health outcomes. For example, Murray and Greenberg (2001) proposed that the relationship is formed of four components. Two concern the positive aspects of the relationship, which are affiliation with the teacher and a sense of bonding with school, and two its negative characteristics, which are dissatisfaction with the teacher and perceived school dangerousness. Studies on the positive aspects of the student-teacher relationship have shown that when it is characterised by warmth, respect, support and openness, it can have positive effects on students’ attitudes towards school, fostering an increased sense of belonging and more effective learning ( Doll et al., 2004 ; Suldo et al., 2009 ). Pianta and colleagues have extensively documented the relationship between higher levels of attachment to teachers and bonding with the school and enhanced social and emotional skills, school satisfaction, engagement and motivation on the part of the students (e.g. Pianta, 1999 ; Pianta et al., 2003 ; Pianta and Hamre, 2009 ). During adolescence, affiliation with teachers and bonds with the school can shield young people from the effects of stressful life events, promoting resilience and decreasing the likelihood of developing mental health issues, such as depression and misconduct ( Murray and Greenberg, 2001 ; Wang et al., 2013 ; Lemma et al., 2014 ; Cefai et al., 2015 , 2018 ; Höltge et al., 2021 ). In contrast, dissatisfaction with teachers and perceived school dangerousness bear the potential to negatively affect mental health outcomes ( Mameli et al., 2018 ). Indeed, studies with adolescents suggest that higher levels of dissatisfaction with teachers are associated with poor social functioning and increased peer problems, anxiety and somatic symptoms ( Mameli et al., 2018 ), whereas perceptions of poor school safety are linked with internalising and externalising behavior problems and bullying ( Nijs et al., 2014 ).
The sense of community in a school, also termed ‘school connectedness’ or ‘belongingness in the school’, is the other contextual factor that we view as a significant marker for mental health. It may be defined as ‘the extent to which students feel personally accepted, respected, included, and supported by others in the school social environment’ ( Goodenow, 1993 , p. 80). Numerous scholars have examined the impact of sense of community on adolescent mental health, finding that school connectedness is positively associated with healthy behaviours, school engagement and adjustment, motivation, school attendance, conflict resolution skills and prosocial behavior ( Vieno et al., 2005 ; Center for Disease Control and Prevention, 2009 ). Conversely, sense of community is negatively associated with school absenteeism, loneliness, worry, social isolation, emotional distress, antisocial and risky behaviours, violence, delinquency, suicidal ideation and suicide attempts ( Hirschi, 1969 ; Pretty et al., 1994 ; Joyce and Early, 2014 ).
Age and Gender Differences in Mental Health Outcomes
Cohort studies with adolescent samples indicate that the incidence of mental health disorders increases with age, especially emotional and conduct disorders, and psychosomatic problems ( Bell et al., 2019 ). According to the recent Health Behavior in School-aged Children report, adolescents’ quality of school relationships and school belonging worsen over time. In contrast, younger adolescents report higher levels of life satisfaction and better mental health ( Inchley et al., 2020 ).
With respect to gender, research has long shown that adolescent males and females tend to display different mental health patterns in relation to internalising and externalising behavioural problems ( Yeo et al., 2007 ; Nijs et al., 2014 ). For example, various studies have found that girls display more frequent and intense internalising behaviours, such as stress and anxiety (e.g. concerning interpersonal relationships, school demands, family relationships, and personal and social adjustment), as well as a higher risk of developing depression compared to males ( Angold and Rutter, 1992 ; Compas et al., 1993 ; Nolen-Hoeksema and Girgus, 1994 ). On the contrary, male adolescents are more prone to externalising behaviours, such as school problems, aggressive behavior and difficulty in managing negative emotions ( Stark et al., 1989 ; van der Ende and Verhulst, 2005 ).
Research Aims and Hypothesis
Although the existing research offers insights into the role played by individual and contextual factors in secondary school students’ mental health, most previous studies have taken a deficit-based approach by focusing on the impact of negative factors ( Ben-Arieh, 2000 ; Antaramian et al., 2010 ). Consequently, a number of authors have pointed out the need to focus on the role of both risk and protective factors and how they simultaneously impact on mental health (e.g. Seligman and Csikszentmihalyi, 2000 ; Terjesen et al., 2004 ). Furthermore, despite growing awareness of the importance of relational experience at school, relatively few studies have focused on the quality of students’ social relationships with teachers and peers and its impact on overall mental health during adolescence ( Torsheim and Wold, 2001 ; Gaete et al., 2016 ).
To address this gap, we set out to extend the recent literature on school-related factors in adolescents’ mental health by focusing on both protective and risk factors. More specifically, we used structural equation modelling (SEM) to evaluate the contributions of quality of school relations and life satisfaction to the mental health of a large group of adolescents. The model was also specified to control for effects of age, whereas a multigroup invariance test was conducted to assess differences as a function of gender. The conceptual model is illustrated in Figure 1 .
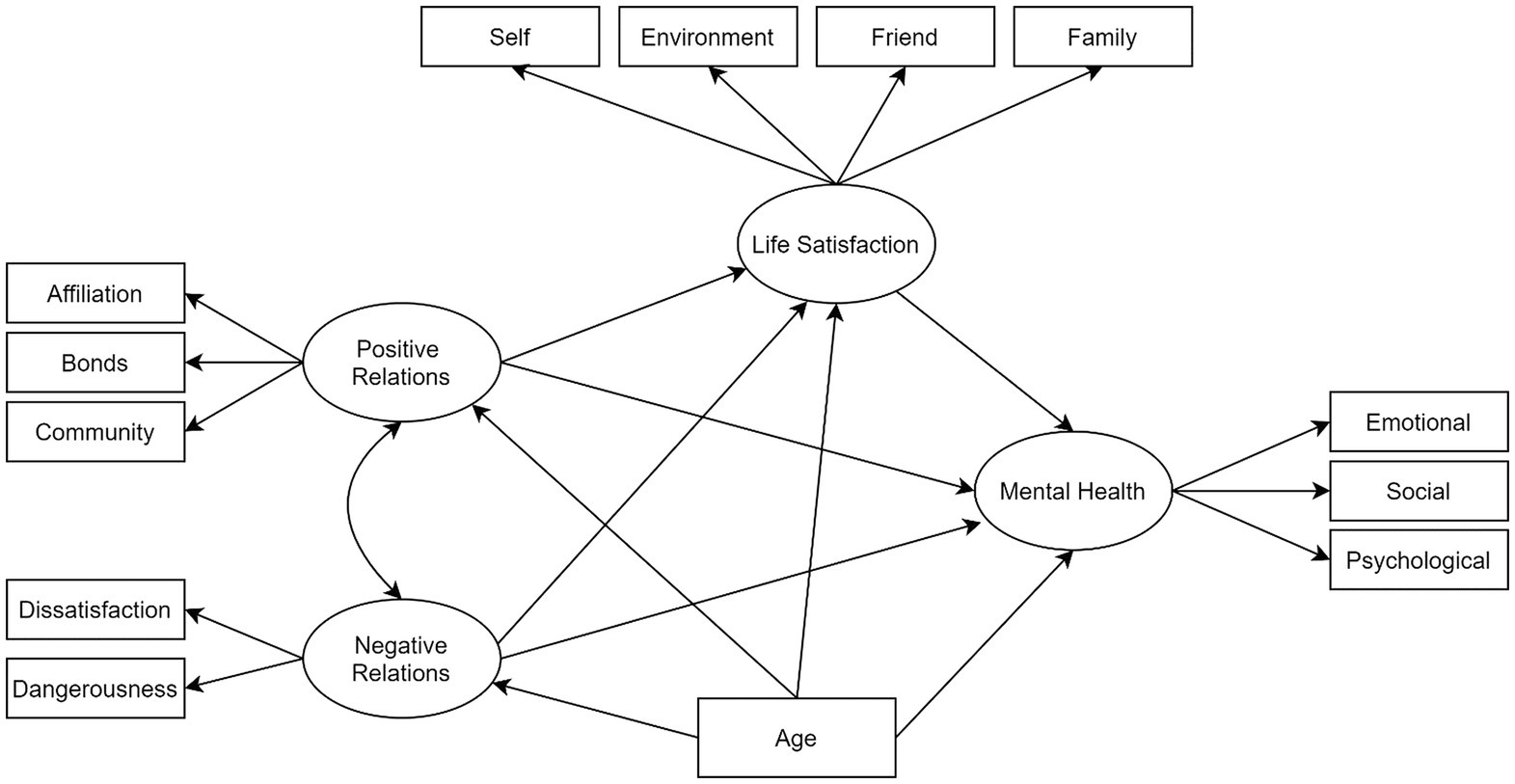
Figure 1 . Conceptual model of association between type of relationships at school, life satisfaction and mental health in adolescents.
Specifically, we expected that positive relations at school, in terms of affiliation with teachers, bonds with school and sense of school community, would be positively associated with both life satisfaction and mental health (Hypothesis 1); moreover, we predicted that negative relationships, in terms of dissatisfaction with teachers and a perception of school dangerousness, would be negatively associated with both life satisfaction and mental health (Hypothesis 2). In addition, we planned to conduct a multigroup invariance test to assess whether were differences between boys and girls in terms of the magnitude of the predicted associations. Notably, while past studies have examined gender differences in relation to life satisfaction and mental health, little research to date has attempted to model these variables in relation to the quality of young people’s relationships at school.
Materials and Methods
Participants and procedures.
The head teachers of 20 high schools located in two regions of Northern Italy (Lombardy and Piedmont) were contacted via email or by telephone and informed about the aims of the study and the research procedure. Seventeen schools agreed to participate in the study. A briefing letter was sent to the students’ parents. Informed consent and GDPR consent were obtained from all respondents and from their parents (who were free to deny their child’s participation in the study). Data were collected anonymously, and students were free to withdraw at any time during the administration of the questionnaire. Seventeen parents refused permission for their child to participate in the study; 11 students were absent during data collection, and four declined to participate.
Students responded to a set of online questionnaires in the classroom during regular school hours. The entire battery of instruments took about 15 min to complete. The questionnaires were presented in random order to minimise potential sources of measurement error ( Franke, 1997 ). Data collection was managed by the lead researcher and two research assistants, who presented the aims of the study to the students before administering the questionnaires.
A sample of 3,895 students (41.3% girls) completed the research instruments. Following a review of missing data, no questionnaires were removed from the analysis due to the use of mandatory fields in the online data collection. The final sample, aged between 15 and 19 years ( M = 16.7, SD = 1.5), included students from all three branches of the Italian high school system: professional institutes, technical institutes and lyceums. Almost half the participants (48%) were enrolled at lyceums (academic track), compared to 25.1 and 26.9% who attended professional and technical schools (vocational track), respectively. The majority (88.7%) were Italian citizens (i.e., born in Italy of Italian parents), while 11.3% came from non-Italian ethno-cultural backgrounds (parents not Italian and/or not born in Italy). The study was approved by the Ethical Committee of Milano-Bicocca University and was conducted in accordance with the Declaration of Helsinki.
Demographics
Participants were asked to specify their age, gender, school grade and nationality.
Life Satisfaction
The Italian translation of the abbreviated Multidimensional Students’ Life Satisfaction Scale (MSLSS) was used to assess life satisfaction ( Huebner, 1994 ; Huebner et al., 1998 ; Zappulla et al., 2014 ). The MSLSS is a thirty-item self-report questionnaire that measures children’s and adolescents’ life satisfaction in five domains: family (e.g. ‘I enjoy being at home with my family’), friends (e.g. ‘My friends treat me well’), school (e.g. ‘I look forward to going to school’), self (e.g. ‘Most people like me’) and living environment (‘My family’s house is nice’). Respondents are asked to rate items on a 6-point Likert scale, ranging from 1 (strongly disagree) to 6 (strongly agree). Previous studies with adolescent samples yielded acceptable validity and reliability coefficients across the five domains with alphas ranging from 0.71 to 0.91 ( Gilligan and Huebner, 2007 ; Sawatzky et al., 2009 ; Huebner et al., 2012 ; Zappulla et al., 2014 ). Cronbach’s reliability values for the present study were as follows: family ( α = 0.89), friend ( α = 0.85), environment ( α = 0.75), self ( α = 0.73) and school ( α = 0.79).
Student-Teacher Relationship
Students’ perceptions of their relationships with teachers and bonds with school were evaluated using the Italian version of the Student-Teacher Relationship Questionnaire (STRQ; Tonci et al., 2012 ) developed by Murray and Greenberg (2001) . The STRQ comprises 22 items to be rated on a 4-point Likert scale (from 1 = almost never or never true to 4 = almost always or always true). The questionnaire evaluates the quality of individual students’ relationships with their teachers and their perceptions of their school environment in terms of four factors: affiliation with teacher (e.g. ‘My teachers pay a lot of attention to me’), dissatisfaction with teachers (e.g. ‘I feel angry with my teacher’), bonds with school (e.g. ‘I feel safe at my school’) and school dangerousness (e.g. ‘My school is a dangerous place to be’). The four factors have been found to be reliable, with Cronbach’s alphas ranging between 0.66 and 0.88 ( Murray and Greenberg, 2001 ). Cronbach’s reliability values in the present study were as follows: affiliation ( α = 0.84), bonds ( α = 0.71), dangerousness ( α = 0.66) and dissatisfaction ( α = 0.74).
Sense of Community in School
Students’ sense of community was assessed via the Italian version of the Students’ Sense of Community in School scale ( Vieno et al., 2005 ), originally developed by Samdal et al. (1998) . The questionnaire comprises six items (e.g. ‘I feel I belong at this school’) designed to assess the three dimensions of sense of community (membership, shared emotional connection and fulfilment of needs) identified by McMillan and Chavis (1986) . Responses are rated on a 5-point Likert scale (from 1 = strongly disagree to 5 = strongly agree). In previous studies, this questionnaire displayed satisfactory internal reliability with alphas ranging between 0.71 and 0.82 ( Vieno et al., 2005 ; Prati et al., 2020 ). Cronbach’s reliability value for the present study was α =0.75.
Mental Health
The Italian validated version of the Mental Health Continuum Short Form (MHC-SF) was used to assess respondent’ mental health ( Petrillo et al., 2015 ). This instrument, originally developed by Keyes (2002) , is a self-report questionnaire comprising 14 items. Informed by Keyes’ theoretical model of mental health ( Keyes, 1998 , 2002 , 2005 , 2007 ; Keyes and Waterman, 2003 ), the MHC-SF evaluates three dimensions of mental health: emotional (e.g. ‘How often did you feel happy?’), social (e.g. ‘How often did you feel that you had something important to contribute to society?’) and psychological (e.g. ‘How often did you feel good at managing the responsibilities of your daily life?’). Items are rated on a 6-point Likert scale ranging from 0 (none of the time) to 5 (all of the time), based on respondents’ experience over the preceding month. Total scores on the MHC-SF range from 0 to 70, with higher scores reflecting better mental health. Among adolescents, the MHC-SF has displayed validity and satisfactory internal reliability values ranging from 0.75 to 0.91 ( Lim, 2014 ; Petrillo et al., 2014 , 2015 ; Luijten et al., 2019 ; Reinhardt et al., 2020 ). Cronbach’s reliability values for the present study were as follows: emotional ( α = 0.81), social ( α = 0.78) and psychological ( α = 0.83).
Statistical Analysis and SEM
In order to test the network of associations between adolescents’ mental health and the other study variables, we adopted a SEM approach ( Thakkar, 2020 ). SEM techniques are based on multivariate data analysis and combine empirical measurement with theoretical inquiry by allowing latent factors to be estimated along with patterns of associations among observed variables ( Guo et al., 2009 ; Cavioni et al., 2020b ; Farina et al., 2020 ; Veronese et al., 2020 ). SEM permits estimation of the magnitude and direction of paths among variables and the evaluation of total, direct and indirect effects ( Hair et al., 2017 ).
It is essentially a method of testing hypotheses via a confirmatory rather than an exploratory approach. In the present paper, we estimated a model with four latent variables and 13 empirical indicators (see Figure 1 ).
Moving from left to right in the figure, two of the latent constructs were positive and negative school relationships as operationalised by five empirical indicators: affiliation with teachers, bonds with school, sense of community, dissatisfaction with school and school dangerousness. Next, life satisfaction was assessed in relation to four domains: self, friends, family and environment. The school domain of the MSLSS was omitted from the analysis due to its collinearity with other latent variables (e.g. positive and negative school relations ). Finally, the target latent variable mental health was modelled via its psychological, emotional and social dimensions. In line with the research hypotheses, we estimated the direct effects of positive and negative school relations on both life satisfaction and mental health. All variables were viewed as endogenous conceptual components of the model, whereas participants’ age was modelled as an exogenous variable. Estimated total effects were broken down into direct and indirect effects ( Kline, 2015 ).
Following standard procedures for SEM, we evaluated the following goodness-of-fit indices: root mean square error of approximation (RMSEA; RMSEA < 0.05; Madeu-Olivares et al., 2018 ), standardised root mean square residual (SRMR; SRMR < 0.05) ( Sass et al., 2014 ); normed fit index (NFI; NFI > 0.95; Marsh et al., 2013 ), Tucker-Lewis index (TLI; TLI > 0.95; Morin et al., 2013 ) and comparative fit index (CFI; CFI > 0.95; Morin et al., 2013 ). As currently recommended (e.g. Bollen and Long, 1993 ; Kaplan and Depaoli, 2012 ) for SEM, we used both Monte Carlo simulation and bootstrapping methods to estimate confidence limits with a set of random samples ( k = 500). We calculated the given indirect effects for each of the k samples and the mean value for the selected pool of samples. Finally, we conducted a multigroup invariance test (MGCFA) to determine whether similar response patterns were obtained across gender-based cohorts. The MGCFA also helped us to specify the model structure with the best potential for generalisation ( Brown et al., 2017 ). The hypothesis of measurement invariance was to be accepted if configural invariance (all parameters free to vary but structural model held constant), metric invariance (factor loadings set to be equal in both groups), scalar invariance (factor loadings and item intercepts constrained) and full invariance (all parameters were equivalent across the groups) were all supported. Structural equivalence was to be rejected if the indexed variations were statistically significant. The cut-off points (CFI, RMSEA and SRMR) for rejecting measurement invariance were set at Δ = 0.01, corresponding to a p level of 0.01 ( Chen, 2007 ).
We also estimated Mahalanobis’ distance ( p < 0.001) to detect potentially multivariate outliers; no cases needed to be removed from the dataset. Finally, we assessed the distribution of the data for each of the study measures. None of the kurtosis or skewness values exceeded the recommended limits [−1,+1], and consequently, the maximum likelihood method ( Gath and Hayes, 2006 ) was adopted to estimate the parameters for the SEM analysis. The software used for all analyses was Amos 23.0 ( Arbuckle, 2014 ).
Table 1 provides a summary of the main descriptive statistics for the variables under study (e.g. mean values and standard deviations), along with their zero-order correlations.
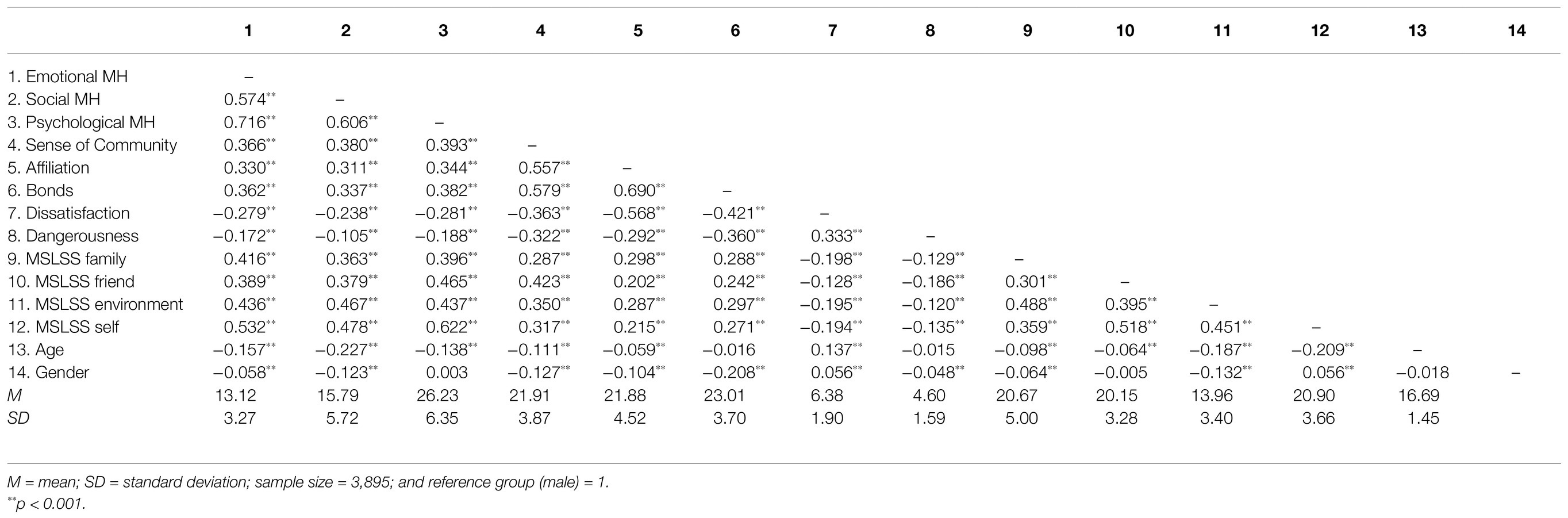
Table 1 . Zero-order correlations and main descriptive statistics for mental health, life satisfaction and positive/negative school relations.
In general, the zero-order correlations revealed statistically significant, robustly positive patterns of association between mental health and positive school relations, with r values ranging between 0.382 (psychological mental health and bonds) and 0.311 (social mental health and affiliation). Furthermore, mental health was negatively associated with negative relations, with an especially robust association between dissatisfaction and the psychological dimension of mental health. However, the strongest patterns of association in terms of statistical significance and magnitude of effect were observed between mental health and life satisfaction, with values ranging between 0.622 (psychological mental health and satisfaction with self) and 0.379 (social mental health and satisfaction with friends). With regard to demographic variables, age was found to be negatively associated with all aspects of mental health and life satisfaction, while mixed patterns of association were found between age and school relations. Concerning gender differences, zero-order correlations were generally low or not statistically significant, with the exception of bonds with school ( r = −0.108), a measure on which boys scored more poorly than girls. Overall, the correlational analysis provided support for testing a structural equation model with all the study variables.
The fit analysis (see Figure 1 ) suggested that the empirical data provided a good fit for conceptual model. All the fit indexes endorsed the full acceptance of the model: NFI = 0.954, NNFI = 0.954, CFI = 0.956, RMSEA = 0.066 [C.I. 90th = 0.063–0.070] and SRMR = 0.041. Total, direct and indirect standardised effects are reported in Table 2 . Indirect effects reflect interaction among three variables, while a direct effect represents the impact of a single determinant on a given target variable.
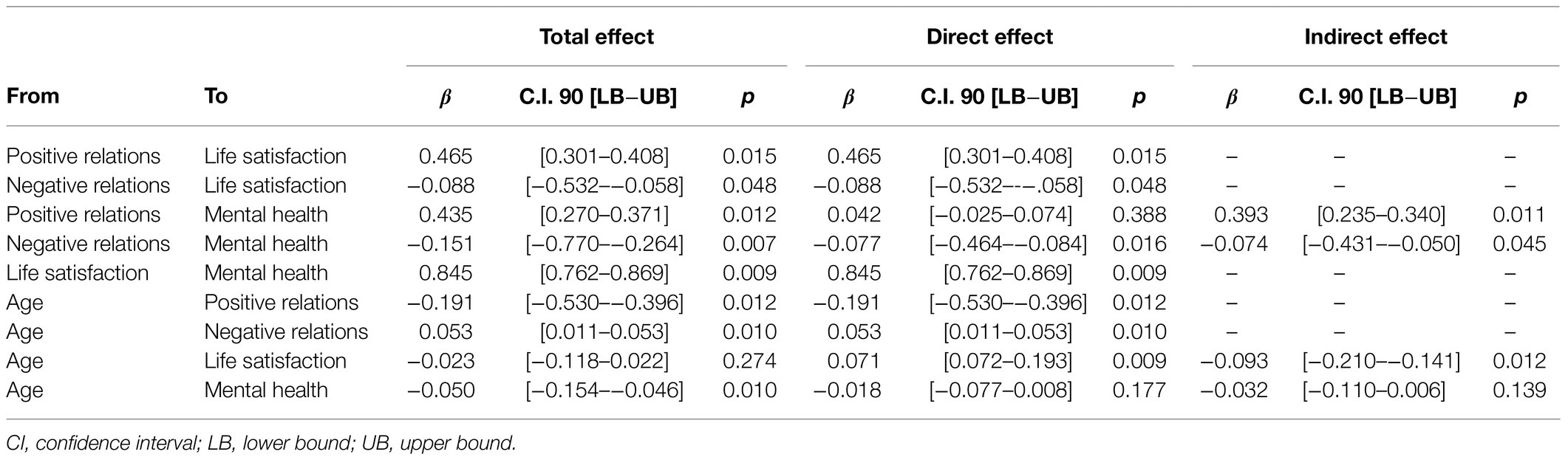
Table 2 . Breakdown of total, direct and indirect standardised effects identified via the structural model.
Again, moving from left to right, the latent variable, positive school relations, had significant effects on both life satisfaction ( β = 0.478) and mental health ( β = 0.435). Interestingly, the direct pathway between positive relations and mental health was negligible and non-significant ( β = 0.042), meaning that life satisfaction fully mediated the association between these two variables (the magnitude of the indirect effect was 0.393). Negative school relations had significant total effects on both life satisfaction ( β = − 0.088) and mental health ( β = −0.151), although the magnitude of these effects was small compared to the effects of positive relationships. Finally, a large, statistically significant, positive pathway was observed from life satisfaction to mental health ( β = 0.845). In terms of pathways between age and latent variables, older adolescents generally reported weaker positive relations ( β = −0.191), poorer mental health ( β = −0.05) and stronger negative relations ( β = 0.053). In contrast, no statistically significant pathway was found between age and life satisfaction. The results of the invariance test of gender-based cohorts of adolescents are reported in Table 3 and Figure 2 .
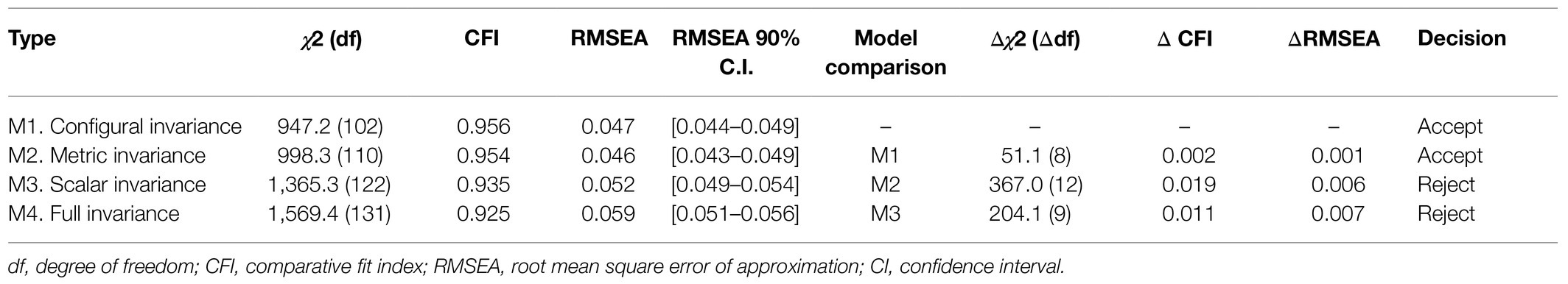
Table 3 . Multigroup analysis of the structural equation model: fit indexes and model comparison.
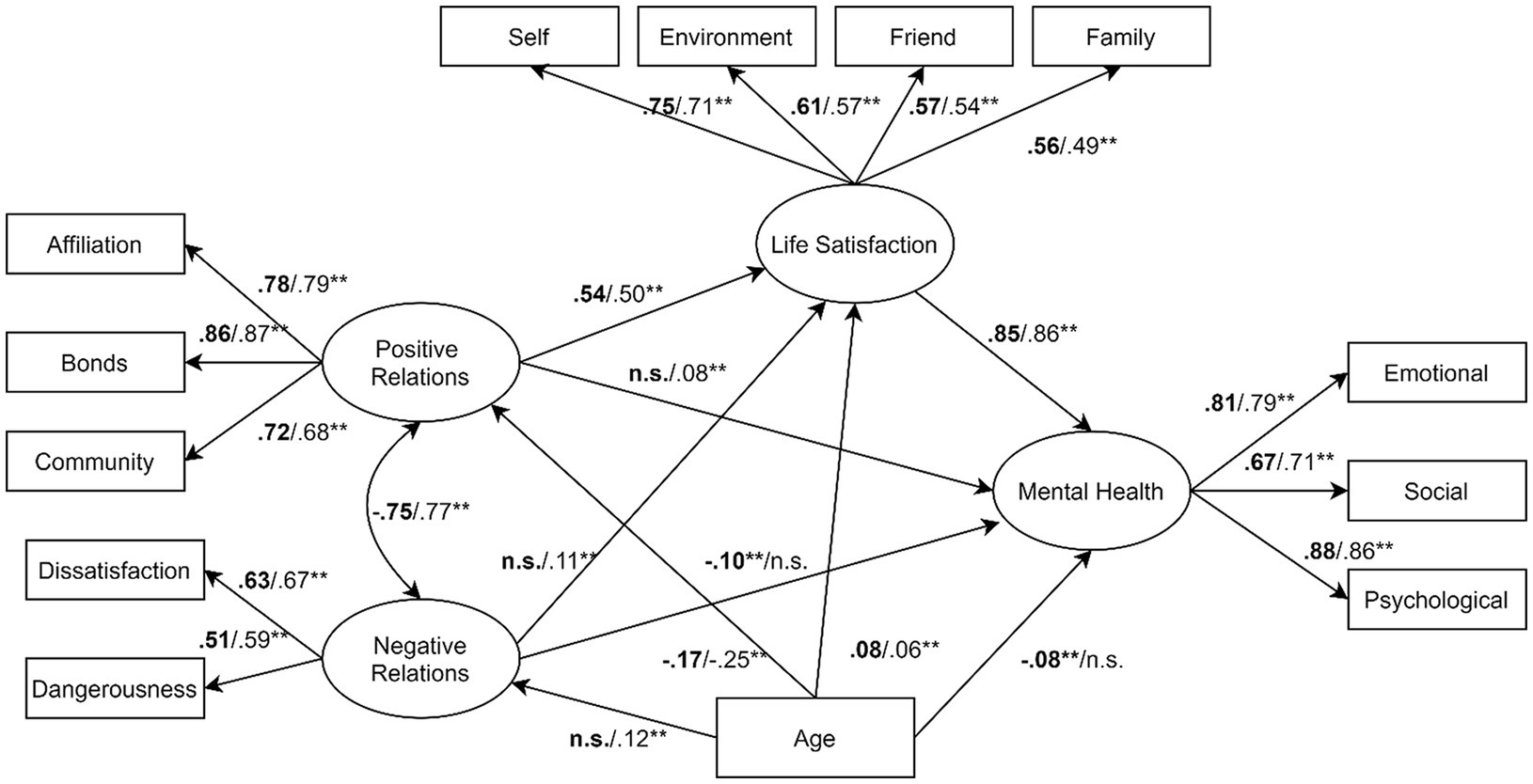
Figure 2 . Structural model and standardised direct effects as resulting from invariance test ( n = 3,895). ** p < 0.01; n.s. = not statistically significant. Values for males were reported in bold.
The main outcome of the invariance analysis was that the structural equation model supported the first two levels of invariance between boys and girls. Specifically, only configural and metric invariance were confirmed, meaning that the theorised set of variables and pathways held in the two groups, but males and females obtained different intercept values. Although the set of pathways remained substantially the same in the two cohorts of adolescents, there were minor differences concerning the latent variable negative relations: specifically, there was a small inverse association ( β = −0.109) between negative relations and life satisfaction for girls, but this pathway was not statistically significant for boys.
The main aim of the present study was to investigate – via SEM – whether and to what extent quality of school relations and life satisfaction predicted mental health in a large sample of adolescents. We obtained the following key findings, which are discussed below in further detail. First, we found strong associations between the quality of adolescents’ school relations, their life satisfaction and their mental health. Second, life satisfaction, which was positively associated with mental health, was found to act as mediator between adolescents’ positive relationships and their mental health. Third, both the quality of school relations and life satisfaction appeared to protect mental health, and this outcome did not significantly vary as a function of gender. Finally, students’ quality of school relations and mental health deteriorated with age.
Associations Among Quality of School Relations, Life Satisfaction and Mental Health
The first main outcome confirmed our leading research hypothesis, namely that positive school relations, in terms of affiliation with teachers, bond with school and sense of community, would be positively associated with mental health and life satisfaction. The second hypothesis was also borne out by the data: specifically, negative school relations, in terms of dissatisfaction with teachers and perceptions of school dangerousness, were negatively associated with life satisfaction and mental health. The structural equational model also indicated that the quality of school relations – operationalised via affiliation with teachers, bonds with school and sense of community – was associated with adolescents’ mental health. Although the literature acknowledges the importance of students’ social and relational experience, and especially the role of teachers in promoting it (e.g. Pianta, 1999 ; Roorda et al., 2011 ; Cavioni et al., 2017 ), few recent studies have been focused on how these factors may be related to one another during adolescence. Our findings also underscored the key role of student-teacher relationships, especially in the high school setting where they tend to become more impersonal ( Roorda et al., 2011 ). This is in line with recent work by Ibrahim and El Zaatari (2020) , who concluded that teacher-student relationships are the most important relationship in the school context and have positive effects on students’ mental health when characterised by empathy, closeness, love, care, support, respect and reciprocity. Another remarkable outcome of our model concerns the impact of adolescents’ self-perceived bonds with their school and sense of community at school on mental health. Although existing studies have examined the association between adolescents’ school bonds and sense of community on mental health, traditionally the focus has been on their role in reducing emotional and conduct issues, hyperactivity, peer problems, depression and anxiety ( Lester et al., 2013 ; Gaete et al., 2016 ). Our findings, on the other hand, offer the novel insight that students’ school bonds and sense of community actually act as preventive factors. Consequently, mental health in schools needs to be promoted by building collective beliefs, values and expectations among students, teachers and all members of the school community. Overall, these outcomes are consistent with the positive psychology approach, which emphasises the importance of identifying and fostering positive indicators of mental health rather than merely detecting and seeking to mitigate factors that cause psychopathology ( Seligman and Csikszentmihalyi, 2000 ; Antaramian et al., 2008 ).
The Moderating Role of Life Satisfaction
Our second finding was that life satisfaction played a key mediating role between adolescents’ positive relationships at school and their mental health. In our model, life satisfaction was operationalised as adolescents’ subjective cognitive appraisal of their quality of life in the domains of self, environment, friends and family. We set out to investigate how contextual factors at school interact with individual characteristics to shape adolescents’ mental health, and our results suggest that life satisfaction, conceptualised as an individual factor, may play a significant part in this process. In addition, although the association between life satisfaction and mental health has been widely examined in adult populations, few studies have explored this aspect among adolescents. Existing research conducted with teenage samples has been focused on life satisfaction as a buffer against negative life events and stress, and the development of externalising and internalising behavioural problems ( McKnight et al., 2002 ; Suldo and Huebner, 2004 ; Sawatzky et al., 2010 ). Our results suggest that life satisfaction for adolescents not only acts as a barrier mitigating the impact of negative events and mental health problems ( Lazarus, 1991 ; Suldo and Huebner, 2004 ) but also represents a key psychological resource through which positive relationships can boost mental health.
Gender Invariance
Overall, we identified minor gender differences in the relative strength of the associations among the variables. Previous studies with adolescents mainly examined the role of gender in terms of differential patterns of internalising and externalising behavioural problems in boys versus girls (e.g. van der Ende and Verhulst, 2005 ). However, in this study, we explored the role of gender by applying a multigroup invariance test to compare the performance of our conceptual model across gender groups ( Ornaghi et al., 2016 ). Our structural equation model was aimed at identifying contextual and individual resources that contribute to mental health rather than comparing psychological symptoms between genders. The results suggested that positive school relations and life satisfaction protect the school mental health of both girls and boys.
Age Invariance
We found that older students reported weaker positive school relations and poorer mental health, along with a higher incidence of negative school relations. These findings are consistent with previous studies that have identified declines over time in adolescents’ mental health outcomes as well as in their perceptions of emotional support from teachers ( Eccles and Roeser, 2011 ; Bayram Özdemir and Özdemir, 2020 ). Given that adolescence is a major life period marked by numerous individual and contextual challenges with the potential to impact on adolescents’ mental health ( Dwivedi and Harper, 2004 ; Grazzani Gavazzi et al., 2011 ), our results add to our understanding of the association between school relations and mental health across age groups, confirming that student mental health hits its lowest point during late adolescence.
Limitation and Future Studies
Some limitations of this study should be noted. First, although we analysed data from a large sample of adolescents, the outcomes cannot be generalised to early adolescence nor to adolescents with atypical development. Second, the study was conducted on a sample of adolescents mainly enrolled at lyceums. Consequently, the findings can be generalised with caution to the whole population of high school students attending professional and technical institutes. Third, given that the present data were collected in Italian schools from only two regions, the outcome could not be automatically extended to adolescents from the whole Italian Country.
Finally, while we examined the impact of school relations and life satisfaction on adolescents’ mental health at a single time point, relationships at school are never static. We, therefore, recommend that the future research adopt a longitudinal design to investigate how the contribution of the school relationships to young people’s mental health may evolve over time.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of Milano-Bicocca. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
VC has made substantial contributions to the conception and design of the research, to the collection, input, scoring and interpretation of the data, and drafting of the manuscript. IG made a key contribution to designing the research, interpreting the data, drafting and revising the manuscript. VO contributed to interpreting the data and revising the manuscript critically. AA has been involved in collecting the data and revising the manuscript critically. AP made a key contribution to analysing and interpreting the data and in drafting the manuscript. All authors read and approved the final manuscript.
This study was co-funded by the Erasmus+ programme of the European Union (Reference number: 606689-EPP_2018-2-IT-PI-POLICY).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We wish to thank Veronica Re and Raffaella Roncoroni who collected the data in schools. We also would like to thank the head teachers and teachers who facilitated the data collection in school as well as the students who join the study and their parents who authorised the students’ participation.
Andrews, F. M., and Withey, S. B. (1976). Social Indicators of Well-Being. New York: Plenum.
Google Scholar
Angold, A., and Rutter, M. (1992). The effects of age and pubertal status on depression in a large clinical sample. Dev. Psychopathol. 4, 5–28. doi: 10.1017/S0954579400005538
CrossRef Full Text | Google Scholar
Antaramian, S. P., Huebner, E. S., Hills, K. J., and Valois, R. F. (2010). A dual-factor model of mental health: Toward a more comprehensive understanding of youth functioning. Am. J. Orthopsychiatry 80, 462–472. doi: 10.1111/j.1939-0025.2010.01049.x
PubMed Abstract | CrossRef Full Text | Google Scholar
Antaramian, S. P., Huebner, E. S., and Valois, R. F. (2008). Adolescent life satisfaction. Appl. Psychol. 57, 112–126. doi: 10.1111/j.1464-0597.2008.00357.x
Arbuckle, J. L. (2014). Amos 23.0 User’s Guide. Chicago, US: IBM SPSS.
Bayram Özdemir, S., and Özdemir, M. (2020). How do adolescents’ perceptions of relationships with teachers change during upper-secondary school years? J. Youth Adolesc. 49, 921–935. doi: 10.1007/s10964-019-01155-3
Bell, S., Audrey, S., Gunnell, D., Cooper, A., and Campbell, R. (2019). The relationship between physical activity, mental wellbeing and symptoms of mental health disorder in adolescents: a cohort study. Int. J. Behav. Nutr. Phys. Act. 16:138. doi: 10.1186/s12966-019-0901-7
Ben-Arieh, A. (2000). Beyond welfare: Measuring and monitoring the state of children: New trends and domains. Soc. Indic. Res. 52, 235–257. doi: 10.1023/A:1007009414348
Bollen, K. A., and Long, J. S. (eds.) (1993). Testing Structural Equation Models. London, UK: Sage Publications, Inc.
Bonell, C., Humphrey, N., Fletcher, A., Moore, L., Anderson, R., and Campbell, R. (2014). Why schools should promote students’ health and wellbeing. Br. Med. J. 13:g3078. doi: 10.1136/bmj.g3078
Brown, G. T., Harris, L. R., O’Quin, C., and Lane, K. E. (2017). Using multi-group confirmatory factor analysis to evaluate cross-cultural research: identifying and understanding non-invariance. Int. J. Res. Meth. Educ. 40, 66–90. doi: 10.1080/1743727X.2015.1070823
Burstein, B., Agostino, H., and Greenfield, B. (2019). Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007-2015. JAMA Pediatr. 173, 598–600. doi: 10.1001/jamapediatrics.2019.0464
Cavioni, V., Grazzani, I., and Ornaghi, V. (2017). Social and emotional learning for children with learning disability: implications for inclusion. Int. J. Emot. 9, 100–109.
Cavioni, V., Grazzani, I., and Ornaghi, V. (2020a). Mental health promotion in schools: A comprehensive theoretical framework. Int. J. Emot. 12, 65–82.
Cavioni, V., Grazzani, I., Ornaghi, V., Pepe, A., and Pons, F. (2020b). Assessing the factor structure and measurement invariance of the Test of Emotion Comprehension (TEC): a large cross-sectional study with children aged 3-10 Years. J. Cogn. Dev. 21, 406–424. doi: 10.1080/15248372.2020.1741365
Cefai, C., Arlove, A., Duca, M., Galea, N., Muscat, M., and Cavioni, V. (2018). RESCUR Surfing the Waves: an evaluation of a resilience programme in the early years. Pastor. Care Educ. 36, 189–204. doi: 10.1080/02643944.2018.1479224
Cefai, C., and Cavioni, V. (2015). “Mental health promotion in school: An integrated, school-based, whole school,” in Promoting Psychological Well-Being in Children and Families. ed. B. Kirkcaldy (London: Palgrave Macmillan), 52–67.
Cefai, C., Cavioni, V., Bartolo, P., Simões, C., Miljevic-Ridicki, R., Bouilet, D., et al. (2015). Social inclusion and social justice: a resilience curriculum for early years and elementary schools in Europe. J. Multicult. Educ. 9, 122–139. doi: 10.1108/JME-01-2015-0002
Center for Disease Control and Prevention (2009). School Connectedness: Strategies for Increasing Protective Factors Among Youth. Atlanta, GA, US: Department of Health and Human Services.
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Modeling 14, 464–504. doi: 10.1080/10705510701301834
Compas, B. E., Orosan, P. G., and Grant, K. E. (1993). Adolescent stress and coping: Implications for psychopathology during adolescence. J. Adolesc. 16, 331–349. doi: 10.1006/jado.1993.1028
Craig, B. A., Morton, D. P., Morey, P. J., Kent, L. M., Beamish, P., Gane, A. B., et al. (2020). Factors predicting the mental health of adolescents attending a faith-based Australian school system: A multi-group structural equation analysis. J. Ment. Health 29, 401–409. doi: 10.1080/09638237.2019.1608929
Deković, M. (1999). Risk and protective factors in the development of problem behavior. J. Youth Adolesc. 28, 667–685. doi: 10.1023/A:1021635516758
Doll, B., Zucker, S., and Brehm, K. (2004). Resilient Classrooms: Creating Healthy Environments for Learning. New York, USA: Guilford Press.
Dwivedi, K. N., and Harper, P. B. (2004). Promoting the Emotional Well-Being of Children and Adolescents and Preventing their Mental Ill Health: A Handbook. London, UK: Jessica Kingsley Publishers.
Eccles, J. S., and Roeser, R. W. (2011). Schools as developmental contexts during adolescence. J. Res. Adolesc. 21, 225–241. doi: 10.1111/j.1532-7795.2010.00725.x
Erskine, H., Moffitt, T., Copeland, W., Ferrari, A., Patton, G., Degenhardt, L., et al. (2015). A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychol. Med. 45, 1551–1563. doi: 10.1017/S0033291714002888
Farina, E., Ornaghi, V., Pepe, A., Fiorilli, C., and Grazzani, I. (2020). High school student burnout: Is empathy a protective or risk factor? Front. Psychol. 11:897. doi: 10.3389/fpsyg.2020.00897
Farina, E., Pepe, A., Ornaghi, V., and Cavioni, V. (2021). Trait emotional intelligence and school burnout discriminate between high and low alexithymic profiles: a study with female adolescents. Front. Psychol. 12:645215. doi: 10.3389/fpsyg.2021.645215
Fergusson, D. M., McLeod, G. F., Horwood, L. J., Swain, N. R., Chapple, S., and Poulton, R. (2015). Life satisfaction and mental health problems (18 to 35 years). Psychol. Med. 45, 2427–2436. doi: 10.1017/S0033291715000422
Ford, T., Goodman, R., and Meltzer, H. (2003). The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. J. Am. Acad. Child Adolesc. Psychiatry 42, 1203–1211. doi: 10.1097/00004583-20
Franke, G. H. (1997). “The whole is more than the sum of its parts”: The effects of grouping and randomizing items on the reliability and validity of questionnaires. Eur. J. Psychol. Assess. 13, 67–74. doi: 10.1027/1015-5759.13.2.67
Gaete, J., Rojas-Barahona, C. A., Olivares, E., and Araya, R. (2016). Brief report: Association between psychological sense of school membership and mental health among early adolescents. J. Adolesc. 50, 1–5. doi: 10.1016/j.adolescence.2016.04.002
Galderisi, S., Heinz, A., Kastrup, M., Beezhold, J., and Sartorius, N. (2015). Toward a new definition of mental health. World Psychiatry 14, 231–233. doi: 10.1002/wps.20231
Gath, E. G., and Hayes, K. (2006). Bounds for the largest Mahalanobis distance. Linear Algebra Appl. 419, 93–106. doi: 10.1016/j.laa.2006.04.007
Gilligan, T. D., and Huebner, S. (2007). Initial development and validation of the multidimensional students’ life satisfaction scale–adolescent version. Appl. Res. Qual. Life 2, 1–16. doi: 10.1007/s11482-007-9026-2
Goodenow, C. (1993). The psychological sense of school membership among adolescents: Scale development and educational correlates. Psychol. Sch. 30, 79–90. doi: 10.1002/1520-6807(199301)30:1<79::AID-PITS2310300113>3.0.CO;2-X
Grazzani Gavazzi, I., Ornaghi, V., and Antoniotti, C. (2011). Children’s and adolescents’ narratives of guilt: antecedents and mentalization. Eur. J. Dev. Psychol. 8, 311–330. doi: 10.1080/17405629.2010.491303
Gore, F. M., Bloem, P., Patton, G. C., Joseph, V., Coffey, C., Sawyer, S. M., et al. (2011). Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet 377, 2093–2102. doi: 10.1016/S0140-6736(11)60512-6
Guo, B., Perron, B. E., and Gillespie, D. F. (2009). A systematic review of structural equation modelling in Ssial work research. Br. J. Soc. Work. 39, 1556–1574. doi: 10.1093/bjsw/bcn101
Hair, J. F., Hult, G. T., Ringle, C. M., Sarstedt, M., and Thiele, K. O. (2017). Mirror, mirror on the wall: A comparative evaluation of composite-based structural equation modeling methods. J. Acad. Mark. Sci. 45, 616–632. doi: 10.1007/s11747-017-0517-x
Haranin, E. C., Huebner, E. S., and Suldo, S. M. (2007). Predictive and incremental validity of global and domain-based adolescent life satisfaction reports. J. Psychoeduc. Assess. 25, 127–138. doi: 10.1177/0734282906295620
Hirschi, T. (1969). Causes of Delinquency. Berkeley, CA: University of California Press.
Höltge, J., Theron, L., Cowden, R. G., Govender, K., Maximo, S. I., Carranza, J. S., et al. (2021). A Cross-country network analysis of adolescent resilience. J. Adolesc. Health 68, 580–588. doi: 10.1016/j.jadohealth.2020.07.010
Huebner, E. S. (1994). Preliminary development and validation of a multidimensional life satisfaction scale for children. Psychol. Assess. 6, 149–158. doi: 10.1037/1040-3590.6.2.149
Huebner, E. S., Laughlin, J., Ash, C., and Gilman, R. (1998). Further validation of the multidimensional students’ life satisfaction scale. J. Psychoeduc. Assess. 16, 118–134. doi: 10.1177/073428299801600202
Huebner, E. S., Zullig, K. J., and Saha, R. (2012). Factor structure and reliability of an abbreviated version of the multidimensional students’ life satisfaction scale. Child Indic. Res. 5, 651–657. doi: 10.1007/s12187-012-9140-z
Ibrahim, A., and El Zaatari, W. (2020). The teacher–student relationship and adolescents’ sense of school belonging. J. Youth Adolesc. 25, 382–395. doi: 10.1080/02673843.2019.1660998
Inchley, J., Currie, D., Budisavljevic, S., Torsheim, T., Jåstad, A., Cosma, A., et al. (2020). Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behavior in School-aged Children (HBSC) survey in Europe and Canada. International report. Vol . 1. Key findings. Copenhagen: WHO Regional Office for Europe.
Joyce, H. D., and Early, T. J. (2014). The impact of school connectedness and teacher support on depressive symptoms in adolescents: A multilevel analysis. Child Youth Serv. Rev. 39, 101–107. doi: 10.1016/j.childyouth.2014.02.005
Kaplan, D., and Depaoli, S. (2012). “Bayesian structural equation modeling,” in Handbook of Structural Equation Modeling. ed. R. H. Hoyle (New York, US: The Guilford Press), 650–673.
Kessler, R. C., Angermeyer, M., Anthony, J. C., De Graaf, R. O. N., Demyttenaere, K., Gasquet, I., et al. (2007). Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s world mental health survey initiative. World Psychiatry 6, 168–176.
PubMed Abstract | Google Scholar
Keyes, C. L. (1998). Social well-being. Soc. Psychol. Q. 61, 121–140. doi: 10.2307/2787065
Keyes, C. L. (2002). The mental health continuum: From languishing to flourishing in life. J. Behav. Health Serv. Res. 43, 207–222. doi: 10.2307/3090197
Keyes, C. L. (2005). The subjective well-being of America’s youth: Toward a comprehensive assessment. Adolesc. Fam. Health 4, 3–11.
Keyes, C. L. (2007). Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. Am. Psycho. 62, 95–108. doi: 10.1037/0003-066X.62.2.95
Keyes, K. M., Gary, D., O’Malley, P. M., Hamilton, A., and Schulenber, J. (2019). Recent increases in depressive symptoms among U.S. adolescents: trends from 1991 to 2018. Soc. Psychiatry Psychiatr. Epidemiol. 54, 987–996. doi: 10.1007/s00127-019-01697-8
Keyes, C. L., and Waterman, M. B. (2003). “Dimensions of well-being and mental health in adulthood,” in Well-Being: Positive Development Throughout the Life Course. eds. M. Bornstein, L. Davidson, C. M. Keyes, and K. Moore (Hillsdale, NJ: Erlbaum), 477–497.
Kline, R. B. (2015). Principles and Practice of Structural Equation Modeling. 4th Edn . New York: The Guilford Press.
Lazarus, R. (1991). Emotion and Adaptation. New York: Oxford University Press.
Lemma, P., Borraccino, A., Berchialla, P., Dalmasso, P., Charrier, L., Vieno, A., et al. (2014). Well-being in 15-year-old adolescents: a matter of relationship with school. J. Public Health 37, 573–580. doi: 10.1093/pubmed/fdu095
Lester, L., Waters, S., and Cross, D. (2013). The relationship between school connectedness and mental health during the transition to secondary school: A path analysis. Aust. J. Guid. Couns. 23, 157–171. doi: 10.1017/jgc.2013.20
Lim, Y. (2014). Psychometric characteristics of the Korean mental health continuum–short form in an adolescent sample. J. Psychoeduc. Assess. 32, 356–364. doi: 10.1177/0734282913511431
Luijten, C. C., Kuppens, S., van de Bongardt, D., and Nieboer, A. P. (2019). Evaluating the psychometric properties of the mental health continuum-short form (MHC-SF) in Dutch adolescents. Health Qual. Life Outcomes 17:157. doi: 10.1186/s12955-019-1221-y
Madeu-Olivares, A., Shi, D., and Rosseel, Y. (2018). Assessing fit in structural equation models: A Monte-Carlo evaluation of RMSEA versus SRMR confidence intervals and tests of close fit. Struct. Equ. Modeling 25, 389–402. doi: 10.1080/10705511.2017.138961
Mameli, C., Biolcati, R., Passini, S., and Mancini, G. (2018). School context and subjective distress: The influence of teacher justice and school-specific well-being on adolescents’ psychological health. Sch. Psychol. Int. 39, 526–542. doi: 10.1177/0143034318794226
Marsh, H. W., Nagengast, B., and Morin, A. J. (2013). Measurement invariance of big-five factors over the life span: ESEM tests of gender, age, plasticity, maturity, and la dolce vita effects. Dev. Psychol. 49, 1194–1218. doi: 10.1037/a0026913
McKnight, C. G., Huebner, E. S., and Suldo, S. M. (2002). Relationships among stressful life events, temperament, problem behavior, and global life satisfaction in adolescents. Psychol. Sch. 39, 677–687. doi: 10.1002/pits.10062
McMillan, D. W., and Chavis, D. M. (1986). Sense of community: A definition and theory. J. Community Psychol. 14, 6–23. doi: 10.1002/1520-6629(198601)14:1<6::AID-JCOP2290140103>3.0.CO;2-I
Morin, A. J., Marsh, H. W., and Nagengast, B. (2013). “Exploratory structural equation modeling,” in Quantitative Methods in Education and the Behavioral Sciences: Issues, Research, and Teaching. Structural Equation Modeling: A Second Course. eds. R. Hancock and R. O. Mueller (Charlotte, US: IAP Information Age Publishing), 395–436.
Murray, C., and Greenberg, M. T. (2001). Relationships with teachers and bonds with school: social emotional adjustment correlates for children with and without disabilities. Psychol. Sch. 38, 25–41. doi: 10.1002/1520-6807(200101)38:1<25::AID-PITS4>3.0.CO;2-C
Nijs, M. M., Bun, C. J., Tempelaar, W. M., de Wit, N. J., Burger, H., Plevier, C. M., et al. (2014). Perceived school safety is strongly associated with adolescent mental health problem. Community Ment. Health J. 50, 127–134. doi: 10.1007/s10597-013-9599-1
Nolen-Hoeksema, S., and Girgus, J. S. (1994). The emergence of gender differences in depression during adolescence. Psychol. Bull. 115, 424–443. doi: 10.1037/0033-2909.115.3.424
O’Connell, M. E., Boat, T., and Warner, K. E. (2009). Preventing Mental, Emotional, and Behavioral Disorders Among Young People. Progress and Possibilities. Washington, DC: National Academies Press.
Ornaghi, V., Pepe, A., and Grazzani, I. (2016). False-belief understanding and language ability mediate the relationship between emotion comprehension and prosocial orientation in preschoolers. Front. Psychol. 7:1534. doi: 10.3389/fpsyg.2016.01534
Patel, V., Flisher, A. J., Hetrick, S., and Mcgorry, P. (2007). Mental health of young people: a global public-health challenge. Lancet 369, 1302–1313. doi: 10.1016/S0140-6736(07)60368-7
Patton, G. C., Coffey, C., Romaniuk, H., Mackinnon, A., Carlin, J. B., Degenhardt, L., et al. (2014). The prognosis of common mental disorders in adolescents: A 14-year prospective cohort study. Lancet 383, 1404–1411. doi: 10.1016/S0140-6736(13)62116-9
Paus, T., Keshavan, M., and Giedd, J. N. (2008). Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 9, 947–957. doi: 10.1038/nrn2513
Petrillo, G., Capone, V., Caso, D., and Keyes, C. M. (2015). The mental health continuum–short form (MHC–SF) as a measure of well-being in the Italian context. Soc. Indic. Res. 121, 291–312. doi: 10.1007/s11205-014-0629-3
Petrillo, G., Caso, D., and Capone, V. (2014). Un’applicazione del mental health continuum di Keyes al contesto italiano: benessere e malessere in giovani, adulti e anziani [An application of Keyes’ mental health continuum to the Italian context: well-being and illness in youth, adults and elderly]. Psicol. della Salut. 2, 159–181. doi: 10.3280/PDS2014-002010
Pianta, R. C. (1999). Enhancing Relationships Between Children and Teachers. Washington, DC: American Psychological Association.
Pianta, R. C., and Hamre, B. K. (2009). Conceptualization, measurement and improvement of classroom processes. Educ. Res. 38, 109–119. doi: 10.3102/0013189X09332374
Pianta, R. C., Hamre, B., and Stuhlman, M. (2003). “Relationships between teachers and children,” in Comprehensive Handbook of Psychology: Educational Psychology. Vol. 7. eds. W. Reynolds and G. Miller (Hoboken, NJ: Wiley) 199–234.
Prati, G., Tomasetto, C., and Cicognani, E. (2020). Sense of community in early adolescents: Validating the scale of sense of community in early adolescents. J. Early Adolesc. 41, 309–331. doi: 10.1177/0272431620912469
Pretty, G. M., Andrewes, L., and Collett, C. (1994). Exploring adolescents’ sense of community and its relationship to loneliness. J. Community Psychol. 22, 346–358. doi: 10.1002/1520-6629(199410)22:4<346::AID-JCOP2290220407>3.0.CO;2-J
Proctor, C., Linley, P. A., and Maltby, J. (2009). Youth life satisfaction: A review of the literature. J. Happiness Stud. 10, 583–630. doi: 10.1007/s10902-008-9110-9
Reinhardt, M., Horváth, Z., Morgan, A., and Kökönyei, G. (2020). Well-being profiles in adolescence: psychometric properties and latent profile analysis of the mental health continuum model – a methodological study. Health Qual. Life Outcomes 18:95. doi: 10.1186/s12955-020-01332-0
Roorda, D., Koomen, H., Spilt, J., and Oort, F. (2011). The influence of affective teacher-student relationships on students’ school engagement and achievement: A meta-analytic approach. Rev. Educ. Res. 81, 493–529. doi: 10.3102/0034654311421793
Samdal, O., Wold, B., and Torsheim, T. (1998). “Rationale for school: The relationship between students’ perception of school and their reported health and quality of life,” in Health Behavior in School-Aged Children: Research Protocol. ed. C. Currie (Scotland: University of Edinburgh), 51–59.
Sass, D. A., Schmitt, T. A., and Marsh, H. W. (2014). Evaluating model fit with ordered categorical data within a measurement invariance framework: A comparison of estimators. Struct. Equ. Modeling 21, 167–180. doi: 10.1080/10705511.2014.882658
Sawatzky, R., Ratner, P. A., Johnson, J. L., Kopec, J. A., and Zumbo, B. D. (2009). Sample heterogeneity and the measurement structure of the multidimensional students’ life satisfaction scale. Soc. Indic. Res. 94, 273–296. doi: 10.1007/s11205-008-9423-4
Sawatzky, R., Ratner, P. A., Johnson, J. L., Kopec, J. A., and Zumbo, B. D. (2010). Self-reported physical and mental health status and quality of life in adolescents: a latent variable mediation model. Health Qual. Life Outcomes 8:17. doi: 10.1186/1477-7525-8-17
Seligman, M. E., and Csikszentmihalyi, M. (2000). Positive psychology: An introduction. Am. Psychol. 55, 5–14. doi: 10.1037/0003-066X.55.1.5
Stark, L. J., Spirito, A., Williams, C. A., and Guevremont, D. C. (1989). Common problems and coping strategies I: Findings with normal adolescents. J. Abnorm. Child Psychol. 17, 203–212. doi: 10.1007/BF00913794
Suldo, S. M., Friedrich, A. A., White, T., Farmer, J., Minch, D., and Michalowski, J. (2009). Teacher support and adolescents’ subjective well-being: A mixed-methods investigation. School Psych. Rev. 38, 67–85. doi: 10.1080/02796015.2009.12087850
Suldo, S. M., Gormley, M. J., DuPaul, G. J., and Anderson-Butcher, D. (2014). The impact of school mental health on student and shool-level academic outcomes: current status of the research and future directions. School Ment. Health 6, 84–98. doi: 10.1007/s12310-013-9116-2
Suldo, S. M., and Huebner, E. S. (2004). Does life satisfaction moderate the effects of stressful life events on psychopathological behavior during adolescence? Sch. Psychol. Q. 19, 93–105. doi: 10.1521/scpq.19.2.93.33313
Terjesen, M. D., Jacofsky, M., Froh, J., and DiGiuseppe, R. (2004). Integrating positive psychology into schools: Implications for practice. Psychol. Sch. 41, 163–172. doi: 10.1002/pits.10148
Thakkar, J. J. (2020). Structural Equation Modelling. Application for Research and Practice (with AMOS and R). Singapore: Springer.
Tonci, E., De Domini, P., and Tomada, G. (2012). La misura della relazione alunno-insegnante: adattamento dello student-teacher relationship questionnaire secondo una prospettiva integrata [The measure of the pupil-teacher relationship: adaptation of the student-teacher relationship questionnaire] G . Ital. di Psicol. 39, 667–693. doi: 10.1421/38777
Torsheim, T., and Wold, B. (2001). School-related stress, support, and subjective health complaints among early adolescents: a multilevel approach. J. Adolesc. 24, 701–713. doi: 10.1006/jado.2001.0440
Twenge, J. M. (2020). Why increases in adolescent depression may be linked to the technological environment. Curr. Opin. Psychol. 32, 89–94. doi: 10.1016/j.copsyc.2019.06.036
Twenge, J., Joiner, T. E., Rogers, M. L., and Martin, G. N. (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among u.s. adolescents after 2010 and links to increased new media screen time. Clin. Psychol. Sci. 6, 3–17. doi: 10.1177/2167702617723376
Valdez, C. R., Lambert, S. F., and Ialongo, N. S. (2011). Identifying patterns of early risk for mental health and academic problems in adolescence: A longitudinal study of urban youth. Child Psychiatry Hum. Dev. 42, 521–538. doi: 10.1007/s10578-011-0230-9
van der Ende, J., and Verhulst, F. C. (2005). Informant, gender and age differences in ratings of adolescent problem behaviour. Eur. Child Adolesc. Psychiatry 14, 117–126. doi: 10.1007/s00787-005-0438-y
Veronese, G., Pepe, A., Alzaanin, W., and Shoman, H. (2020). Sources of functioning, symptoms of trauma, and psychological distress: A cross-sectional study with Palestinian health workers operating in West Bank and Gaza strip. Am. J. Orthopsychiatry 90, 751–759. doi: 10.1037/ort0000508
Vieno, A., Perkins, D. D., Smith, T. M., and Santinello, M. (2005). Democratic school climate and sense of community in school: A multilevel analysis. Am. J. Community Psychol. 36, 327–341. doi: 10.1007/s10464-005-8629-8
Wang, M., Brinkworth, M., and Eccles, J. (2013). Moderating effects of teacher-student relationship in adolescent trajectories of emotional and behavioral adjustment. Dev. Psychol. 49, 690–705. doi: 10.1037/a0027916
Weare, K., and Nind, M. (2011). Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot. Int. 26, i29–i69. doi: 10.1093/heapro/dar075
World Health Organization (2005). Promoting Mental Health: Concepts, Emerging Evidence, Practice. Geneva, Switzerland: Publications of the World Health Organization.
World Health Organization (2012). Risks to mental health: An overview of vulnerabilities and risk factors background paper by who secretariat for the development of a comprehensive mental health action plan . Available at: https://www.who.int/mental_health/mhgap/risks_to_mental_health_EN_27_08_12.pdf (Accessed April 23, 2021).
Yeo, L. S., Ang, R. P., Chong, W. H., and Huan, V. S. (2007). Gender differences in adolescent concerns and emotional well-being: perceptions of Singaporean adolescent students. J. Genet. Psychol. 168, 63–80. doi: 10.3200/GNTP.168.1.63-80
Zappulla, C., Pace, U., Lo Cascio, V., Guzzo, G., and Huebner, E. S. (2014). Factor structure and convergent validity of the long and abbreviated versions of the multidimensional students’ life satisfaction scale in an Italian sample. Soc. Indic. Res. 118, 57–69. doi: 10.1007/s11205-013-0418-4
Zullig, K. J., Valois, R. F., Huebner, E. S., and Drane, J. W. (2001). Relationship between perceived life satisfaction and adolescents’ substance abuse. J. Adolesc. Health 29, 279–288. doi: 10.1016/S1054-139X(01)00269-5
Keywords: school mental health, adolescence, life satisfaction, teacher-student relationship, school connectedness, structural equation modelling
Citation: Cavioni V, Grazzani I, Ornaghi V, Agliati A and Pepe A (2021) Adolescents’ Mental Health at School: The Mediating Role of Life Satisfaction. Front. Psychol . 12:720628. doi: 10.3389/fpsyg.2021.720628
Received: 07 June 2021; Accepted: 13 July 2021; Published: 18 August 2021.
Reviewed by:
Copyright © 2021 Cavioni, Grazzani, Ornaghi, Agliati and Pepe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valeria Cavioni, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Effects of the COVID-19 Pandemic on University Students' Mental Health: A Literature Review
Beatta zarowski, demetrios giokaris.
- Author information
- Article notes
- Copyright and License information
Olga Green [email protected]
Corresponding author.
Accepted 2024 Feb 11; Collection date 2024 Feb.
This is an open access article distributed under the terms of the Creative Commons Attribution License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This review aims to focus on the effects of COVID-19 on university students' mental health and deepen our understanding of it. The conclusions are based on the review of 32 studies conducted during the pandemic. This review confirms that university students were at high risk for mental health disorders, heightened stress, and increased sleep comorbidities both pre-pandemic and during the pandemic. This literature review confirmed a few universal trends, i.e., increased stress, anxiety, and depression, during the pandemic. The rates of insomnia, obsessive-compulsive disorder, and suicidal ideation also went up. Overall, female students are at a disadvantage in the development of mental health issues. Male students coped better but may be at higher risk for lethality in suicidal ideation. Students with a history of mental health issues and other comorbidities prior to the pandemic had worse outcomes compared to healthy individuals. The study points to a strong positive correlation between fear and increased rates of stress, anxiety, and insomnia. There is also a positive correlation between declining mental health and online learning. A strong negative correlation was present between physical activity and depressive symptoms. These findings are universal across many countries and regions where the studies occurred.
Keywords: suicidal ideation, depression, anxiety, stress, students, mental health, covid-19
Introduction and background
The COVID-19 pandemic began in March 2020 and profoundly impacted university students' mental, emotional, academic, social, and other aspects of life. Mid-pandemic studies [ 1 - 5 ] and pre-pandemic publications, including 2017 WHO mental health estimates, place university students at high risk for mental health dysfunction, with a higher prevalence of psychiatric morbidity compared to the general global population, with 4.4% for anxiety and 3.6% for depression [ 5 ]. Unexpected and sudden restrictions, isolation policies, and lockdowns in many countries were meant to protect communities and society at large but had a lot of unintended negative consequences. This review aims to present evidence of the disruptive trends uniquely amplified globally within the university student population and identified in the literature published in 2020-2023 on this topic. The review will analyze 32 peer-reviewed sources focusing on the pandemic's mental, psychological, academic, social, and other effects on university students.
Methodology
This literature review utilized several scientific literature databases, including Science Direct, Google Scholar, Web of Science, and PubMed, to identify articles that include the search criteria, such as those related to the prevalence of anxiety, stress, depression, obsessive-compulsive disorder (OCD), sleep disorders, and suicidal ideation and other symptoms in students in university settings. For cross-reference, the review includes topics identified in scientific literature across different geographical regions and comprises the most prevalent mental health issues. The sources originated from different countries, including the United States, Denmark, UK, Turkey, Saudi Arabia, Serbia, UAE, Italy, Jordan, India, Lebanon, Egypt, Germany, Bangladesh, Iraq, Switzerland, Canada, Australia, and China, offering an international viewpoint on the mental health impact of the pandemic on university students. Each article was published following a scientific peer-review process, ensuring the reliability and validity of the data presented.
Inclusion/exclusion criteria
Specific inclusion and exclusion criteria were put together to preserve focus and relevance. The review included only peer-reviewed literature published between January 2020 and December 2023. The timeframe included research completed during and after the COVID-19 pandemic. Only the publications written in English were studied for inclusion. Studies on the mental health issues and consequences of the COVID-19 epidemic on university students were included, while studies on other populations or unrelated issues were discarded. Inclusion and exclusion criteria are shown in Table 1 .
Table 1. Inclusion and exclusion criteria for the study.
Stress and anxiety
The WHO estimates that the most prevalent mental health disorder is anxiety, affecting up to 1/3 of adults in their lifetime [ 4 ]. Following the implementation of quarantines, lockdowns, and suspension of face-to-face teaching, universities and colleges switched to online remote learning modes. This sudden change altered students' functioning, primarily evidenced by increased stress and anxiety. The review demonstrated several trends directly resulting from the COVID-19 pandemic, such as fear of contamination, a rise in OCD, a decline in personal interactions, and long hours pursuing online learning. The review also identified several indirect stressors caused by COVID-19: financial hardships, decreased sleep quality, rise in pre-existing anxiety, depression, and stress. According to pre-pandemic data, direct and indirect stressors have contributed significantly to an overall spike in stress and anxiety. Female gender emerged as an additional factor for increased symptoms and comorbidities during COVID-19.
The most apparent stressor was the danger of contamination [ 3 , 6 - 10 ]. In the first few months of the pandemic, the university academic population in Turkey cited danger and fear of infection as the most significant stressors affecting their day-to-day lives [ 3 ]. American students echoed the same fear of infection among their family members and themselves [ 10 ]. Researchers concluded that prolonged exposure to fear positively correlated with increased anxiety [ 6 ]. The announcements of the pandemic often came with the government's policies of mandatory lockdowns to reduce the spread of COVID-19 infections. The restrictions considerably changed lifestyles and social relationships. For the first time in their lives, students experienced home quarantine. The research on increased stress and the adverse effects of at-home isolation was conducted during other pandemics and during COVID-19 [ 2 , 11 ]. The magnitude of the COVID-19 pandemic multiplied stress and other adverse effects and eliminated most of the social person-to-person interaction [ 2 , 12 , 13 ]. Researchers consistently show the harmful effects of social distancing and decreased social interactions during COVID-19 closures [ 10 ]. All those elements contributed to psychological dysfunction, increased stress, anxiety symptoms [ 14 ], and changes in sleeping patterns [ 15 , 16 ]. Other studies show a link between COVID-19-induced home isolation and changed sleep patterns [ 2 ], COVID-19 and stress, and poor academic performance [ 2 , 17 ].
Following announcements of public restrictions, colleges and universities rushed to implement online-only learning models [ 2 , 7 - 9 , 18 , 19 ]. Preventing academic loss and adopting digital learning allowed students to continue their education under home quarantine. Before the COVID-19 pandemic, Brooks et al. [ 11 ] analyzed the effects of home quarantine during other outbreaks. Brooks et al. hypothesize that education, when conducted under home quarantine, is a cause of increased frustration, stress, anger, and anxiety. The dominance of technology-driven college education associated with long online hours and possible internet addiction leads to a significant increase in anxiety levels [ 20 ]. The shift from in-person to digital education among university students contributed to increased anxiety prevalence [ 18 , 20 ]. A positive correlation between declining mental health and online learning was noted among Asian students, as observed by Islam et al. [ 21 ]. The constant fear, online presence, the enormous volume of information consumed, endless searches, and associated behaviors amplified anxiety and stress [ 8 , 22 ] and were a reason for the rise in anxiety [ 6 ] and were labeled as "cyberchondria" [ 7 ].
As the closures and lockdowns continued, students suffered financial hardships, causing anxiety [ 7 , 8 , 22 , 23 ]. College students reported adverse events such as declining family income, food and housing insecurity, and inadequate financial resources [ 23 ] to afford food, housing, and technology for effective learning. These indirect stressors disrupted the lives of low-income students more significantly and caused higher rates of stress and anxiety than those of high-income students [ 23 ]. Pandemic-generated unemployment caused working students to exhibit additional anxiety. Asian students were also reporting rising anxiety levels during the pandemic, particularly those who did not have access to resources [ 21 ], such as reliable internet, inability to purchase subscriptions, technology, or supplies, and who suffered from economic instability.
The long-term effects of the pandemic-related students' stress did not end with the first vaccination. This elevated stress trend continued for months after the initial impact [ 8 , 24 - 26 ], and even as of April 2021, 71% of Asian students were still reporting mild anxiety symptoms [ 26 ]. This finding contrasts with pre-pandemic anxiety levels recorded at about 15.7% and rising to 18.86% in March 2020 and to 32.68% in September 2020, respectively [ 26 ]. Al-Kumaim et al. [ 24 ] indicated that the pandemic had a considerable influence on students' psychological well-being, with anxiety being one of the most reported symptoms. The length of the pandemic hurt the mental health of university students. Students' anxiety levels continued at elevated levels. This observation is congruent with increased anxiety (60.8%) for students surveyed in 2021 [ 27 ]. The length of the pandemic was also detrimental to the deterioration of the mental health of the students.
Studies consistently found that female students were more at risk for increased anxiety during the pandemic. The research does not firmly establish why the female gender appears at significant risk for developing anxiety and increased stress [ 8 , 9 , 14 - 16 , 18 , 20 , 28 - 32 ]. This female factor could be due to the multifaceted nature of biological, psychosocial, cultural, and behavioral differences before and during the pandemic [ 29 ]. The exact calculations on how wide the gap is between male and female students' stress levels during the pandemic vary from paper to paper. The levels of pre-pandemic anxiety in female vs. male students were established in a Chinese longitudinal study showing anxiety for female students at 22%, while male students scored at 19% [ 29 ]. The study of students in Turkey [ 3 ] mid-COVID-19 demonstrates that the trend continues at almost twice the rate of anxiety, with 63% in females vs. 36% in male students. A systemic review by Liyanage et al. [ 4 ] quotes global differences in stress and anxiety for university students with mid-pandemic symptoms at 43% for females and 39% for males.
Several scholarly papers discuss the presence of a few well-established protective factors that reduce the levels of stress and anxiety experienced by students during the pandemic. The researchers zeroed in on the male gender [ 9 , 29 - 31 , 33 ], the presence of physical health [ 31 ], participation in exercise [ 34 ], student seniority, and urban residence [ 12 ]. Pre and mid-pandemic literature suggests that male students have shown consistently lower stress and anxiety symptoms than their female counterparts. This review shows strong mid-pandemic consistency for gender differences across many authors [ 3 , 6 - 9 , 13 , 28 , 29 , 31 , 32 ]. The articles reviewed do not explain why the male gender appears less affected by mental health challenges during the pandemic.
Academic stress is a part of a typical student learning cycle. Students who had senior student status experienced less stress [ 16 , 28 , 32 ]. Wang et al. [ 33 ] confirmed that increased stress and anxiety are more prevalent in junior student populations. The differences between the junior and senior students can be explained by older age, more independence, and autonomy contributing to frustrations. Undergraduate students need time to develop psychological and emotional skills to handle stress better [ 33 ].
Families of students residing in rural areas are more vulnerable to socioeconomic downturn. Rural areas experience higher rates of poverty, and students tend to be poorer than their urban colleagues who reside in urban settings [ 8 , 12 , 33 ]. Living in an urban setting with more access to resources, including high-speed internet, protects students from developing higher stress and anxiety levels [ 12 ]. Students who returned home and lived with supportive family members also reported decreased stress and anxiety levels compared to students who lived alone [ 8 , 12 ]. Students who lived with families had lower anxiety levels. Living with supportive parents had a protective effect on rising anxiety levels [ 12 ].
The extensive use of home confinement and prolonged self-quarantine began the COVID-19 pandemic. The disruption of students' daily regimens and increasing lack of physical health resulted in decreased motivation and academic/social involvement [ 31 ]. Xiang et al. [ 34 ] describe the relationship between anxiety levels among Chinese students who engaged in consistent physical activity during the pandemic vs. inactive students. Physically active students experienced better mental health [ 27 , 34 ]. Exercise stimulates endorphin production. Students who exercised regularly experienced decreased stress levels compared to non-active students [ 27 , 34 ]. Regular physical activity is a protective factor against increased anxiety levels. Pandemic time research showed an inverse association between resistance training and anxiety levels [ 34 ].
Together, these studies confirm the negative impact of the COVID-19 crisis on mental health, especially concerning anxiety and stress. Considering the challenges associated with the transition to adulthood, university students are particularly vulnerable to mental health problems.
Very few sources compare rates of depression pre- and post-pandemic. The studies that capture this information come from the United Arab Emirates (UAE) [ 28 ] and China [ 2 ]. They indicate the pre-pandemic level of depressive symptoms at 22% in UAE [ 28 ] and 16.9% [ 2 ] in China and post-pandemic depressive symptoms at 40% and 30.6%, respectively. The authors of both studies suggest that the rates of depression during the COVID-19 pandemic almost doubled. They link the increased rates of depression to family stress [ 2 ] and academic demands. High rates of depression at 64% among university medical students who lived with family during COVID-19 are also echoed by Serbian researchers [ 32 ]. Increased rates of depression in the student population, as compared to other age groups, before the pandemic continued the same trend post-pandemic [ 1 ].
Chinese university students who participated in the research were 18 to 24 years old [ 1 ]. This "post-adolescent" period [ 1 ] is one of the most challenging periods in life, characterized by difficulties managing emotions and inadequate capabilities and skills to manage psychological and academic needs. Research conducted during similar periods of confinement [ 2 ] shows that students, when in prolonged home isolation, are a vulnerable population to increased stress, anxiety, and, ultimately, depression. The studies on Jordanian students [ 2 ] link home confinement to COVID-19-related issues, including increased stress, anxiety, sleep and eating disturbances, feelings of loneliness, dissatisfaction with distance learning, and the presence of home quarantine as a possible precursor to the pandemic time increase in depression. Fawaz et al. [ 18 ] show a significant positive correlation between students' dissatisfaction and depressive symptoms. The analysis of the source of UK-based doctoral students' study [ 35 ] lists pre-existing cumulative stress, pre-pandemic depression, and anxiety as possible reasons for developing six times higher than the general population's depression tendencies, reporting clinical levels of depressive and anxiety symptoms at 28.3% and 79.4%, respectively. Researchers show a direct relationship between the COVID-19 home quarantine period and an increase in mental health difficulties represented by the following findings: 78% depression, 67.9% anxiety, and 58.7% stress [ 2 ].
Other studies show that during the COVID-19 pandemic, students feared and suffered academic decline [ 2 , 18 , 23 , 26 , 28 , 31 ]. The decrease in students' satisfaction during COVID-19 inherently influenced the increased prevalence of depressive symptoms [ 18 , 26 ]. Factors such as the perception of an overwhelming school workload also contributed to the increase in depressive symptoms [ 18 , 28 ]. Study participants felt overwhelmed by too many online tasks [ 18 , 24 ]. Students who are depressed are more likely to avoid classes, tests, and assignments [ 1 ], causing a slide to poor academic performance. Fawaz et al. [ 18 ] discovered an association between an abrupt shift to e-learning and an increase in perceived increase in workload that also produced depression symptoms.
Increasing depression during the COVID-19 pandemic was exacerbated among the students with feelings of loneliness and isolation [ 2 , 7 , 13 , 27 ]. Wang et al. [ 33 ] concluded that epidemic-related factors, such as the impact of isolation, increased anxiety, and fear of contagion, are associated with higher risk of depressive symptoms. Additional factors contributing to the increase in depressive symptoms include a family history of chronic illness [ 2 , 12 ].
Researchers show an increased prevalence of depressive symptoms in female students [ 2 , 29 ]. A Serbian study of university students [ 32 ] puts the rate of increased depression of female students at almost 2.5 times higher than men. Mirilovic et al. [ 32 ] also show more severe rates of depressive symptoms among junior first and second-year students as compared to senior students.
Despite many issues contributing to an increase in depressive symptoms, Xiang et al. [ 34 ] point to specific forms of physical activity, such as stretching and resistance training, which were negatively correlated with both anxiety and depression. Participating in house chores was negatively correlated with depression.
Quoted studies provide evidence of overall increased depressive symptoms in the university student population during the COVID-19 pandemic. The researchers point to several factors that play a role in the increased depression prevalence pre-pandemic baseline and increased mid-pandemic levels compared to the general population. This finding is a specific aspect of the mental health picture of the university student population.
Obsessive-compulsive disorder (OCD)
OCD is a chronic psychiatric disorder characterized by unwanted thoughts and repetitive behaviors. The global prevalence is at about 2.3% [ 36 ]. During the COVID-19 pandemic, government recommendations for increased handwashing efforts and other preventative measures provided a cognitive justification for excessive compulsion to take a firm root and spread [ 17 , 37 , 38 ]. Those prevention tools became a direct trigger and stressor for about 3.8% of medical students who struggled with OCD symptoms before the pandemic [ 36 ]. Medical students exhibit increased prevalence because the onset and peak of OCD happen in late teens and early adulthood. The average onset is 19-20 years old [ 21 ]. Munk et al. [ 38 ], in a German study, listed an increase in OCD symptoms from 3.6% before the pandemic to 21.4% in March 2020 in the general population. In late 2021, researchers in Iraq pointed to OCD symptoms in about 43% of surveyed university subjects [ 37 ], demonstrating a massive increase with symptoms spread as follows: unpleasant thoughts (58.1%), washing (14%), contamination scales (19.4%), and repetition of numbers (8%). These symptoms seem to affect the younger students more and the students in earlier years of study [ 37 ]. In addition, Zheng et al. [ 19 ] identified in their research that just becoming a student puts university students at 2.169 times the increased risk of having an OCD diagnosis compared to healthcare workers. Other variables as predictors for OCD in the general population may also apply to university students: being single places people at 1.836 times increased risk of having OCD, the presence of an increase in sleep latency is an independent predictor for OCD, and a history of psychiatric comorbidity. Mazhar et al. [ 39 ] observed that female medical students in junior preclinical years are more likely to suffer symptoms of OCD at increased rates in contrast to male students. Fears, depression, eating disorders, and other stress-inducing factors had a magnifying effect that contributed to increased OCD prevalence in students during the pandemic [ 37 ].
Suicidal ideation
Suicide claims over 800,000 lives every year worldwide [ 40 ], with more than half occurring before the age of 50. The estimated global mortality rate is about 16/100,000, with males at over four times the rate of females. It is the second leading cause of death among 10 to 34-year-old adults, according to the Centers for Disease Control and Prevention (CDC) [ 40 ]. Multiple authors talk about experiences of increased suicidal ideation among university students during the COVID-19 pandemic [ 16 , 30 , 41 , 42 ]. A study of younger students conducted before the COVID-19 pandemic by Lewinsohn et al. [ 43 ] found that female adolescents are at significantly higher risk of suicide attempts compared to male counterparts. The differences between genders diminished as participants increased with age. Gender was found to predict the lethality in suicide attempts as more males than females made attempts with high perceived lethality and medical lethality [ 43 ]. The study on Chinese university students during the COVID-19 pandemic [ 42 ] points to the male gender as well as a risk factor for increased suicidal ideation along with other factors like anxiety and depressive symptoms. Becoming a senior student decreases the risk of suicidal ideation [ 42 ].
A comparison between male and female students demonstrated that suicidal ideation is more prevalent among students with heightened depression and anxiety levels [ 30 , 41 , 42 ]. The pandemic disrupted daily structures and sleep-wake cycles. An increase in suicidal ideation was linked by AlHadi et al. [ 16 ] to students with insomnia symptoms. AlHadi et al. [ 16 ] suggest that insomnia could be the "mediator" between COVID-19 anxiety and suicide. They demonstrate a direct link between increased insomnia levels and an increase in suicidal thoughts [ 16 ]. Building on the analysis presented by Lewinsohn et al. [ 43 ], the research on Saudi students also finds junior female students have more experiences with an increased prevalence of suicidal thoughts. The theme of mental and medical health issues before the pandemic as a risk factor for developing suicidal ideation before and during the pandemic was brought up consistently as a risk factor for greater prevalence of suicidal ideation [ 30 , 40 - 44 ]. Scientists from multiple sources quoted by the CDC point out that at any age, suicidal behavior is a complex process. Experts agree that a single event does not cause suicide. It involves various risk factors, such as individual, relationships, community, and societal levels [ 40 ]. During the COVID-19 pandemic, university students were experiencing pressures and stress involving all aspects of life, increasing the possibility of the development of suicidal ideation, and advancing from ideation to suicidal attempts and suicide completion [ 40 , 42 , 44 ].
Canadian researchers [ 41 ] demonstrated that university students also remained vulnerable to the increased risk of developing suicidal ideation when additional risk factors were present: identifying as Chinese or as another ethnic minority, experiencing depression or anxiety, having a history of suicidal planning or attempts, and being overwhelmed but unable to get help [ 4 ].
The COVID-19 pandemic triggered an increase in uncertainty and fear. The elevated prevalence of suicidal ideation and other psychiatric disorders coincided with anti-pandemic measures such as lockdowns, social isolation, heightened levels of stress and psychological strain, and other factors beyond this review.
Sleeping disorders and insomnia
Most authors agree that sleeping disorders among university students have worsened during the COVID-19 pandemic, with increased stress and anxiety playing a significant role in sleep disruptions [ 8 , 10 , 14 - 16 , 19 , 20 , 45 , 46 ]. Students' negative perceptions during the COVID-19 pandemic were also reflected in decreased sleep quality [ 8 , 15 , 46 ]. The combination of social restrictions, physical isolation, and stress of distance learning resulted in interrupted sleep and wake cycles [ 8 , 15 , 20 , 22 ]. Over 52% of the students reported difficulties falling asleep and 43% reported not getting enough sleep with self-reported stress and anxiety in 78% of the student population [ 46 ], causing declining mental health [ 25 ].
Pre-COVID-19 sleep disorders increased their prevalence during the COVID-19 pandemic [ 15 , 46 ]. Dongol et al. analyzed data from smartwatches and surveys to measure sleep duration and light and deep sleep, and demonstrated that almost 80% of the students were found to be experiencing high-level sleeping disturbance; most significantly, about 27% of males and 33% of females had clinical insomnia [ 15 ]. These findings are in sharp contrast to insomnia presence before the pandemic at 9.5% [ 47 ]. The authors offer a list of predisposing factors that included the following: female gender, chronic health issues, being an older student, sleep disorder before the COVID-19 pandemic, increased caffeine consumption, and changes in daily routines that include sleeping patterns [ 15 ]. Dongol et al. attributed increased stress, poor sleep quality, and fear during COVID-19 to the elevated presence of clinical insomnia symptoms. On the other hand, the conclusion of the Italian study [ 14 ] discusses how the lockdowns affected the students' psycho-emotional well-being, changes in sleep patterns, and heightened insomnia rates from 15% before COVID-19 to 42% during the pandemic. Students identified different aspects associated with this difficulty: 52% reported increased problems falling asleep, 43% were not getting enough sleep, and almost 70% reported various disturbances ranging from having vivid dreams and not having a fixed sleep schedule to overwhelming stress and anxiety [ 14 ].
The fear of contracting COVID-19 has been found to correlate with heightened stress levels, clinical insomnia, and diminished sleep quality [ 10 , 15 ]. Pre-pandemic studies link insomnia in college students to poor academic performance [ 45 ]. Mid-pandemic research by Son et al. [ 10 ] suggested insomnia contributes to difficulties with concentration.
There has been a notable rise in the prevalence of insomnia, a decline in sleep quality, and elevated stress levels among college students, regardless of country of origin. This increased prevalence is particularly pronounced among female students [ 14 , 20 ], older students, and those with chronic illnesses and pre-existing sleep disorders [ 15 , 16 ].
Research gaps
This review addresses only college students as they are a particular population with many challenges. The scholarly papers examined the mental health difficulties, stressors, sleeping difficulties, selected psychiatric prevalence, coping methods, and potential short-term psychological impacts of the pandemic on higher education students. This review identifies opportunities for further research in this area by identifying gaps in existing literature.
More research should be conducted on the psychological influence of the coronavirus pandemic on university students with different backgrounds. The studies presented in this paper originated from the West, China, India, and a few Middle Eastern countries. It is essential to recognize how this pandemic has affected individuals from different backgrounds and how many factors may have influenced their experiences. Most studies have primarily focused on a narrow range of short-term effects. It is crucial to consider the wide-ranging consequences and lasting impact. Further research is necessary to fully comprehend the long-term mental health implications of the pandemic on university students.
Additionally, more research is needed to determine the most effective interventions/solutions for supporting university students continuously. Although most studies have primarily examined the adverse psychological effects, data are available on protective factors that can assist institutions and students. The research on the role of resilience and protective factors could provide helpful and practical information when facing COVID-19 or any other adverse event. This type of research allows the universities' governing bodies and administrators to comprehend students' mental health struggles and create effective strategies to support student well-being when facing personal, national, or global disasters such as COVID-19.
Future directions
To manage mental health needs during future outbreaks of COVID-19 or other pandemics, measurable, science-based, uniform intervention and support for university students are required. Most support should be deployed on a smaller scale and within the academic community to support individual students' needs. These services can be expanded and scaled up as needed during times of need. The literature suggests different models of examination of the interventional landscape [ 24 ]: (1) screenings and education: institutional and community-level regular screenings, broad education with outreach and follow-up, and access to tailored interventions and information for at-risk individuals. (2) Personal development: opportunities to examine and improve self-determination, self-efficacy, self-regulation, and other qualities [ 24 ]. Research out of Germany brings up a somewhat elusive concept of resilience [ 31 ] linked to a perception of control, a positive development that allows students to flourish under pressure and strengthen personal bonds. Researchers believe [ 31 ] that academic success is reinforced by the notion of "belonging" as a protective factor for mental health. Based on these findings, incorporating the teaching of resilience could become a valuable tool for university students. (3) Technical fluency: ongoing training and exposure to new technologies, digital fluency, mobile interactive learning, and intuitive design of online learning experiences [ 24 ]. (4) Environmental support: this area includes a broad category of socioeconomic factors like family support, university support, and emotional engagement [ 23 , 24 ]. Each category has its variables, and students' well-being depends on the sum of improvements in all four areas.
Finally, implementing a structured program of longitudinal studies to capture and measure the adequate representation of the mental health status of university students is the preferred practice in higher educational settings [ 4 ]. Taking a continuous pulse of the students' mental health through regular health screenings and hopefully accessible intervention seems like a logical solution. As those new interventions, studies, and programs are instituted, we need to measure what is changing and what is effective [ 25 ].
Recommendations
The COVID-19 pandemic caused school and university closures and changes in daily schedules, teaching methods, and other aspects of daily life. These changes dramatically impacted university students and highly affected young adults, leading to many mental health trends discussed above. The disadvantaged factors emerge among different student profiles analyzed: social isolation, female, history of comorbidities, poor, and rural background. The advantage factors were good health, male gender, resilience, supportive family and plenty of social connections, affluent urban background, and regular physical activity. The pandemic has intensified the significant increase in the number and type of disorders across the mental health spectrum and the rapid emergence of psychiatric conditions. This review finds that the COVID-19 pandemic negatively affected the mental health of university students, and the following trends have been identified: (1) decreased mental health: these psychological trends include increased stress, anxiety, self-reported decreased well-being, constant worry, etc. [ 1 , 3 , 4 , 6 , 9 , 10 , 12 - 23 , 26 - 28 , 30 , 31 , 33 , 34 , 46 ]; (2) psychiatric trends include the presence of depression, substance abuse, and increased psychiatric morbidity, including an increase in OCD occurrence as well as suicidal ideation [ 1 , 16 - 19 , 23 , 24 , 26 , 28 , 30 - 37 , 39 , 41 , 42 , 48 ]; (3) disruption of the circadian cycle trends, sleep disorders, and insomnia [ 10 , 14 - 16 , 19 , 20 , 46 ]; (4) the disproportional detrimental effect of COVID-19 on female students in all areas reviewed [ 3 , 6 , 9 , 13 - 16 , 20 , 28 - 31 ].
Conclusions
The COVID-19 pandemic is the most significant public health threat to generational mental health. Anxiety and stress were cited as the most prevalent conditions among the student population during the COVID-19 pandemic. Higher education institutions and governments were reactive in their response to the COVID-19 pandemic. Young intellectuals suffered at increased rates from stress, anxiety, sleep-related issues, depression, and suicidal ideation. A firm action to protect the students' safety and physical, social, and mental well-being must be taken in partnership with their communities, students, and higher education institutions.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Beatta Zarowski, Demetrios Giokaris, Olga Green
Acquisition, analysis, or interpretation of data: Beatta Zarowski, Demetrios Giokaris, Olga Green
Drafting of the manuscript: Beatta Zarowski, Demetrios Giokaris, Olga Green
Critical review of the manuscript for important intellectual content: Beatta Zarowski, Demetrios Giokaris, Olga Green
Supervision: Demetrios Giokaris
- 1. COVID-19: a source of stress and depression among university students and poor academic performance. Jiang Z, Jia X, Tao R, Dördüncü H. https://doi.org/10.3389/fpubh.2022.898556 . Front Public Health. 2022;10:898556. doi: 10.3389/fpubh.2022.898556. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Depression, anxiety and stress among undergraduate students during COVID-19 outbreak and "home-quarantine". Hamaideh SH, Al-Modallal H, Tanash M, Hamdan-Mansour A. https://doi.org/10.1002/nop2.918 . Nurs Open. 2022;9:1423–1431. doi: 10.1002/nop2.918. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Anxiety and stress levels associated with COVID-19 pandemic of university students in Turkey: a year after the pandemic. Durbas A, Karaman H, Solman CH, Kaygisiz N, Ersoy Ö. Front Psychiatry. 2021;12:731348. doi: 10.3389/fpsyt.2021.731348. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Prevalence of anxiety in university students during the COVID-19 pandemic: a systematic review. Liyanage S, Saqib K, Khan AF, et al. Int J Environ Res Public Health. 2021;22:62. doi: 10.3390/ijerph19010062. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Geneva, Switzerland: Estimates; World Health Organization; 2017. World Health Organization. Depression and other common mental disorders: global health. [ Google Scholar ]
- 6. Impact on mental health of students due to restriction caused by COVID-19 pandemic: cross-sectional study. [PREPRINT] Chaudhary AP, Sonar NS, Jamuna TR, Banerjee M, Yadav S. medRxiv. 2021 doi: 10.2196/28158. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Psychosocial effects of isolation and fear of contagion of COVID-19 on the mental health of different population groups. Richaud MC, Muzio RN, Lemos V, Urquijo S, Carlo G. Front Psychol. 2022;13:1011028. doi: 10.3389/fpsyg.2022.1011028. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Effect of COVID-19 outbreak on anxiety among students of higher education; a review of literature. Jehi T, Khan R, Dos Santos H, Majzoub N. Curr Psychol. 2022;42:17475–17489. doi: 10.1007/s12144-021-02587-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Anxiety and fear of COVID-19 among nursing students during the COVID-19 pandemic: a descriptive correlation study. Kuru Alici N, Ozturk Copur E. Perspect Psychiatr Care. 2022;58:141–148. doi: 10.1111/ppc.12851. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. Son C, Hegde S, Smith A, Wang X, Sasangohar F. J Med Internet Res. 2020;22:0. doi: 10.2196/21279. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. The psychological impact of the COVID-19 epidemic on college students in China. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Students under lockdown: comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. Elmer T, Mepham K, Stadtfeld C. PLoS One. 2020;15:0. doi: 10.1371/journal.pone.0236337. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Marelli S, Castelnuovo A, Somma A, et al. J Neurol. 2021;268:8–15. doi: 10.1007/s00415-020-10056-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Sleep quality, stress level and COVID-19 in university students; the forgotten dimension. Dongol E, Shaker K, Abbas A, et al. Sleep Sci. 2022;15:347–310. doi: 10.5935/1984-0063.20210011. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Insomnia prevalence and associated factors among university students in Saudi Arabia during the COVID-19 pandemic and lockdown: a large-scale survey. AlHadi AN, Alhuwaydi AM. Nat Sci Sleep. 2022;14:1651–1663. doi: 10.2147/NSS.S380972. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Obsessive-compulsive disorder during the COVID-19 pandemic—a systematic review. Linde ES, Varga TV, Clotworthy A. Front Psychiatry. 2022;13:806872. doi: 10.3389/fpsyt.2022.806872. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. E-learning: depression, anxiety, and stress symptomatology among Lebanese university students during COVID-19 quarantine. Fawaz M, Samaha A. Nurs Forum. 2021;56:52–57. doi: 10.1111/nuf.12521. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Prevalence and characteristics of obsessive-compulsive disorder among urban residents in Wuhan during the stage of regular control of coronavirus disease-19 epidemic. Zheng Y, Xiao L, Xie Y, Wang H, Wang G. Front Psychiatry. 2020;11:594167. doi: 10.3389/fpsyt.2020.594167. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Impact of internet addiction during COVID-19 on anxiety and sleep quality among college students of Bhubaneswar city. Kumar G, Dash P, Jnaneswar A, Suresan V, Jha K, Ghosal S. J Educ Health Promot. 2022;11:156. doi: 10.4103/jehp.jehp_396_21. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. Islam MA, Barna SD, Raihan H, Khan MN, Hossain MT. PLoS One. 2020;15:0. doi: 10.1371/journal.pone.0238162. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. A survey of attitudes, anxiety status, and protective behaviors of the university students during the COVID-19 outbreak in Turkey. Akdeniz G, Kavakci M, Gozugok M, Yalcinkaya S, Kucukay A, Sahutogullari B. Front Psychiatry. 2020;11:695. doi: 10.3389/fpsyt.2020.00695. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Disparities in college students’ financial hardships during the COVID-19 pandemic. Soria KM, Horgos B, Shenouda JD. J Student Aff Res Pract. 2023;60:31–48. [ Google Scholar ]
- 24. Exploring the impact of the COVID-19 pandemic on university students' learning life: an integrated conceptual motivational model for sustainable and healthy online learning. Al-Kumaim NH, Alhazmi AK, Mohammed F, Gazem NA, Shabbir MS, Fazea Y. Sustainability. 2021;13:2546. [ Google Scholar ]
- 25. Editorial: COVID-19: mid- and long-term educational and psychological consequences for students and educators. Alvarez-Alonso MJ, Scott R, Morales-Muñoz I. Front Psychol. 2022;13:903022. doi: 10.3389/fpsyg.2022.903022. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Psychological responses during the COVID-19 outbreak among university students in Bangladesh. Islam MS, Sujan MS, Tasnim R, Sikder MT, Potenza MN, van Os J. PLoS One. 2020;15:0. doi: 10.1371/journal.pone.0245083. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Impact of COVID-19 on the mental health of US college students. Lee J, Solomon M, Stead T, Kwon B, Ganti L. BMC Psychol. 2021;9:95. doi: 10.1186/s40359-021-00598-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Impact of COVID-19 pandemic on the mental health of university students in the United Arab Emirates: a cross-sectional study. Vajpeyi Misra A, Mamdouh HM, Dani A, Mitchell V, Hussain HY, Ibrahim GM, Alnakhi WK. BMC Psychol. 2022;10:312. doi: 10.1186/s40359-022-00986-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. Gao W, Ping S, Liu X. J Affect Disord. 2020;263:292–300. doi: 10.1016/j.jad.2019.11.121. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Depression, anxiety, and suicidal ideation in Chinese university students during the COVID-19 pandemic. Zhou SJ, Wang LL, Qi M, et al. Front Psychol. 2021;12:669833. doi: 10.3389/fpsyg.2021.669833. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Effects of the COVID-19 pandemic on university students' physical health, mental health and learning, a cross-sectional study including 917 students from eight universities in Germany. Gewalt SC, Berger S, Krisam R, Breuer M. PLoS One. 2022;17:0. doi: 10.1371/journal.pone.0273928. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. The impact of the COVID-19 epidemic on students' mental health: a cross-sectional study. Mirilović N, Janković J, Latas M. PLoS One. 2022;17:0. doi: 10.1371/journal.pone.0275167. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. Wang ZH, Yang HL, Yang YQ, et al. J Affect Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Relationship of physical activity with anxiety and depression symptoms in Chinese college students during the COVID-19 outbreak. Xiang MQ, Tan XM, Sun J, et al. Front Psychol. 2020;11:582436. doi: 10.3389/fpsyg.2020.582436. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. The effects of cumulative stressful educational events on the mental health of doctoral students during the COVID-19 pandemic. [ Aug; 2024 ];Sideropoulos V, Midouhas E, Kokosi T, Brinkert J, Wong KK, Kambouri MA. UCL Open Environ. 2022 4:0. doi: 10.14324/111.444/ucloe.000048. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Obsessive-compulsive symptoms in medical students: prevalence, severity, and correlates. Torres AR, Cruz BL, Vicentini HC, Lima MC, Ramos-Cerqueira AT. https://link.springer.com/article/10.1007/s40596-015-0357-2 . Acad Psychiatry. 2016;40:46–54. doi: 10.1007/s40596-015-0357-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Prevalence of obsessive-compulsive disorder (OCD) among Iraqi undergraduate medical students in time of COVID-19 pandemic. Taher TM, Al-fadhul SA, Abutiheen AA, Ghazi HF, Abood NS. Middle East Curr Psychiatry. 2021;28:8. [ Google Scholar ]
- 38. Covid-19-Beyond virology: potentials for maintaining mental health during lockdown. Munk AJ, Schmidt NM, Alexander N, Henkel K, Hennig J. PLoS One. 2020;15:0. doi: 10.1371/journal.pone.0236688. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Association of COVID 19 pandemic with new onset obsessive-compulsive disorder (OCD) symptomology in the medical students - a cross sectional study. Mazhar K, Khaliq F, Arshad D. BJPsych Open. 2021;7:0. [ Google Scholar ]
- 40. CDC. Facts about suicide. 2023. https://www.cdc.gov/suicide/facts/index.html https://www.cdc.gov/suicide/facts/index.html
- 41. Suicidal ideation amongst university students during the COVID-19 pandemic: time trends and risk factors. Jones LB, Vereschagin M, Wang AY, et al. Can J Psychiatry. 2023;68:531–546. doi: 10.1177/07067437221140375. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Prevalence and associated factors of suicidal ideation among college students during the COVID-19 pandemic in China: a 3-wave repeated survey. Liang SW, Liu LL, Peng XD, et al. BMC Psychiatry. 2022;22:336. doi: 10.1186/s12888-022-03968-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Gender differences in suicide attempts from adolescence to young adulthood. Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. J Am Acad Child Adolesc Psychiatry. 2001;40:427–434. doi: 10.1097/00004583-200104000-00011. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Lim KS, Wong CH, McIntyre RS, et al. Int J Environ Res Public Health. 2019;16:4581. doi: 10.3390/ijerph16224581. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Sleep complaints affecting school performance at different educational levels. Pagel JF, Kwiatkowski CF. Front Neurol. 2010;1:125. doi: 10.3389/fneur.2010.00125. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Intra-individual impact of the COVID-19 pandemic on mental health and sleep in young adults. Knickerbocker KJ, Cox EA, Dhawka L, Woods K, Ingram KK. https://doi.org/10.1371/journal.pone.0276165 . PLoS One. 2022;17:0. doi: 10.1371/journal.pone.0276165. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Epidemiology of insomnia in college students: relationship with mental health, quality of life, and substance use difficulties. Taylor DJ, Bramoweth AD, Grieser EA, Tatum JI, Roane BM. Behav Ther. 2013;44:339–348. doi: 10.1016/j.beth.2012.12.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Editorial: the consequences of COVID-19 on the mental well-being of parents, children and adolescents. Sorbring E, Svensson Y, Erlandsson SI, Deater-Deckard K. Front Psychiatry. 2022;13:924599. doi: 10.3389/fpsyt.2022.924599. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (177.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Open access
- Published: 20 September 2022
Factors that influence mental health of university and college students in the UK: a systematic review
- Fiona Campbell 1 ,
- Lindsay Blank 1 ,
- Anna Cantrell 1 ,
- Susan Baxter 1 ,
- Christopher Blackmore 1 ,
- Jan Dixon 1 &
- Elizabeth Goyder 1
BMC Public Health volume 22 , Article number: 1778 ( 2022 ) Cite this article
133k Accesses
90 Citations
98 Altmetric
Metrics details
Worsening mental health of students in higher education is a public policy concern and the impact of measures to reduce transmission of COVID-19 has heightened awareness of this issue. Preventing poor mental health and supporting positive mental wellbeing needs to be based on an evidence informed understanding what factors influence the mental health of students.
To identify factors associated with mental health of students in higher education.
We undertook a systematic review of observational studies that measured factors associated with student mental wellbeing and poor mental health. Extensive searches were undertaken across five databases. We included studies undertaken in the UK and published within the last decade (2010–2020). Due to heterogeneity of factors, and diversity of outcomes used to measure wellbeing and poor mental health the findings were analysed and described narratively.
We included 31 studies, most of which were cross sectional in design. Those factors most strongly and consistently associated with increased risk of developing poor mental health included students with experiences of trauma in childhood, those that identify as LGBTQ and students with autism. Factors that promote wellbeing include developing strong and supportive social networks. Students who are prepared and able to adjust to the changes that moving into higher education presents also experience better mental health. Some behaviours that are associated with poor mental health include lack of engagement both with learning and leisure activities and poor mental health literacy.
Improved knowledge of factors associated with poor mental health and also those that increase mental wellbeing can provide a foundation for designing strategies and specific interventions that can prevent poor mental health and ensuring targeted support is available for students at increased risk.
Peer Review reports
Poor mental health of students in further and higher education is an increasing concern for public health and policy [ 1 , 2 , 3 , 4 ]. A 2020 Insight Network survey of students from 10 universities suggests that “1 in 5 students has a current mental health diagnosis” and that “almost half have experienced a serious psychological issue for which they felt they needed professional help”—an increase from 1 in 3 in the same survey conducted in 2018 [ 5 ]. A review of 105 Further Education (FE) colleges in England found that over a three-year period, 85% of colleges reported an increase in mental health difficulties [ 1 ]. Depression and anxiety were both prevalent and widespread in students; all colleges reported students experiencing depression and 99% reported students experiencing severe anxiety [ 5 , 6 ]. A UK cohort study found that levels of psychological distress increase on entering university [ 7 ], and recent evidence suggests that the prevalence of mental health problems among university students, including self-harm and suicide, is rising, [ 3 , 4 ] with increases in demand for services to support student mental health and reports of some universities finding a doubling of the number of students accessing support [ 8 ]. These common mental health difficulties clearly present considerable threat to the mental health and wellbeing of students but their impact also has educational, social and economic consequences such as academic underperformance and increased risk of dropping out of university [ 9 , 10 ].
Policy changes may have had an influence on the student experience, and on the levels of mental health problems seen in the student population; the biggest change has arguably been the move to widen higher education participation and to enable a more diverse demographic to access University education. The trend for widening participation has been continually rising since the late 1960s [ 11 ] but gained impetus in the 2000s through the work of the Higher Education Funding Council for England (HEFCE). Macaskill (2013) [ 12 ] suggests that the increased access to higher education will have resulted in more students attending university from minority groups and less affluent backgrounds, meaning that more students may be vulnerable to mental health problems, and these students may also experience greater challenges in making the transition to higher education.
Another significant change has been the introduction of tuition fees in 1998, which required students to self fund up to £1,000 per academic year. Since then, tuition fees have increased significantly for many students. With the abolition of maintenance grants, around 96% of government support for students now comes in the form of student loans [ 13 ]. It is estimated that in 2017, UK students were graduating with average debts of £50,000, and this figure was even higher for the poorest students [ 13 ]. There is a clear association between a student’s mental health and financial well-being [ 14 ], with “increased financial concern being consistently associated with worse health” [ 15 ].
The extent to which the increase in poor mental health is also being seen amongst non-students of a similar age is not well understood and warrants further study. However, the increase in poor mental health specifically within students in higher education highlights a need to understand what the risk factors are and what might be done within these settings to ensure young people are learning and developing and transitioning into adulthood in environments that promote mental wellbeing.
Commencing higher education represents a key transition point in a young person’s life. It is a stage often accompanied by significant change combined with high expectations of high expectations from students of what university life will be like, and also high expectations from themselves and others around their own academic performance. Relevant factors include moving away from home, learning to live independently, developing new social networks, adjusting to new ways of learning, and now also dealing with the additional greater financial burdens that students now face.
The recent global COVID-19 pandemic has had considerable impact on mental health across society, and there is concern that younger people (ages 18–25) have been particularly affected. Data from Canada [ 16 ] indicate that among survey respondents, “almost two-thirds (64%) of those aged 15 to 24 reported a negative impact on their mental health, while just over one-third (35%) of those aged 65 and older reported a negative impact on their mental health since physical distancing began” (ibid, p.4). This suggests that older adults are more prepared for the kind of social isolation which has been brought about through the response to COVID-19, whereas young adults have found this more difficult to cope with. UK data from the National Union of Students reports that for over half of UK students, their mental health is worse than before the pandemic [ 17 ]. Before COVID-19, students were already reporting increasing levels of mental health problems [ 2 ], but the COVID-19 pandemic has added a layer of “chronic and unpredictable” stress, creating the perfect conditions for a mental health crisis [ 18 ]. An example of this is the referrals (both urgent and routine) of young people with eating disorders for treatment in the NHS which almost doubled in number from 2019 to 2020 [ 19 ]. The travel restrictions enforced during the pandemic have also impacted on student mental health, particularly for international students who may have been unable to commence studies or go home to see friends and family during holidays [ 20 ].
With the increasing awareness and concern in the higher education sector and national bodies regarding student mental health has come increasing focus on how to respond. Various guidelines and best practice have been developed, e.g. ‘Degrees of Disturbance’ [ 21 ], ‘Good Practice Guide on Responding to Student Mental Health Issues: Duty of Care Responsibilities for Student Services in Higher Education’ [ 22 ] and the recent ‘The University Mental Health Charter’ [ 2 ]. Universities UK produced a Good Practice Guide in 2015 called “Student mental wellbeing in higher education” [ 23 ]. An increasing number of initiatives have emerged that are either student-led or jointly developed with students, and which reflect the increasing emphasis students and student bodies place on mental health and well-being and the increased demand for mental health support: Examples include: Nightline— www.nightline.ac.uk , Students Against Depression— www.studentsagainstdepression.org , Student Minds— www.studentminds.org.uk/student-minds-and-mental-wealth.html and The Alliance for Student-Led Wellbeing— www.alliancestudentwellbeing.weebly.com/ .
Although requests for professional support have increased substantially [ 24 ] only a third of students with mental health problems seek support from counselling services in the UK [ 12 ]. Many students encounter barriers to seeking help such as stigma or lack of awareness of services [ 25 ], and without formal support or intervention, there is a risk of deterioration. FE colleges and universities have identified the need to move beyond traditional forms of support and provide alternative, more accessible interventions aimed at improving mental health and well-being. Higher education institutions have a unique opportunity to identify, prevent, and treat mental health problems because they provide support in multiple aspects of students’ lives including academic studies, recreational activities, pastoral and counselling services, and residential accommodation.
In order to develop services that better meet the needs of students and design environments that are supportive of developing mental wellbeing it is necessary to explore and better understand the factors that lead to poor mental health in students.
Research objectives
The overall aim of this review was to identify, appraise and synthesise existing research evidence that explores the aetiology of poor mental health and mental wellbeing amongst students in tertiary level education. We aimed to gain a better understanding of the mechanisms that lead to poor mental health amongst tertiary level students and, in so doing, make evidence-based recommendations for policy, practice and future research priorities. Specific objectives in line with the project brief were to:
To co-produce with stakeholders a conceptual framework for exploring the factors associated with poorer mental health in students in tertiary settings. The factors may be both predictive, identifying students at risk, or causal, explaining why they are at risk. They may also be protective, promoting mental wellbeing.
To conduct a review drawing on qualitative studies, observational studies and surveys to explore the aetiology of poor mental health in students in university and college settings and identify factors which promote mental wellbeing amongst students.
To identify evidence-based recommendations for policy, service provision and future research that focus on prevention and early identification of poor mental health
Methodology
Identification of relevant evidence.
The following inclusion criteria were used to guide the development of the search strategy and the selection of studies.
We included students from a variety of further education settings (16 yrs + or 18 yrs + , including mature students, international students, distance learning students, students at specific transition points).
Universities and colleges in the UK. We were also interested in the context prior to the beginning of tertiary education, including factors during transition from home and secondary education or existing employment to tertiary education.
Any factor shown to be associated with mental health of students in tertiary level education. This included clinical indicators such as diagnosis and treatment and/or referral for depression and anxiety. Self-reported measures of wellbeing, happiness, stress, anxiety and depression were included. We did not include measures of academic achievement or engagement with learning as indicators of mental wellbeing.
Study design
We included cross-sectional and longitudinal studies that looked at factors associated with mental health outcomes in Table 5 .
Data extraction and quality appraisal
We extracted and tabulated key data from the included papers. Data extraction was undertaken by one reviewer, with a 10% sample checked for accuracy and consistency The quality of the included studies were evaluated using the Newcastle-Ottawa Scale [ 26 ] and the findings of the quality appraisal used in weighting the strength of associations and also identifying gaps for future high quality research.
Involvement of stakeholders
We recruited students, ex-students and parents of students to a public involvement group which met on-line three times during the process of the review and following the completion of the review. During a workshop meeting we asked for members of the group to draw on their personal experiences to suggest factors which were not mentioned in the literature.
Methods of synthesis
We undertook a narrative synthesis [ 27 ] due to the heterogeneity in the exposures and outcomes that were measured across the studies. Data showing the direction of effects and the strength of the association (correlation coefficients) were recorded and tabulated to aid comparison between studies.
Search strategy
Searches were conducted in the following electronic databases: Medline, Applied Social Sciences Index and Abstracts (ASSIA), International Bibliography of Social Sciences (IBSS), Science,PsycINFO and Science and Social Sciences Ciatation Indexes. Additional searches of grey literature, and reference lists of included studies were also undertaken.
The search strategy combined a number of terms relating to students and mental health and risk factors. The search terms included both subject (MeSH) and free-text searches. The searches were limited to papers about humans in English, published from 2010 to June 2020. The flow of studies through the review process is summarised in Fig. 1 .
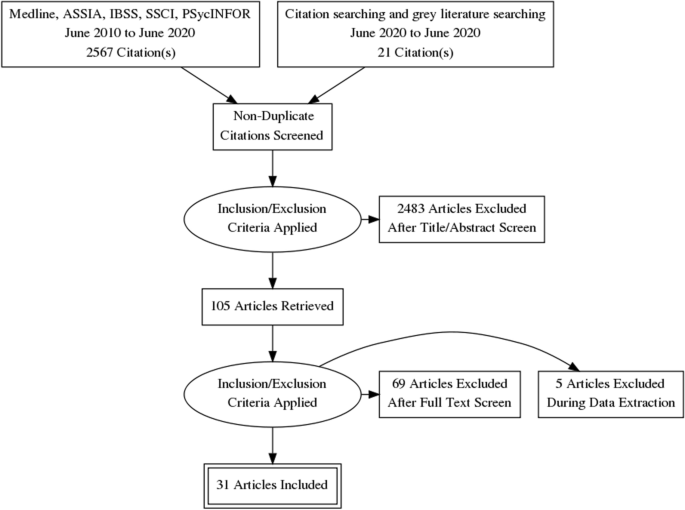
Flow diagram
The full search strategy for Medline is provided in Appendix 1 .
Thirty-one quantitative, observational studies (39 papers) met the inclusion criteria. The total number of students that participated in the quantitative studies was 17,476, with studies ranging in size from 57 to 3706. Eighteen studies recruited student participants from only one university; five studies (10 publications) [ 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] included seven or more universities. Six studies (7 publications) [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ] only recruited first year students, while the majority of studies recruited students from a range of year groups. Five studies [ 39 , 42 , 43 , 44 , 45 ] recruited only, or mainly, psychology students which may impact on the generalisability of findings. A number of studies focused on students studying particular subjects including: nursing [ 46 ] medicine [ 47 ], business [ 48 ], sports science [ 49 ]. One study [ 50 ] recruited LGBTQ (lesbian, gay, bisexual, transgender, intersex, queer/questioning) students, and one [ 51 ] recruited students who had attended hospital having self-harmed. In 27 of the studies, there were more female than male participants. The mean age of the participants ranged from 19 to 28 years. Ethnicity was not reported in 19 of the studies. Where ethnicity was reported, the proportion that were ‘white British’ ranged from 71 – 90%. See Table 1 for a summary of the characteristics of the included studies and the participants.
Design and quality appraisal of the included studies
The majority of included studies ( n = 22) were cross-sectional surveys. Nine studies (10 publications) [ 35 , 36 , 39 , 41 , 43 , 50 , 51 , 52 , 53 , 62 ] were longitudinal in design, recording survey data at different time points to explore changes in the variables being measured. The duration of time that these studies covered ranged from 19 weeks to 12 years. Most of the studies ( n = 22) only recruited participants from a single university. The use of one university setting and the large number of studies that recruited only psychology students weakens the wider applicability of the included studies.
Quantitative variables
Included studies ( n = 31) measured a wide range of variables and explored their association with poor mental health and wellbeing. These included individual level factors: age, gender, sexual orientation, ethnicity and a range of psychological variables. They also included factors that related to mental health variables (family history, personal history and mental health literacy), pre-university factors (childhood trauma and parenting behaviour. University level factors including social isolation, adjustment and engagement with learning. Their association was measured against different measures of positive mental health and poor mental health.
Measurement of association and the strength of that association has some limitations in addressing our research question. It cannot prove causality, and nor can it capture fully the complexity of the inter-relationship and compounding aspect of the variables. For example, the stress of adjustment may be manageable, until it is combined with feeling isolated and out of place. Measurement itself may also be misleading, only capturing what is measureable, and may miss variables that are important but not known. We included both qualitative and PPI input to identify missed but important variables.
The wide range of variables and different outcomes, with few studies measuring the same variable and outcomes, prevented meta-analyses of findings which are therefore described narratively.
The variables described were categorised during the analyses into the following categories:
Vulnerabilities – factors that are associated with poor mental health
Individual level factors including; age, ethnicity, gender and a range of psychological variables were all measured against different mental health outcomes including depression, anxiety, paranoia, and suicidal behaviour, self-harm, coping and emotional intelligence.
Six studies [ 40 , 42 , 47 , 50 , 60 , 63 ] examined a student’s ages and association with mental health. There was inconsistency in the study findings, with studies finding that age (21 or older) was associated with fewer depressive symptoms, lower likelihood of suicide ideation and attempt, self-harm, and positively associated with better coping skills and mental wellbeing. This finding was not however consistent across studies and the association was weak. Theoretical models that seek to explain this mechanism have suggested that older age groups may cope better due to emotion-regulation strategies improving with age [ 67 ]. However, those over 30 experienced greater financial stress than those aged 17-19 in another study [ 63 ].
Sexual orientation
Four studies [ 33 , 40 , 64 , 68 ] examined the association between poor mental health and sexual orientation status. In all of the studies LGBTQ students were at significantly greater risk of mental health problems including depression [ 40 ], anxiety [ 40 ], suicidal behaviour [ 33 , 40 , 64 ], self harm [ 33 , 40 , 64 ], use of mental health services [ 33 ] and low levels of wellbeing [ 68 ]. The risk of mental health problems in these students compared with heterosexual students, ranged from OR 1.4 to 4.5. This elevated risk may reflect the greater levels of isolation and discrimination commonly experienced by minority groups.
Nine studies [ 33 , 38 , 39 , 40 , 42 , 47 , 50 , 60 , 63 ] examined whether gender was associated mental health variables. Two studies [ 33 , 47 ] found that being female was statistically significantly associated with use of mental health services, having a current mental health problem, suicide risk, self harm [ 33 ] and depression [ 47 ]. The results were not consistent, with another study [ 60 ] finding the association was not significant. Three studies [ 39 , 40 , 42 ] that considered mediating variables such as adaptability and coping found no difference or very weak associations.
Two studies [ 47 , 60 ] examined the extent to which ethnicity was associated with mental health One study [ 47 ] reported that the risks of depression were significantly greater for those who categorised themselves as non-white (OR 8.36 p = 0.004). Non-white ethnicity was also associated with poorer mental health in another cross-sectional study [ 63 ]. There was no significant difference in the McIntyre et al. (2018) study [ 60 ]. The small number of participants from ethnic minority groups represented across the studies means that this data is very limited.
Family factors
Six studies [ 33 , 40 , 42 , 50 , 60 ] explored the association of a concept that related to a student’s experiences in childhood and before going to university. Three studies [ 40 , 50 , 60 ] explored the impact of ACEs (Adverse Childhood Experiences) assessed using the same scale by Feletti (2009) [ 69 ] and another explored the impact of abuse in childhood [ 46 ]. Two studies examined the impact of attachment anxiety and avoidance [ 42 ], and parental acceptance [ 46 , 59 ]. The studies measured different mental health outcomes including; positive and negative affect, coping, suicide risk, suicide attempt, current mental health problem, use of mental health services, psychological adjustment, depression and anxiety.
The three studies that explored the impact of ACE’s all found a significant and positive relationship with poor mental health amongst university students. O’Neill et al. (2018) [ 50 ] in a longitudinal study ( n = 739) showed that there was in increased likelihood in self-harm and suicidal behaviours in those with either moderate or high levels of childhood adversities (OR:5.5 to 8.6) [ 50 ]. McIntyre et al. (2018) [ 60 ] ( n = 1135) also explored other dimensions of adversity including childhood trauma through multiple regression analysis with other predictive variables. They found that childhood trauma was significantly positively correlated with anxiety, depression and paranoia (ß = 0.18, 0.09, 0.18) though the association was not as strong as the correlation seen for loneliness (ß = 0.40) [ 60 ]. McLafferty et al. (2019) [ 40 ] explored the compounding impact of childhood adversity and negative parenting practices (over-control, overprotection and overindulgence) on poor mental health (depression OR 1.8, anxiety OR 2.1 suicidal behaviour OR 2.3, self-harm OR 2.0).
Gaan et al.’s (2019) survey of LGBTQ students ( n = 1567) found in a multivariate analyses that sexual abuse, other abuse from violence from someone close, and being female had the highest odds ratios for poor mental health and were significantly associated with all poor mental health outcomes [ 33 ].
While childhood trauma and past abuse poses a risk to mental health for all young people it may place additional stresses for students at university. Entry to university represents life stage where there is potential exposure to new and additional stressors, and the possibility that these students may become more isolated and find it more difficult to develop a sense of belonging. Students may be separated for the first time from protective friendships. However, the mechanisms that link childhood adversities and negative psychopathology, self-harm and suicidal behaviour are not clear [ 40 ]. McLafferty et al. (2019) also measured the ability to cope and these are not always impacted by childhood adversities [ 40 ]. They suggest that some children learn to cope and build resilience that may be beneficial.
McLafferty et al. (2019) [ 40 ] also studied parenting practices. Parental over-control and over-indulgence was also related to significantly poorer coping (OR -0.075 p < 0.05) and this was related to developing poorer coping scores (OR -0.21 p < 0.001) [ 40 ]. These parenting factors only became risk factors when stress levels were high for students at university. It should be noted that these studies used self-report, and responses regarding views of parenting may be subjective and open to interpretation. Lloyd et al.’s (2014) survey found significant positive correlations between perceived parental acceptance and students’ psychological adjustment, with paternal acceptance being the stronger predictor of adjustment.
Autistic students may display social communication and interaction deficits that can have negative emotional impacts. This may be particularly true during young adulthood, a period of increased social demands and expectations. Two studies [ 56 ] found that those with autism had a low but statistically significant association with poor social problem-solving skills and depression.
Mental health history
Three studies [ 47 , 51 , 68 ] investigated mental health variables and their impact on mental health of students in higher education. These included; a family history of mental illness and a personal history of mental illness.
Students with a family history or a personal history of mental illness appear to have a significantly greater risk of developing problems with mental health at university [ 47 ]. Mahadevan et al. (2010) [ 51 ] found that university students who self-harm have a significantly greater risk (OR 5.33) of having an eating disorder than a comparison group of young adults who self-harm but are not students.
Buffers – factors that are protective of mental wellbeing
Psychological factors.
Twelve studies [ 29 , 39 , 40 , 41 , 42 , 43 , 46 , 49 , 54 , 58 , 64 ] assessed the association of a range of psychological variables and different aspects of mental wellbeing and poor mental health. We categorised these into the following two categories: firstly, psychological variables measuring an individual’s response to change and stressors including adaptability, resilience, grit and emotional regulation [ 39 , 40 , 41 , 42 , 43 , 46 , 49 , 54 , 58 ] and secondly, those that measure self-esteem and body image [ 29 , 64 ].
The evidence from the eight included quantitative studies suggests that students with psychological strengths including; optimism, self-efficacy [ 70 ], resilience, grit [ 58 ], use of positive reappraisal [ 49 ], helpful coping strategies [ 42 ] and emotional intelligence [ 41 , 46 ] are more likely to experience greater mental wellbeing (see Table 2 for a description of the psychological variables measured). The positive association between these psychological strengths and mental well-being had a positive affect with associations ranging from r = 0.2–0.5 and OR1.27 [ 41 , 43 , 46 , 49 , 54 ] (low to moderate strength of association). The negative associations with depressive symptoms are also statistically significant but with a weaker association ( r = -0.2—0.3) [ 43 , 49 , 54 ].
Denovan (2017a) [ 43 ] in a longitudinal study found that the association between psychological strengths and positive mental wellbeing was not static and that not all the strengths remained statistically significant over time. The only factors that remained significant during the transition period were self-efficacy and optimism, remaining statistically significant as they started university and 6 months later.
Parental factors
Only one study [ 59 ] explored family factors associated with the development of psychological strengths that would equip young people as they managed the challenges and stressors encountered during the transition to higher education. Lloyd et al. (2014) [ 59 ] found that perceived maternal and paternal acceptance made significant and unique contributions to students’ psychological adjustment. Their research methods are limited by their reliance on retrospective measures and self-report measures of variables, and these results could be influenced by recall bias.
Two studies [ 29 , 64 ] considered the impact of how individuals view themselves on poor mental health. One study considered the impact of self-esteem and the association with non-accidental self-injury (NSSI) and suicide attempt amongst 734 university students. As rates of suicide and NSSI are higher amongst LGBT (lesbian, gay, bisexual, transgender) students, the prevalence of low self-esteem was compared. There was a low but statistically significant association between low self-esteem and NSSI, though not for suicide attempt. A large survey, including participants from seven universities [ 42 ] compared depressive symptoms in students with marked body image concerns, reporting that the risk of depressive symptoms was greater (OR 2.93) than for those with lower levels of body image concerns.
Mental health literacy and help seeking behaviour
Two studies [ 48 , 68 ] investigated attitudes to mental illness, mental health literacy and help seeking for mental health problems.
University students who lack sufficient mental health literacy skills to be able to recognise problems or where there are attitudes that foster shame at admitting to having mental health problems can result in students not recognising problems and/or failing to seek professional help [ 48 , 68 ]. Gorcyznski et al. (2017) [ 68 ] found that women and those who had a history of previous mental health problems exhibited significantly higher levels of mental health literacy. Greater mental health literacy was associated with an increased likelihood that individuals would seek help for mental health problems. They found that many students find it hard to identify symptoms of mental health problems and that 42% of students are unaware of where to access available resources. Of those who expressed an intention to seek help for mental health problems, most expressed a preference for online resources, and seeking help from family and friends, rather than medical professionals such as GPs.
Kotera et al. (2019) [ 48 ] identified self-compassion as an explanatory variable, reducing social comparison, promoting self-acceptance and recognition that discomfort is an inevitable human experience. The study found a strong, significant correlation between self-compassion and mental health symptoms ( r = -0.6. p < 0.01).
There again appears to be a cycle of reinforcement, where poor mental health symptoms are felt to be a source of shame and become hidden, help is not sought, and further isolation ensues, leading to further deterioration in mental health. Factors that can interrupt the cycle are self-compassion, leading to more readiness to seek help (see Fig. 2 ).
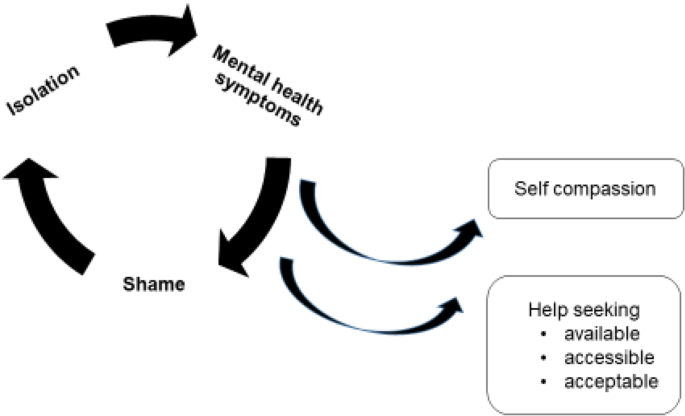
Poor mental health – cycles of reinforcement
Social networks
Nine studies [ 33 , 38 , 41 , 46 , 51 , 54 , 60 , 64 , 65 ] examined the concepts of loneliness and social support and its association with mental health in university students. One study also included students at other Higher Education Institutions [ 46 ]. Eight of the studies were surveys, and one was a retrospective case control study to examine the differences between university students and age-matched young people (non-university students) who attended hospital following deliberate self-harm [ 51 ].
Included studies demonstrated considerable variation in how they measured the concepts of social isolation, loneliness, social support and a sense of belonging. There were also differences in the types of outcomes measured to assess mental wellbeing and poor mental health. Grouping the studies within a broad category of ‘social factors’ therefore represents a limitation of this review given that different aspects of the phenomena may have been being measured. The tools used to measure these variables also differed. Only one scale (The UCLA loneliness scale) was used across multiple studies [ 41 , 60 , 65 ]. Diverse mental health outcomes were measured across the studies including positive affect, flourishing, self-harm, suicide risk, depression, anxiety and paranoia.
Three studies [ 41 , 60 , 62 ] measuring loneliness, two longitudinally [ 41 , 62 ], found a consistently positive association between loneliness and poor mental health in university students. Greater loneliness was linked to greater anxiety, stress, depression, poor general mental health, paranoia, alcohol abuse and eating disorder problems. The strength of the correlations ranged from 0–3-0.4 and were all statistically significant (see Tables 3 and 4 ). Loneliness was the strongest overall predictor of mental distress, of those measured. A strong identification with university friendship groups was most protective against distress relative to other social identities [ 60 ]. Whether poor mental health is the cause, or the result of loneliness was explored further in the studies. The results suggest that for general mental health, stress, depression and anxiety, loneliness induces or exacerbates symptoms of poor mental health over time [ 60 , 62 ]. The feedback cycle is evident, with loneliness leading to poor mental health which leads to withdrawal from social contacts and further exacerbation of loneliness.
Factors associated with protecting against loneliness by fostering supportive friendships and promoting mental wellbeing were also identified. Beliefs about the value of ‘leisure coping’, and attributes of resilience and emotional intelligence had a moderate, positive and significant association with developing mental wellbeing and were explored in three studies [ 46 , 54 , 66 ].
The transition to and first year at university represent critical times when friendships are developed. Thomas et al. (2020) [ 65 ] explored the factors that predict loneliness in the first year of university. A sense of community and higher levels of ‘social capital’ were significantly associated with lower levels of loneliness. ‘Social capital’ scales measure the development of emotionally supportive friendships and the ability to adjust to the disruption of old friendships as students transition to university. Students able to form close relationships within their first year at university are less likely to experience loneliness (r-0.09, r- 0.36, r- 0.34). One study [ 38 ] investigating the relationship between student experience and being the first in the family to attend university found that these students had lower ratings for peer group interactions.
Young adults at university and in higher education are facing multiple adjustments. Their ability to cope with these is influenced by many factors. Supportive friendships and a sense of belonging are factors that strengthen coping. Nightingale et al. (2012) undertook a longitudinal study to explore what factors were associated with university adjustment in a sample of first year students ( n = 331) [ 41 ]. They found that higher skills of emotion management and emotional self-efficacy were predictive of stable adjustment. These students also reported the lowest levels of loneliness and depression. This group had the skills to recognise their emotions and cope with stressors and were confident to access support. Students with poor emotion management and low levels of emotional self-efficacy may benefit from intervention to support the development of adaptive coping strategies and seeking support.
The positive and negative feedback loops
The relationship between the variables described appeared to work in positive and negative feedback loops with high levels of social capital easing the formation of a social network which acts as a critical buffer to stressors (see Fig. 3 ). Social networks and support give further strengthening and reinforcement, stimulating positive affect, engagement and flourishing. These, in turn, widen and deepen social networks for support and enhance a sense of wellbeing. Conversely young people who enter the transition to university/higher education with less social capital are less likely to identify with and locate a social network; isolation may follow, along with loneliness, anxiety, further withdrawal from contact with social networks and learning, and depression.
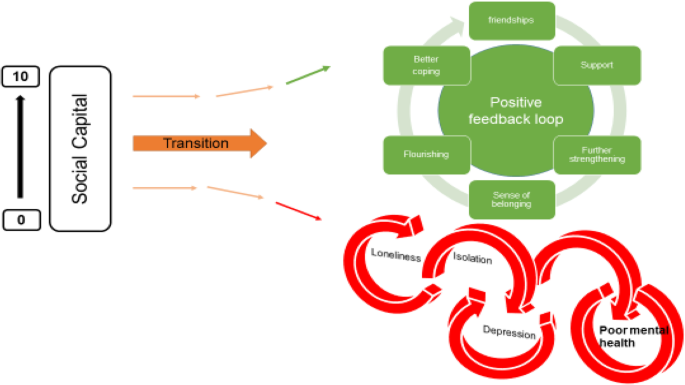
Triggers – factors that may act in combination with other factors to lead to poor mental health
Stress is seen as playing a key role in the development of poor mental health for students in higher education. Theoretical models and empirical studies have suggested that increases in stress are associated with decreases in student mental health [ 12 , 43 ]. Students at university experience the well-recognised stressors associated with academic study such as exams and course work. However, perhaps less well recognised are the processes of transition, requiring adapting to a new social and academic environment (Fisher 1994 cited by Denovan 2017a) [ 43 ]. Por et al. (2011) [ 46 ] in a small ( n = 130 prospective survey found a statistically significant correlation between higher levels of emotional intelligence and lower levels of perceived stress ( r = 0.40). Higher perceived stress was also associated with negative affect in two studies [ 43 , 46 ], and strongly negatively associated with positive affect (correlation -0.62) [ 54 ].
University variables
Eleven studies [ 35 , 39 , 47 , 51 , 52 , 54 , 60 , 63 , 65 , 83 , 84 ] explored university variables, and their association with mental health outcomes. The range of factors and their impact on mental health variables is limited, and there is little overlap. Knowledge gaps are shown by factors highlighted by our PPI group as potentially important but not identified in the literature (see Table 5 ). It should be noted that these may reflect the focus of our review, and our exclusion of intervention studies which may evaluate university factors.
High levels of perceived stress caused by exam and course work pressure was positively associated with poor mental health and lack of wellbeing [ 51 , 52 , 54 ]. Other potential stressors including financial anxieties and accommodation factors appeared to be less consistently associated with mental health outcomes [ 35 , 38 , 47 , 51 , 60 , 62 ]. Important mediators and buffers to these stressors are coping strategies and supportive networks (see conceptual model Appendix 2 ). One impact of financial pressures was that students who worked longer hours had less interaction with their peers, limiting the opportunities for these students to benefit from the protective effects of social support.
Red flags – behaviours associated with poor mental health and/or wellbeing
Engagement with learning and leisure activities.
Engagement with learning activities was strongly and positively associated with characteristics of adaptability [ 39 ] and also happiness and wellbeing [ 52 ] (see Fig. 4 ). Boulton et al. (2019) [ 52 ] undertook a longitudinal survey of undergraduate students at a campus-based university. They found that engagement and wellbeing varied during the term but were strongly correlated.
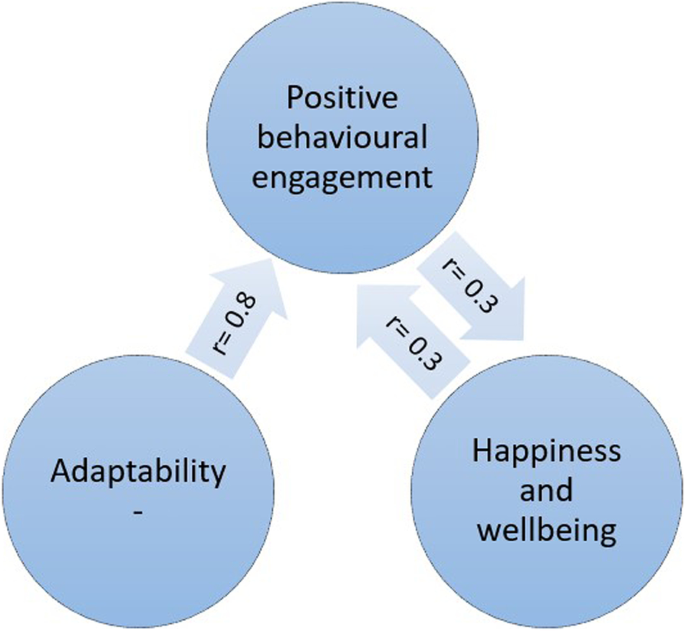
Engagement and wellbeing
Engagement occurred in a wide range of activities and behaviours. The authors suggest that the strong correlation between all forms of engagement with learning has possible instrumental value for the design of systems to monitor student engagement. Monitoring engagement might be used to identify changes in the behaviour of individuals to assist tutors in providing support and pastoral care. Students also were found to benefit from good induction activities provided by the university. Greater induction satisfaction was positively and strongly associated with a sense of community at university and with lower levels of loneliness [ 65 ].
The inte r- related nature of these variables is depicted in Fig. 4 . Greater adaptability is strongly associated with more positive engagement in learning and university life. More engagement is associated with higher mental wellbeing.
Denovan et al. (2017b) [ 54 ] explored leisure coping, its psychosocial functions and its relationship with mental wellbeing. An individual’s beliefs about the benefits of leisure activities to manage stress, facilitate the development of companionship and enhance mood were positively associated with flourishing and were negatively associated with perceived stress. Resilience was also measured. Resilience was strongly and positively associated with leisure coping beliefs and with indicators of mental wellbeing. The authors conclude that resilient individuals are more likely to use constructive means of coping (such as leisure coping) to proactively cultivate positive emotions which counteract the experience of stress and promote wellbeing. Leisure coping is predictive of positive affect which provides a strategy to reduce stress and sustain coping. The belief that friendships acquired through leisure provide social support is an example of leisure coping belief. Strong emotionally attached friendships that develop through participation in shared leisure pursuits are predictive of higher levels of well-being. Friendship bonds formed with fellow students at university are particularly important for maintaining mental health, and opportunities need to be developed and supported to ensure that meaningful social connections are made.
The ‘broaden-and-build theory’ (Fredickson 2004 [ 85 ] cited by [ 54 ]) may offer an explanation for the association seen between resilience, leisure coping and psychological wellbeing. The theory is based upon the role that positive and negative emotions have in shaping human adaptation. Positive emotions broaden thinking, enabling the individual to consider a range of ways of dealing with and adapting to their environment. Conversely, negative emotions narrow thinking and limit options for adapting. The former facilitates flourishing, facilitating future wellbeing. Resilient individuals are more likely to use constructive means of coping which generate positive emotion (Tugade & Fredrickson 2004 [ 86 ], cited by [ 54 ]). Positive emotions therefore lead to growth in coping resources, leading to greater well-being.
Health behaviours at university
Seven studies [ 29 , 31 , 38 , 45 , 51 , 54 , 66 ] examined how lifestyle behaviours might be linked with mental health outcomes. The studies looked at leisure activities [ 63 , 80 ], diet [ 29 ], alcohol use [ 29 , 31 , 38 , 51 ] and sleep [ 45 ].
Depressive symptoms were independently associated with problem drinking and possible alcohol dependence for both genders but were not associated with frequency of drinking and heavy episodic drinking. Students with higher levels of depressive symptoms reported significantly more problem drinking and possible alcohol dependence [ 31 ]. Mahadevan et al. (2010) [ 51 ] compared students and non-students seen in hospital for self-harm and found no difference in harmful use of alcohol and illicit drugs.
Poor sleep quality and increased consumption of unhealthy foods were also positively associated with depressive symptoms and perceived stress [ 29 ]. The correlation with dietary behaviours and poor mental health outcomes was low, but also confirmed by the negative correlation between less perceived stress and depressive symptoms and consumption of a healthier diet.
Physical activity and participation in leisure pursuits were both strongly correlated with mental wellbeing ( r = 0.4) [ 54 ], and negatively correlated with depressive symptoms and anxiety ( r = -0.6, -0.7) [ 66 ].
Thirty studies measuring the association between a wide range of factors and poor mental health and mental wellbeing in university and college students were identified and included in this review. Our purpose was to identify the factors that contribute to the growing prevalence of poor mental health amongst students in tertiary level education within the UK. We also aimed to identify factors that promote mental wellbeing and protect against deteriorating poor mental health.
Loneliness and social isolation were strongly associated with poor mental health and a sense of belonging and a strong support network were strongly associated with mental wellbeing and happiness. These associations were strongly positive in the eight studies that explored them and are consistent with other meta-analyses exploring the link between social support and mental health [ 87 ].
Another factor that appeared to be protective was older age when starting university. A wide range of personal traits and characteristics were also explored. Those associated with resilience, ability to adjust and better coping led to improved mental wellbeing. Better engagement appeared as an important mediator to potentially explain the relationship between these two variables. Engagement led to students being able to then tap into those features that are protective and promoting of mental wellbeing.
Other important risk factors for poor mental wellbeing that emerged were those students with existing or previous mental illness. Students on the autism spectrum and those with poor social problem-solving also were more likely to suffer from poor mental health. Negative self-image was also associated with poor mental health at university. Eating disorders were strongly associated with poor mental wellbeing and were found to be far more of a risk in students at university than in a comparative group of young people not in higher education. Other studies of university students also found that pre-existing poor mental health was a strong predictor of poor mental health in university students [ 88 ].
At a family level, the experience of childhood trauma and adverse experiences including, for example, neglect, household dysfunction or abuse, were strongly associated with poor mental health in young people at university. Students with a greater number of ‘adverse childhood experiences’ were at significantly greater risk of poor mental health than those students without experience of childhood trauma. This was also identified in a review of factors associated with depression and suicide related outcomes amongst university undergraduate students [ 88 ].
Our findings, in contrast to findings from other studies of university students, did not find that female gender associated with poor mental health and wellbeing, and it also found that being a mature student was protective of mental wellbeing.
Exam and course work pressure was associated with perceived stress and poor mental health. A lack of engagement with learning activities was also associated with poor mental health. A number of variables were not consistently shown to be associated with poor mental health including financial concerns and accommodation factors. Very little evidence related to university organisation or support structures was assessed in the evidence. One study found that a good induction programme had benefits for student mental wellbeing and may be a factor that enables students to become a part of a social network positive reinforcement cycle. Involvement in leisure activities was also found to be associated with improved coping strategies and better mental wellbeing. Students with poorer mental health tended to also eat in a less healthy manner, consume more harmful levels of alcohol, and experience poorer sleep.
This evidence review of the factors that influence mental health and wellbeing indicate areas where universities and higher education settings could develop and evaluate innovations in practice. These include:
Interventions before university to improve preparation of young people and their families for the transition to university.
Exploratory work to identify the acceptability and feasibility of identifying students at risk or who many be exhibiting indications of deteriorating mental health
Interventions that set out to foster a sense of belonging and identify
Creating environments that are helpful for building social networks
Improving mental health literacy and access to high quality support services
This review has a number of limitations. Most of the included studies were cross-sectional in design, with a small number being longitudinal ( n = 7), following students over a period of time to observe changes in the outcomes being measured. Two limitations of these sources of data is that they help to understand associations but do not reveal causality; secondly, we can only report the findings for those variables that were measured, and we therefore have to support causation in assuming these are the only factors that are related to mental health.
Furthermore, our approach has segregated and categorised variables in order to better understand the extent to which they impact mental health. This approach does not sufficiently explore or reveal the extent to which variables may compound one another, for example, feeling the stress of new ways of learning may not be a factor that influences mental health until it is combined with a sense of loneliness, anxiety about financial debt and a lack of parental support. We have used our PPI group and the development of vignettes of their experiences to seek to illustrate the compounding nature of the variables identified.
We limited our inclusion criteria to studies undertaken in the UK and published within the last decade (2009–2020), again meaning we may have limited our inclusion of relevant data. We also undertook single data extraction of data which may increase the risk of error in our data.
Understanding factors that influence students’ mental health and wellbeing offers the potential to find ways to identify strategies that enhance the students’ abilities to cope with the challenges of higher education. This review revealed a wide range of variables and the mechanisms that may explain how they impact upon mental wellbeing and increase the risk of poor mental health amongst students. It also identified a need for interventions that are implemented before young people make the transition to higher education. We both identified young people who are particularly vulnerable and the factors that arise that exacerbate poor mental health. We highlight that a sense of belonging and supportive networks are important buffers and that there are indicators including lack of engagement that may enable early intervention to provide targeted and appropriate support.
Availability of data and materials
Further details of the study and the findings can be provided on request to the lead author ([email protected]).
Association of Colleges. Association of Colleges’ survey on students with mental health conditions in further education. London: 2017.
Google Scholar
Hughes G, Spanner L. The University Mental Health Charter. Leeds: Student Minds; 2019.
Sivertsen B, Hysing M, Knapstad M, Harvey AG, Reneflot A, Lønning KJ, et al. Suicide attempts and non-suicidal self-harm among university students: prevalence study. BJPsych Open. 2019;5(2):e26.
Article PubMed PubMed Central Google Scholar
Storrie K, Ahern K, Tuckett A. A systematic review: students with mental health problems—a growing problem. Int J Nurs Pract. 2010;16(1):1–6.
Article PubMed Google Scholar
Pereira S, Reay K, Bottell J, Walker L, Dzikiti C, Platt C, Goodrham C. Student Mental Health Survey 2018: A large scale study into the prevalence of student mental illness within UK universities. 2019.
Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol. 2008;43(8):667–72.
Bewick B, Koutsopoulou G, Miles J, Slaa E, Barkham M. Changes in undergraduate students’ psychological well-being as they progress through university. Stud High Educ. 2010;35(6):633–45.
Article Google Scholar
Thorley C. Not By Degrees: Not by degrees: Improving student mental health in the UK’s universities. London: IPPR; 2017.
Eisenberg D, Golberstein E, Hunt JB. Mental health and academic success in college. BE J Econ Anal Pol. 2009;9(1):1–37.
Hysenbegasi A, Hass SL, Rowland CR. The impact of depression on the academic productivity of university students. J Ment Health Policy Econ. 2005;8(3):145.
PubMed Google Scholar
Chowdry H, Crawford C, Dearden L, Goodman A, Vignoles A. Widening participation in higher education: analysis using linked administrative data. J R Stat Soc A Stat Soc. 2013;176(2):431–57.
Macaskill A. The mental health of university students in the United Kingdom. Br J Guid Couns. 2013;41(4):426–41.
Belfield C, Britton J, van der Erve L. Higher Education finance reform: Raising the repayment threshold to£ 25,000 and freezing the fee cap at £ 9,250: Institute for Fiscal Studies Briefing note. London: Institute for Fiscal Studies; 2017. Available from https://ifs.org.uk/publications/9964 .
Benson-Egglenton J. The financial circumstances associated with high and low wellbeing in undergraduate students: a case study of an English Russell Group institution. J Furth High Educ. 2019;43(7):901–13.
Jessop DC, Herberts C, Solomon L. The impact of financial circumstances on student health. Br J Health Psychol. 2005;10(3):421–39.
(2020) SCSC. Canadians’ mental health during the COVID-19 pandemic. 2020.
(NUS) NUoS. Coronavirus Student Survey phase III November 2020. 2020.
Hellemans K, Abizaid A, Gabrys R, McQuaid R, Patterson Z. For university students, COVID-19 stress creates perfect conditions for mental health crises. The Conversation. 2020. Available from: https://theconversation.com/for-university-students-covid-19-stress-creates-perfect-conditions-for-mental-health-crises-149127 .
England N. Children and Young People with an Eating Disorder Waiting Times: NHS England; 2021 [Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/cyped-waiting-times/
King JA, Cabarkapa S, Leow FH, Ng CH. Addressing international student mental health during COVID-19: an imperative overdue. Australas Psychiatry. 2020;28(4):469.
Rana R, Smith E, Walking J. Degrees of disturbance: the new agenda; the Impact of Increasing Levels of Psychological Disturbance Amongst Students in Higher Education. England: Association for University and College Counselling Rugby; 1999.
AMOSSHE. Responding to student mental health issues: 'Duty of Care' responsibilities for student services in higher education. https://www.amosshe.org.uk/resources/Documents/AMOSSHE_Duty_of_Care_2001.pdf [accessed 24.12.2020]. (2001).
Universities UK. Student mental wellbeing in higher education. Good practice guide. London: Universities UK; 2015.
Williams M, Coare P, Marvell R, Pollard E, Houghton A-M, Anderson J. 2015. Understanding provision for students with mental health problems and intensive support needs: Report to HEFCE by the Institute for Employment Studies (IES) and Researching Equity, Access and Partnership (REAP). Institute for Employment Studies.
Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46(1):3–10.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. In.: Oxford; 2000.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890.
El Ansari W, Adetunji H, Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014a;22(2):90–7.
El Ansari W, Dibba E, Stock C. Body image concerns: levels, correlates and gender differences among students in the United Kingdom. Cent Eur J Public Health. 2014b;22(2):106–17.
Ansari EL, W, Oskrochi R, Stock C. Symptoms and health complaints and their association with perceived stress: Students from seven universities in England, Wales and Northern Ireland. J Public Health. 2013;21(5):413–25.
El Ansari W, Sebena R, Stock C. Do importance of religious faith and healthy lifestyle modify the relationships between depressive symptoms and four indicators of alcohol consumption? A survey of students across seven universities in England, Wales, and Northern Ireland. Subst Use Misuse. 2014c;49(3):211–20.
El Ansari W, Stock C. Is the health and wellbeing of university students associated with their academic performance? Cross sectional findings from the United Kingdom. International Journal of Environmental Research & Public Health [Electronic Resource]. 2010;7(2):509–27.
Gnan GH, Rahman Q, Ussher G, Baker D, West E, Rimes KA. General and LGBTQ-specific factors associated with mental health and suicide risk among LGBTQ students. J Youth Stud. 2019;22(10):1393–408.
Jackson SL, Dritschel B. Modeling the impact of social problem-solving deficits on depressive vulnerability in the broader autism phenotype. Res Aut Spectr Disord. 2016;21:128–38.
Richardson T, Elliott P, Roberts R. The impact of tuition fees amount on mental health over time in British students. J Public Health. 2015;37(3):412–8.
Article CAS Google Scholar
Richardson T, Mma Y, Jansen M, Elliott P, Roberts R. Financial difficulties and psychosis risk in British undergraduate students: a longitudinal analysis. J Public Ment Health. 2018;17(2):61–8.
Thomas L, Briggs P, Hart A, Kerrigan F. Understanding social media and identity work in young people transitioning to university. Comput Hum Behav. 2017;76:541–53.
Hixenbaugh P, Dewart H, Towell T. What enables students to succeed? An investigation of socio-demographic, health and student experience variables. Psychodyn Pract. 2012;18(3):285–301.
Holliman A, Martin A, Collie R. Adaptability, engagement, and degree completion: a longitudinal investigation of university students. Educ Psychol. 2018;38(6):785–99.
McLafferty M, Armour C, Bunting B, Ennis E, Lapsley C, Murray E, et al. Coping, stress, and negative childhood experiences: the link to psychopathology, self-harm, and suicidal behavior. Psychic J. 2019;8(3):293–306.
Nightingale S, Roberts S, Tariq V, Appleby Y, Barnes L, Harris R, et al. Trajectories of university adjustment in the United Kingdom: EMOTION management and emotional self-efficacy protect against initial poor adjustment. Learn Individ Differ. 2013;27:174–81.
Berry K, Kingswell S. An investigation of adult attachment and coping with exam-related stress. Br J Guid Couns. 2012;40(4):315.
Denovan A, Macaskill A. Stress and subjective well-being among first year UK undergraduate students. J Happiness Stud. 2017a;18(2):505–25.
Hassel S, Ridout N. An investigation of first-year students’ and lecturers’ expectations of university education. Front Psychol. 2018;8:2218.
Norbury R, Evans S. Time to think: subjective sleep quality, trait anxiety and university start time. Psychiatry Res. 2019;271:214–9.
Por J, Barriball L, Fitzpatrick J, Roberts J. Emotional intelligence: its relationship to stress, coping, well-being and professional performance in nursing students. Nurse Educ Today. 2011;31(8):855.
Honney K, Buszewicz M, Coppola W, Griffin M. Comparison of levels of depression in medical and non-medical students. Clin Teach. 2010;7(3):180–4.
Kotera Y, Conway E, Van Gordon W. Mental health of UK university business students: Relationship with shame, motivation and self-compassion. Journal of Education for Business. 2019;94(1):11–20.
Oliver EJ, Markland D, Hardy J. Interpretation of self-talk and post-lecture affective states of higher education students: a self-determination theory perspective. Br J Educ Psychol. 2010;80(Pt 2):307–23.
O’Neill S, McLafferty M, Ennis E, Lapsley C, Bjourson T, Armour C, et al. Socio-demographic, mental health and childhood adversity risk factors for self-harm and suicidal behaviour in College students in Northern Ireland. J Affect Disord. 2018;239:58–65.
Mahadevan S, Hawton K, Casey D. Deliberate self-harm in Oxford University students, 1993–2005: a descriptive and case-control study. Soc Psychiatry Psychiatr Epidemiol. 2010;45(2):211–9.
Boulton CA, Hughes E, Kent C, Smith JR, Williams HTP. Student engagement and wellbeing over time at a higher education institution. PLoS One [Electronic Resource]. 2019;14(11): e0225770.
Davies EL, Paltoglou AE. Public self-consciousness, pre-loading and drinking harms among university students. Subst Use Misuse. 2019;54(5):747–57.
Denovan A, Macaskill A. Stress, resilience and leisure coping among university students: Applying the broaden-and-build theory. Leisure Studies. 2017b;36(6):852–65.
El Ansari W, Vallentin-Holbech L, Stock C. Predictors of illicit drug/s use among university students in Northern Ireland, Wales and England. Glob J Health Sci. 2015;7(4):18–29.
Freeth M, Bullock T, Milne E. The distribution of and relationship between autistic traits and social anxiety in a UK student population. Autism. 2013;17(5):571–81.
Jessop DC, Reid M, Solomon L. Financial concern predicts deteriorations in mental and physical health among university students. Psychology Health. 2020;35(2):196–209.
Kannangara CS, Allen RE, Waugh G, Nahar N, Khan SZN, Rogerson S, Carson J. All that glitters is not grit: Three studies of grit in university students. Front Psychol. 2018;9:1539.
Lloyd J, Ward T, Young J. Do parental interpersonal power and prestige moderate the relationship between parental acceptance and psychological adjustment in U.K. Students? Cross-Cultural Research. The Journal of Comparative Social Science. 2014;48(3):326–35.
McIntyre JC, Worsley J, Corcoran R, Harrison Woods P, Bentall RP. Academic and non-academic predictors of student psychological distress: the role of social identity and loneliness. J Ment Health. 2018;27(3):230–9.
Ribchester C, Ross K, Rees EL. Examining the impact of pre-induction social networking on the student transition into higher education. Innov Educ Teach Int. 2014;51(4):355–65.
Richardson T, Elliott P, Roberts R. Relationship between loneliness and mental health in students. J Public Ment Health. 2017a;16(2):48–54.
Richardson T, Elliott P, Roberts R, Jansen M. A Longitudinal Study of Financial Difficulties and Mental Health in a National Sample of British Undergraduate Students. Community Ment Health J. 2017;53(3):344–52.
Taylor PJ, Dhingra K, Dickson JM, McDermott E. Psychological Correlates of Self-Harm within Gay, Lesbian and Bisexual UK University Students. Arch Suicide Res. 2020;24(sup1):41–56.
Thomas L, Orme E, Kerrigan F. Student loneliness: The role of social media through life transitions. Comput Educ. 2020;146:103754.
Tyson P, Wilson K, Crone D, Brailsford R, Laws K. Physical activity and mental health in a student population. J Ment Health. 2010;19(6):492–9.
Folkman S. The Oxford handbook of stress, health, and coping. Oxford: Oxford University Press; 2011.
Gorczynski P, Sims-schouten W, Hill D, Wilson JC. Examining mental health literacy, help seeking behaviours, and mental health outcomes in UK university students. J Ment Health Train Educ Pract. 2017;12(2):111–20.
Felitti VJ. Adverse childhood experiences and adult health. Acad Pediatr. 2009;9(3):131–2.
Denovan A, Macaskill A. An interpretative phenomenological analysis of stress and coping in first year undergraduates. Br Educ Res J. 2013;39(6):1002–24.
Bandura A. Self-efficacy: The foundation of agency. Control of human behavior, mental processes, and consciousness: Essays in honor of the 60th birthday of August Flammer. 2000;16.
Martin AJ, Nejad H, Colmar S, Liem GAD. Adaptability: Conceptual and empirical perspectives on responses to change, novelty and uncertainty. J Psychol Couns Sch. 2012;22(1):58–81.
Lazarus RS, Folkman S. Stress, appraisal, and coping: Springer publishing company; 1984.
Gross JJ. Emotion regulation: Past, present, future. Cogn Emot. 1999;13(5):551–73.
Mayer JD, Salovey P, Caruso DR. TARGET ARTICLES:" Emotional Intelligence: Theory, Findings, and Implications". Psychol Inq. 2004;15(3):197–215.
Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92(6):1087.
Snyder CR, Ilardi SS, Cheavens J, Michael ST, Yamhure L, Sympson S. The role of hope in cognitive-behavior therapies. Cognit Ther Res. 2000;24(6):747–62.
Scheier MF, Carver CS, Bridges MW. Optimism, pessimism, and psychological well-being. 2001.
Seligman ME. Positive psychology in practice: Wiley; 2012.
Masten AS. Ordinary magic: Lessons from research on resilience in human development. Education Canada. 2009;49(3):28–32.
Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self-esteem and specific self-esteem: Different concepts, different outcomes. Am Sociol Rev. 1995:141–56.
Oliver EJ, Markland D, Hardy J. Interpretation of self-talk and post-lecture affective states of higher education students: A self-determination theory perspective. Br J Educ Psychol. 2010;80(2):307–23.
Hofmann W, Friese M, Strack F. Impulse and self-control from a dual-systems perspective. Perspect Psychol Sci. 2009;4(2):162–76.
Aceijas C, Waldhausl S, Lambert N, Cassar S, Bello-Corassa R. Determinants of health-related lifestyles among university students. Perspect Public Health. 2017;137(4):227–36.
Fredrickson BL. The broaden–and–build theory of positive emotions. Philos Trans R Soc Lond B Biol Sci. 2004;359(1449):1367–77.
Tugade MM, Fredrickson BL, Feldman Barrett L. Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. J Pers. 2004;72(6):1161–90.
Harandi TF, Taghinasab MM, Nayeri TD. The correlation of social support with mental health: A meta-analysis. Electron physician. 2017;9(9):5212.
Sheldon E, Simmonds-Buckley M, Bone C, Mascarenhas T, Chan N, Wincott M, Gleeson H, Sow K, Hind D, Barkham M. Prevalence and risk factors for mental health problems in university undergraduate students: A systematic review with meta-analysis. J Affect Disord. 2021;287:282–92.
Download references
Acknowledgements
We acknowledge the input from our public advisory group which included current and former students, and family members of students who have struggled with their mental health. The group gave us their extremely valuable insights to assist our understanding of the evidence.
This project was supported by funding from the National Institute for Health Research as part of the NIHR Public Health Research Programme (fuding reference 127659 Public Health Review Team). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
University of Sheffield, Sheffield, UK
Fiona Campbell, Lindsay Blank, Anna Cantrell, Susan Baxter, Christopher Blackmore, Jan Dixon & Elizabeth Goyder
You can also search for this author in PubMed Google Scholar
Contributions
All of the included authors designed the project methods and prepared a protocol. A.C. designed the search strategy. F.C, L.B and C.B screened the identified citations and undertook data extraction. S.B. led the PPI involvement. JD participated as a member of the PPI group. F.C and L.B undertook the analysis. F.C. and L.B wrote the main manuscript text. All authors reviewed the manuscript. F.C designed Figs. 2 , 3 and 4 . The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Fiona Campbell .
Ethics declarations
Ethics approval and consent to participate.
Not applicable as this was secondary research.
Consent for publication
Not applicable.
Competing interests
None of the authors have competing interests or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Campbell, F., Blank, L., Cantrell, A. et al. Factors that influence mental health of university and college students in the UK: a systematic review. BMC Public Health 22 , 1778 (2022). https://doi.org/10.1186/s12889-022-13943-x
Download citation
Received : 03 February 2022
Accepted : 25 July 2022
Published : 20 September 2022
DOI : https://doi.org/10.1186/s12889-022-13943-x

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student mental health
- Mental wellbeing
- Risk factors
- Rapid review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 3.9.2020 in Vol 22 , No 9 (2020) : September
Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study
Authors of this article:

Original Paper
- Changwon Son 1 , BS, MS ;
- Sudeep Hegde 1 , BEng, MS, PhD ;
- Alec Smith 1 , BS ;
- Xiaomei Wang 1 , BS, PhD ;
- Farzan Sasangohar 1, 2 , BA, BCS, MASc, SM, PhD
1 Department of Industrial and Systems Engineering, Texas A&M University, College Station, TX, United States
2 Center for Outcomes Research, Houston Methodist Hospital, Houston, TX, United States
Corresponding Author:
Farzan Sasangohar, BA, BCS, MASc, SM, PhD
Department of Industrial and Systems Engineering
Texas A&M University
College Station, TX, 77843
United States
Phone: 1 979 458 2337
Email: [email protected]
Background: Student mental health in higher education has been an increasing concern. The COVID-19 pandemic situation has brought this vulnerable population into renewed focus.
Objective: Our study aims to conduct a timely assessment of the effects of the COVID-19 pandemic on the mental health of college students.
Methods: We conducted interview surveys with 195 students at a large public university in the United States to understand the effects of the pandemic on their mental health and well-being. The data were analyzed through quantitative and qualitative methods.
Results: Of the 195 students, 138 (71%) indicated increased stress and anxiety due to the COVID-19 outbreak. Multiple stressors were identified that contributed to the increased levels of stress, anxiety, and depressive thoughts among students. These included fear and worry about their own health and of their loved ones (177/195, 91% reported negative impacts of the pandemic), difficulty in concentrating (173/195, 89%), disruptions to sleeping patterns (168/195, 86%), decreased social interactions due to physical distancing (167/195, 86%), and increased concerns on academic performance (159/195, 82%). To cope with stress and anxiety, participants have sought support from others and helped themselves by adopting either negative or positive coping mechanisms.
Conclusions: Due to the long-lasting pandemic situation and onerous measures such as lockdown and stay-at-home orders, the COVID-19 pandemic brings negative impacts on higher education. The findings of our study highlight the urgent need to develop interventions and preventive strategies to address the mental health of college students.
Introduction
Mental health issues are the leading impediment to academic success. Mental illness can affect students’ motivation, concentration, and social interactions—crucial factors for students to succeed in higher education [ 1 ]. The 2019 Annual Report of the Center for Collegiate Mental Health [ 2 ] reported that anxiety continues to be the most common problem (62.7% of 82,685 respondents) among students who completed the Counseling Center Assessment of Psychological Symptoms, with clinicians also reporting that anxiety continues to be the most common diagnosis of the students that seek services at university counseling centers. Consistent with the national trend, Texas A&M University has seen a rise in the number of students seeking services for anxiety disorders over the past 8 years. In 2018, slightly over 50% of students reported anxiety as the main reason for seeking services. Despite the increasing need for mental health care services at postsecondary institutions, alarmingly, only a small portion of students committing suicide contact their institution counseling centers [ 3 ], perhaps due to the stigma associated with mental health. Such negative stigma surrounding mental health diagnosis and care has been found to correlate with a reduction in adherence to treatment and even early termination of treatment [ 4 ].
The COVID-19 pandemic has brought into focus the mental health of various affected populations. It is known that the prevalence of epidemics accentuates or creates new stressors including fear and worry for oneself or loved ones, constraints on physical movement and social activities due to quarantine, and sudden and radical lifestyle changes. A recent review of virus outbreaks and pandemics documented stressors such as infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma [ 5 ]. Much of the current literature on psychological impacts of COVID-19 has emerged from the earliest hot spots in China. Although several studies have assessed mental health issues during epidemics, most have focused on health workers, patients, children, and the general population [ 6 , 7 ]. For example, a recent poll by The Kaiser Family Foundation showed that 47% of those sheltering in place reported negative mental health effects resulting from worry or stress related to COVID-19 [ 8 ]. Nelson et al [ 9 ] have found elevated levels of anxiety and depressive symptoms among general population samples in North America and Europe. However, with the exception of a few studies, notably from China [ 10 - 12 ], there is sparse evidence of the psychological or mental health effects of the current pandemic on college students, who are known to be a vulnerable population [ 13 ]. Although the findings from these studies thus far converge on the uptick of mental health issues among college students, the contributing factors may not necessarily be generalizable to populations in other countries. As highlighted in multiple recent correspondences, there is an urgent need to assess effects of the current pandemic on the mental health and well-being of college students [ 14 - 17 ].
The aim of this study is to identify major stressors associated with the COVID-19 pandemic and to understand their effects on college students’ mental health. This paper documents the findings from online interview surveys conducted in a large university system in Texas.
Study Design
A semistructured interview survey guide was designed with the purpose of assessing the mental health status of college students both quantitatively and qualitatively. In addition, the interview aimed to capture the ways that students have been coping with the stress associated with the pandemic situation. First, our study assesses participants’ general stress levels using the Perceived Stress Scale-10 (PSS) [ 18 ]. PSS is a widely used instrument to measure overall stress in the past month [ 19 ]. Second, participants were asked if their own and peers’ (two separate questions) stress and anxiety increased, decreased, or remained the same because of the COVID-19 pandemic. For those who indicated increased stress and anxiety during the pandemic, we questioned their stress coping strategies and use of available mental health counseling services. We then elicited pandemic-specific stressors and their manifestations across 12 academic-, health-, and lifestyle-related categories of outcomes such as effects on own or loved ones’ health, sleeping habits, eating habits, financial situation, changes to their living environment, academic workload, and social relations. Students were also asked about the impact of COVID-19 on depressive and suicidal thoughts. These constructs were derived from existing literature identifying prominent factors affecting college students’ mental health [ 20 , 21 ]. Feedback on the severity of COVID-19’s impact on these aspects were elicited using a 4-point scale: 0 (none), 1 (mild), 2 (moderate), and 3 (severe). Participants were asked to elaborate on each response. Third, participants were guided to describe stressors, coping strategies, and barriers to mental health treatment during a typical semester without associating with the COVID-19 pandemic. Although multiple analyses of the collected data are currently under progress, PSS results and the COVID-19–related findings are presented in this paper.
Participants
Participants were recruited from the student population of a large university system in Texas, United States. This particular university closed all their campuses on March 23, 2020, and held all its classes virtually in response to the COVID-19 pandemic. In addition, the state of Texas issued a stay-at-home order on April 2, 2020. Most interviews were conducted about 1 month after the stay-at-home order in April 2020. Figure 1 illustrates the trend of cumulative confirmed cases and a timeline of major events that took place in the university and the state of Texas. Participants were recruited by undergraduate student researchers through email, text messaging, and snowball sampling. The only inclusion criteria for participation was that participants should have been enrolled as undergraduate students in the university at the time of the interviews.

The interviews were conducted by 20 undergraduate researchers trained in qualitative methods and the use of the interview survey guide described above. None of the authors conducted the interviews. All interviews were conducted via Zoom [ 22 ] and were audio recorded. The recordings were later transcribed using Otter.ai [ 23 ], an artificial intelligence–based transcription service, and verified for accuracy manually. Prior to the interview, participants were provided an information document about the study approved by the university’s Institutional Review Board (No 2019-1341D). Upon verbal consent, participants were asked to respond to a questionnaire about their demographic information such as age, gender, year of college, and program of study before completing the interview. Participation was voluntary and participants were not compensated.
Data Analysis
First, descriptive statistics were compiled to describe participants’ demographics (eg, age, gender, academic year, and major) and the distribution of the ratings on PSS-10 survey items. A total PSS score per participant was calculated by first reversing the scores of the positive items (4-7, 9, and 10) and then adding all the ten scores. A mean (SD) PSS score was computed to evaluate the overall level of stress and anxiety among the participants during the COVID-19 pandemic. Second, participants’ answers to 12 academic-, health-, and lifestyle-related questions were analyzed to understand relative impacts of the pandemic on various aspects of college students’ mental health. Percentages of participants who indicated negative ratings (ie, mild, moderate, or severe influence) on these questions were calculated and ranked in a descending order. Qualitative answers to the 12 stressors and coping strategies were analyzed using thematic analysis [ 24 , 25 ] similar to the deductive coding step in the grounded theory method [ 26 ]. A single coder (CS), trained in qualitative analysis methods, analyzed the transcripts and identified themes using an open coding process, which does not use a priori codes or codes created prior to the analysis and places an emphasis on information that can be extracted directly from the data. Following the identification of themes, the coder discussed the codes with two other coders (XW and AS) trained in qualitative analysis and mental health research to resolve discrepancies among related themes and discuss saturation. The coders consisted of two Ph.D. students and one postdoctoral fellow at the same university. MAXQDA (VERBI GmbH) [ 27 ] was used as a computer software program to carry out the qualitative analysis.
Of the 266 university students initially recruited by the undergraduate researchers, 17 retreated and 249 participated in this study. There were 3 graduate students and 51 participants who had missing data points and were excluded, and data from 195 participants were used in the analysis. The average age was 20.7 (SD 1.7) years, and there were more female students (111/195, 57%) than male students (84/195, 43%). Approximately 70% of the participants were junior and senior students. About 60% of the participants were majoring in the college of engineering, which was the largest college in the university population ( Table 1 ). The mean PSS score for the 195 participants was 18.8 (SD 4.9), indicating moderate perceived stress in the month prior to the interview ( Table 2 ).
a PSS: Perceived Stress Scale-10.
Challenges to College Students’ Mental Health During COVID-19
Out of 195 participants, 138 (71%) indicated that their stress and anxiety had increased due to the COVID-19 pandemic, whereas 39 (20%) indicated it remained the same and 18 (9%) mentioned that the stress and anxiety had actually decreased. Among those who perceived increased stress and anxiety, only 10 (5%) used mental health counseling services. A vast majority of the participants (n=189, 97%) presumed that other students were experiencing similar stress and anxiety because of COVID-19. As shown in Figure 2 , at least 54% (up to 91% for some categories) of participants indicated negative impacts (either mild, moderate, or severe) of COVID-19 on academic-, health-, and lifestyle-related outcomes. The qualitative analysis yielded two to five themes for each category of outcomes. The chronic health conditions category was excluded from the qualitative analysis due to insufficient qualitative response. Table 3 presents the description and frequency of the themes and select participant quotes.

a Not every participant provided sufficient elaboration to allow for identification of themes, so the frequency of individual themes does not add up to the total number of participants who indicated negative impacts of the COVID-19 outbreak.
b The five-digit alphanumeric value indicates the participant ID.
c TA: teaching assistant.
Concerns for One’s Own Health and the Health of Loved Ones
A vast majority of the participants (177/195, 91%) indicated that COVID-19 increased the level of fear and worry about their own health and the health of their loved ones. Over one-third of those who showed concern (76/177, 43%) were worried about their families and relatives who were more vulnerable, such as older adults, those with existing health problems, and those who are pregnant or gave birth to a child recently. Some of the participants (26/177, 15%) expressed their worry about their family members whose occupation increased their risk of exposure to COVID-19 such as essential and health care workers. Some participants (19/177, 11%) specifically mentioned that they were worried about contracting the virus.
Difficulty With Concentration
A vast majority of participants (173/195, 89%) indicated difficulty in concentrating on academic work due to various sources of distraction. Nearly half of them (79/173, 46%) mentioned that their home is a distractive environment and a more suitable place to relax rather than to study. Participants mentioned that they were more prone to be interrupted by their family members and household chores at home. Other factors affecting students’ concentration were lack of accountability (21/173, 12%) and social media, internet, and video games (19/173, 11%). Some (18/173, 10%) stated that online classes were subject to distraction due to lack of interactions and prolonged attention to a computer screen. Additionally, monotonous life patterns were mentioned by some to negatively affect concentration on academic work (5/173, 3%).
Disruption to Sleep Patterns
A majority of participants (168/195, 86%) reported disruptions to their sleep patterns caused by the COVID-19 pandemic, with over one-third (38%) reporting such disruptions as severe. Half of students who reported some disruption (84/168, 50%) stated that they tended to stay up later or wake up later than they did before the COVID-19 outbreak. Another disruptive impact brought by the pandemic was irregular sleep patterns such as inconsistent time to go to bed and to wake up from day to day (28/168, 17%). Some (12/168, 7%) reported increased hours of sleep, while others (10/168, 6%) had poor sleep quality.
Increased Social Isolation
A majority of participants answered that the pandemic has increased the level of social isolation (167/195, 86%). Over half of these students (91/167, 54%) indicated that their overall interactions with other people such as friends had decreased significantly. In particular, about one-third (52/167, 31%) shared their worries about a lack of in-person interactions such as face-to-face meetings. Others (9/167, 5%) stated that disruptions to their outdoor activities (eg, jogging, hiking) have affected their mental health.
Concerns About Academic Performance
A majority of participants (159/195, 82%) showed concerns about their academic performance being impacted by the pandemic. The biggest perceived challenge was the transition to online classes (61/159, 38%). In particular, participants stated their concerns about sudden changes in the syllabus, the quality of the classes, technical issues with online applications, and the difficulty of learning online. Many participants (36/159, 23%) were worried about progress in research and class projects because of restrictions put in place to keep social distancing and the lack of physical interactions with other students. Some participants (23/159, 14%) mentioned the uncertainty about their grades under the online learning environment to be a major stressor. Others (12/159, 8%) indicated their reduced motivation to learn and tendency to procrastinate.
Disruptions to Eating Patterns
COVID-19 has also negatively impacted a large portion of participants’ dietary patterns (137/195, 70%). Many (35/137, 26%) stated that the amount of eating has increased, including having more snacks since healthy dietary options were reduced, and others (27/137, 20%) addressed that their eating patterns have become inconsistent because of COVID-19, for example, irregular times of eating and skipping meals. Some students (16/137, 12%) reported decreased appetite, whereas others (7/137, 5%) were experiencing emotional eating or a tendency to eat when bored. On the other hand, some students (28/195, 14%) reported that they were having healthier diets, as they were cooking at home and not eating out as much as they used to.
Changes in the Living Environment
A large portion of the participants (130/195, 67%) described that the pandemic has resulted in significant changes in their living conditions. A majority of these students (89/130, 68%) referred to living with family members as being less independent and the environment to be more distractive. For those who stayed in their residence either on- or off-campus (18/130, 14%), a main change in their living environment was reduced personal interactions with roommates. Some (9/130, 7%) mentioned that staying inside longer due to self-quarantine or shelter-in-place orders was a primary change in their living circumstances.
Financial Difficulties
More than half of the participants (115/195, 59%) expressed their concerns about their financial situations being impacted by COVID-19. Many (44/115, 38%) noted that COVID-19 has impacted or is likely to impact their own current and future employment opportunities such as part-time jobs and internships. Some (21/115, 18%) revealed the financial difficulties of their family members, mostly parents, getting laid off or receiving pay cuts in the wake of COVID-19.
Increased Class Workload
The effect of COVID-19 on class workload among the college students was not conclusive. Although slightly over half of participants (106/195, 54%) indicated their academic workload has increased due to COVID-19, the rest stated the workload has remained the same (70/195, 36%) or rather decreased (19/195, 10%). For those who were experiencing increased workloads, nearly half (51/106, 48%) thought they needed to increase their own efforts to catch up with online classes and class projects given the lack of in-person support from instructors or teaching assistants. About one-third of the participants (33/106, 31%) perceived that assignments had increased or became harder to do. Some (6/106, 6%) found that covering the remainder of coursework as the classes resumed after the 2-week break to be challenging.
Depressive Thoughts
When asked about the impact of the COVID-19 pandemic on depressive thoughts, 44% (86/195) mentioned that they were experiencing some depressive thoughts during the COVID-19 pandemic. Major contributors to such depressive thoughts were loneliness (28/86, 33%), insecurity or uncertainty (10/86, 12%), powerlessness or hopelessness (9/86, 10%), concerns about academic performance (7/86, 8%), and overthinking (4/86, 5%).
Suicidal Thoughts
Out of 195 participants, 16 (8%) stated that the pandemic has led to some suicidal thoughts with 5% (10/16) reporting these thoughts as mild and 3% (6/16) as moderate. There were 6 participants (38%) that attributed their suicidal thoughts to the presence of depressive thoughts. Other reasons were related to academic performance (1/16, 6%), problems with family as they returned home (1/16, 6%), and fear from insecurity and uncertainty (1/16, 6%).
Coping Mechanism During COVID-19
To cope with stress and anxiety imposed by COVID-19, college students reported seeking support from others but were mainly using various self-management methods.
Self-Management
The majority of the participants (105/138, 76%) with increased stress due to the outbreak of COVID-19 explained that they were using various means to help themselves cope with stress and anxiety during the pandemic. Some (24/105, 23%) relied on negative coping methods such as ignoring the news about COVID-19 (10/105), sleeping longer (7/105), distracting themselves by doing other tasks (5/105), and drinking or smoking (2/105). Approximately one-third (30/105, 29%) used positive coping methods such as meditation and breathing exercises (18/105), spiritual measures (7/105), keeping routines (4/105), and positive reframing (2/105). A majority of the participants (73/105, 70%) who used self-management mentioned doing relaxing hobbies including physical exercise (31/105), enjoying streaming services and social media (22/105), playing with pets (7/105), journaling (5/105), listening to music (4/105), reading (2/105), and drawing (2/105). Finally, some participants (15/105, 14%) stated that they were planning activities (eg, drafting to-do lists) for academic work and personal matters as a self-distraction method.
Seeking Support From Others
Approximately one-third of the participants (47/138, 34%) mentioned that communicating with their families and friends was a primary way to deal with stress and anxiety during COVID-19. Some explicitly stated that they were using a virtual meeting application such as Zoom frequently to connect to friends and family. Only 1 participant claimed to be receiving support from a professional therapist, and another participant was using Sanvello, a mobile mental health service app provided by the university.
Barriers to Seeking Professional Support During COVID-19
Despite the availability of tele-counseling and widespread promotion of such services by the university, a vast majority of participants who indicated an increase in stress and anxiety (128/138, 93%) claimed that they had not used school counseling services during the pandemic. Reasons for such low use included the condition not being perceived as severe enough to seek the services (4/128, 3%), not comfortable interacting with unfamiliar people (1/128, 0.8%), not comfortable talking about mental health issues over the phone (1/128, 0.8%), and lack of trust in the counseling services (1/128, 0.8%).
Principal Findings
College students comprise a population that is considered particularly vulnerable to mental health concerns. The findings of this study bring into focus the effects of pandemic-related transitions on the mental health and well-being of this specific population. Our findings suggest a considerable negative impact of the COVID-19 pandemic on a variety of academic-, health-, and lifestyle-related outcomes. By conducting online survey interviews in the midst of the pandemic, we found that a majority of the participants were experiencing increased stress and anxiety due to COVID-19. In addition, results of the PSS showed moderate levels of stress among our participants. This is in line with a recent pre–COVID-19 survey conducted in the United Kingdom (mean PSS score 19.79, SD 6.37) [ 28 ]; however, the administration of PSS as interview questions (compared to allowing participants to read and respond to the 10 questions) might have introduced bias and resulted in underreporting.
Among the effects of the pandemic identified, the most prominent was worries about one’s own health and the health of loved ones, followed by difficulty concentrating. These findings are in line with recent studies in China that also found concerns relating to health of oneself and of family members being highly prevalent among the general population during the pandemic. Difficulty in concentrating, frequently expressed by our participants, has previously been shown to adversely affect students’ confidence in themselves [ 29 ], which has known correlations to increased stress and mental health [ 30 ]. In comparison with stress and anxiety in college students’ general life, it appears that countermeasures put in place against COVID-19, such as shelter-in-place orders and social distancing practices, may have underpinned significant changes in students’ lives. For example, a vast majority of the participants noted changes in social relationships, largely due to limited physical interactions with their families and friends. This is similar to recent findings of deteriorated mental health status among Chinese students [ 10 ] and increased internet search queries on negative thoughts in the United States [ 31 ]. The findings on the impact of the pandemic on sleeping and eating habits are also a cause for concern, as these variables have known correlations with depressive symptoms and anxiety [ 20 ].
Although a majority of participants expressed concerns regarding academic performance, interestingly, almost half of the participants reported lower stress levels related to academic pressure and class workload since the pandemic began. This may be due, in part, to decisions taken by professors and the university to ease the students’ sudden transition to distance learning. For instance, this university allowed students to choose a pass/fail option for each course instead of a regular letter grade. Additionally, actions taken by professors, such as reduced course loads, open book examinations, and other allowances on grading requirements, could also have contributed to alleviating or reducing stress. Although participants who returned to their parental home reported concerns about distractions and independence, students might have benefited from family support and reduced social responsibilities. Therefore, the increased stress due to the pandemic may have been offset, at least to some extent.
Alarmingly, 44% (86/195) of the participants reported experiencing an increased level of depressive thoughts, and 8% (16/195) reported having suicidal thoughts associated with the COVID-19 pandemic. Previous research [ 32 ] reported about 3%-7% of the college student population to have suicidal thoughts outside of the pandemic situation. Furthermore, with the exception of high-burnout categories, depression levels among students, reported in several recent studies [ 33 - 35 ], have varied between 29% and 38%, which may suggest an uptick in pandemic-related depressive symptoms among college students similar to recent studies in China [ 10 , 11 ]. Although our participants specifically mentioned several factors such as feelings of loneliness, powerlessness, as well as financial and academic uncertainties, other outcomes that were perceived to be impacted by the COVID-19 pandemic may also act as contributors to depressive thoughts and suicidal ideation. In particular, both difficulty concentrating and changes in sleeping habits are associated with depression [ 20 , 29 , 36 ].
Our study also identifies several coping mechanisms varying between adaptive and maladaptive behaviors. The maladaptive coping behaviors such as denial and disengagement have been shown to be significant predictors of depression among young adults [ 37 ]. In contrast, adaptive coping such as acceptance and proactive behaviors are known to positively impact mental health. Our findings suggest that the majority of our participants exhibited maladaptive coping behaviors. Identifying students’ coping behavior is important to inform the planning and design of support systems. In this regard, participatory models of intervention development can be used, in which researchers’ and psychologists’ engagement with the target population to adapt interventional programs to their specific context has shown promise [ 37 , 38 ]. For instance, Nastasi et al [ 37 ] used a participatory model to develop culture-specific mental health services for high school students in Sri Lanka. Similar approaches can be adopted to engage college students as well to develop a mental health program that leverages their natural positive coping behaviors and addresses their specific challenges.
Participants described several barriers to seeking help, such as lack of trust in counseling services and low comfort levels in sharing mental health issues with others, which may be indicative of stigma. Perceiving social stigma as a barrier to seeking help and availing counseling services and other support is common among students [ 29 ]. One study showed that only a minor fraction of students who screened positive for a mental health problem actually sought help [ 39 ]. Although overcoming the stigma associated with mental health has been discussed at length, practical ways of mitigating this societal challenge remains a gap [ 40 , 41 ]. Our findings suggest that self-management is preferred by students and should be supported in future work. Digital technologies and telehealth applications have shown some promise to enable self-management of mental health issues [ 42 ]. For instance, Youn et al [ 43 ] successfully used social media networks as a means to reach out to college students and screen for depression by administering a standardized scale, the Patient Health Questionnaire-9. Digital web-based platforms have also been proposed to enhance awareness and communication with care providers to reduce stigma related to mental health among children in underserved communities [ 44 ]. For instance, one of the online modules suggested by the authors involves providing information on community-identified barriers to communicating with care providers. Technologies such as mobile apps and smart wearable sensors can also be leveraged to enable self-management and communication with caregivers.
In light of the aforementioned projections of continued COVID-19 cases at the time of this writing [ 45 ] and our findings, there is a need for immediate attention to and support for students and other vulnerable groups who have mental health issues [ 17 ]. As suggested by a recent study [ 46 ] based on the Italian experience of this pandemic, it is essential to assess the population’s stress levels and psychosocial adjustment to plan for necessary support mechanisms, especially during the recovery phase, as well as for similar events in the future. Although the COVID-19 pandemic seems to have resulted in a widespread forced adoption of telehealth services to deliver psychiatric and mental health support, more research is needed to investigate use beyond COVID-19 as well as to improve preparedness for rapid virtualization of psychiatric counseling or tele-psychiatry [ 47 - 49 ].
Limitations and Future Work
To our knowledge, this is the first effort in documenting the psychological impacts of the COVID-19 pandemic on a representative sample of college students in the United States via a virtual interview survey method in the middle of the pandemic. However, several limitations should be noted. First, the sample size for our interview survey was relatively small compared to typical survey-only studies; however, the survey interview approach affords the capture of elaboration and additional clarifying details, and therefore complements the survey-based approaches of prior studies focusing on student mental health during this pandemic [ 10 , 11 , 50 ]. Second, the sample used is from one large university, and findings may not generalize to all college students. However, given the nationwide similarities in universities transitioning to virtual classes and similar stay-at-home orders, we expect reasonable generalizability of these findings. Additionally, a majority of our participants were from engineering majors. Therefore, future work is needed to use a stratified nationwide sample across wider disciplines to verify and amend these findings. Third, although a vast majority of participants answered that they have not used the university counseling service during the pandemic, only a few of them provided reasons. Since finding specific reasons behind the low use is a key to increasing college students’ uptake of available counseling support, future research is warranted to unveil underlying factors that hinder college students’ access to mental health support. Finally, we did not analyze how student mental health problems differ by demographic characteristics (eg, age, gender, academic year, major) or other personal and social contexts (eg, income, religion, use of substances).
Future work could focus on more deeply probing the relationships between various coping mechanisms and stressors. Additionally, further study is needed to determine the effects of the pandemic on students’ mental health and well-being in its later phases beyond the peak period. As seen in the case of health care workers in the aftermath of the severe acute respiratory syndrome outbreak, there is a possibility that the effects of the pandemic on students may linger for a period beyond the peak of the COVID-19 pandemic itself [ 51 ].
Acknowledgments
This research was partly funded by a Texas A&M University President’s Excellence (X-Grant) award.
Conflicts of Interest
None declared.
- Unger K. Handbook on Supported Education: Providing Services for Students With Psychiatric Disabilities. Charleston, SC: BookSurge Publishing; 2007.
- 2019 annual report. Center for Collegiate Mental Health. University Park, PA: Penn State University; 2020. URL: https://ccmh.memberclicks.net/assets/docs/2019-CCMH-Annual-Report_3.17.20.pdf [accessed 2020-05-11]
- Shuchman M. Falling through the cracks — Virginia Tech and the restructuring of college mental health services. N Engl J Med 2007 Jul 12;357(2):105-110. [ CrossRef ]
- Eisenberg D, Downs MF, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev 2009 Oct;66(5):522-541. [ CrossRef ] [ Medline ]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020 Mar 14;395(10227):912-920 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020 Mar 02;3(3):e203976 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr 2020 Apr 24:e201619 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kirzinger A, Kearney A, Hamel L, Brodie M. KFF health tracking poll - early April 2020: the impact Of coronavirus on life In America. Kaiser Family Foundation. 2020 Apr 02. URL: https://www.kff.org/health-reform/report/kff-health-tracking-poll-early-april-2020/ [accessed 2020-05-10]
- Nelson B, Pettitt A, Flannery J, Allen N. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. Int J Methods in Psychiatr Res 2020 Apr 13;21(3):169-184. [ CrossRef ]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020 May;287:112934 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Liu X, Liu J, Zhong X. Psychological state of college students during COVID-19 epidemic. SSRN J 2020 Mar 24:A. [ CrossRef ]
- Wang C, Zhao H. The impact of COVID-19 on anxiety in Chinese university students. Front Psychol 2020;11:1168. [ CrossRef ] [ Medline ]
- Bruffaerts R, Mortier P, Kiekens G, Auerbach RP, Cuijpers P, Demyttenaere K, et al. Mental health problems in college freshmen: prevalence and academic functioning. J Affect Disord 2018 Jan 01;225:97-103 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhai Y, Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res 2020 Jun;288:113003 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhai Y, Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry 2020 Apr;7(4):e22 [ FREE Full text ] [ CrossRef ] [ Medline ]
- de Oliveira Araújo FJ, de Lima LSA, Cidade PIM, Nobre CB, Neto MLR. Impact of Sars-Cov-2 and its reverberation in global higher education and mental health. Psychiatry Res 2020 Jun;288:112977 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020 Jun;7(6):547-560 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983 Dec;24(4):385-396. [ Medline ]
- Cohen S, Kessler R, Gordon L. Measuring stress: A Guide for Health and Social Scientists. New York, NY: Oxford University Press; 1997.
- Acharya L, Jin L, Collins W. College life is stressful today - emerging stressors and depressive symptoms in college students. J Am Coll Health 2018 Oct;66(7):655-664. [ CrossRef ] [ Medline ]
- Baghurst T, Kelley BC. An examination of stress in college students over the course of a semester. Health Promot Pract 2014 May;15(3):438-447. [ CrossRef ] [ Medline ]
- Zoom. Zoom Video Communications. URL: https://zoom.us/
- Otter.ai. URL: https://otter.ai/login
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol 2006 Jan;3(2):77-101. [ CrossRef ]
- Guest G, MacQueen K, Namey E. Applied Thematic Analysis. Thousand Oaks, CA: Sage Publications; 2011.
- Corbin J, Strauss A. Basics of Qualitative Research (3rd ed.): Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications; 2014.
- MAXQDA. VERBI Software. URL: https://www.maxqda.com/
- Denovan A, Dagnall N, Dhingra K, Grogan S. Evaluating the perceived stress scale among UK university students: implications for stress measurement and management. Stud Higher Education 2017 Jun 22;44(1):120-133. [ CrossRef ]
- Martin JM. Stigma and student mental health in higher education. Higher Education Res Dev 2010 Jun;29(3):259-274. [ CrossRef ]
- Zuckerman DM. Stress, self-esteem, and mental health: how does gender make a difference? Sex Roles 1989 Apr;20(7-8):429-444. [ CrossRef ]
- Jacobson NC, Lekkas D, Price G, Heinz MV, Song M, O'Malley AJ, et al. Flattening the mental health curve: COVID-19 stay-at-home orders are associated with alterations in mental health search behavior in the United States. JMIR Ment Health 2020 Jun 01;7(6):e19347 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zivin K, Eisenberg D, Gollust SE, Golberstein E. Persistence of mental health problems and needs in a college student population. J Affect Disord 2009 Oct;117(3):180-185. [ CrossRef ] [ Medline ]
- Zeng Y, Wang G, Xie C, Hu X, Reinhardt JD. Prevalence and correlates of depression, anxiety and symptoms of stress in vocational college nursing students from Sichuan, China: a cross-sectional study. Psychol Health Med 2019 Aug;24(7):798-811. [ CrossRef ] [ Medline ]
- Nahas ARMF, Elkalmi R, Al-Shami A, Elsayed T. Prevalence of depression among health sciences students: findings from a public university in Malaysia. J Pharm Bioallied Sci 2019;11(2):170-175 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fitzpatrick O, Biesma R, Conroy RM, McGarvey A. Prevalence and relationship between burnout and depression in our future doctors: a cross-sectional study in a cohort of preclinical and clinical medical students in Ireland. BMJ Open 2019 May 01;9(4):e023297 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Heiligenstein E, Guenther G, Hsu K, Herman K. Depression and academic impairment in college students. J Am Coll Health 1996 Sep;45(2):59-64. [ CrossRef ] [ Medline ]
- Nastasi BK, Sarkar S, Varjas K, Jayasena A. Participatory model of mental health programming: lessons learned from work in a developing country. Sch Psychol Rev 1998;27(2):260-276.
- Cappella E, Jackson DR, Bilal C, Hamre BK, Soulé C. Bridging mental health and education in urban elementary schools: participatory research to inform intervention development. Sch Psychol Rev 2011;40(4):486-508.
- Eisenberg D, Hunt J, Speer N, Zivin K. Mental health service utilization among college students in the United States. J Nerv Ment Dis 2011 May;199(5):301-308. [ CrossRef ] [ Medline ]
- Husain W. Barriers in seeking psychological help: public perception in Pakistan. Community Ment Health J 2020 Jan;56(1):75-78. [ CrossRef ] [ Medline ]
- Fischer EP, McSweeney JC, Wright P, Cheney A, Curran GM, Henderson K, et al. Overcoming barriers to sustained engagement in mental health care: perspectives of rural veterans and providers. J Rural Health 2016 Sep;32(4):429-438. [ CrossRef ] [ Medline ]
- Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health 2020 Mar 26;7(3):e18848 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Youn SJ, Trinh N, Shyu I, Chang T, Fava M, Kvedar J, et al. Using online social media, Facebook, in screening for major depressive disorder among college students. Int J Clin Health Psychol 2013 Jan;13(1):74-80. [ CrossRef ]
- Ginossar T, Nelson S. Reducing the health and digital divides: a model for using community-based participatory research approach to e-health interventions in low-income Hispanic communities. J Computer-Mediated Commun 2010;15(4):530-551. [ CrossRef ]
- COVID-19 projections. Institute for Health Metrics and Evaluation. Seattle, WA: University of Washington URL: https://covid19.healthdata.org/united-states-of-america [accessed 2020-05-20]
- de Girolamo G, Cerveri G, Clerici M, Monzani E, Spinogatti F, Starace F, et al. Mental health in the coronavirus disease 2019 emergency-the Italian response. JAMA Psychiatry 2020 Apr 30:A. [ CrossRef ] [ Medline ]
- Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry 2020 Jul 01;177(7):574-575. [ CrossRef ] [ Medline ]
- Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health 2020 Apr;26(4):377-379. [ CrossRef ] [ Medline ]
- Shore JH, Waugh M, Calderone J, Donahue A, Rodriguez J, Peters D, et al. Evaluation of telepsychiatry-enabled perinatal integrated care. Psychiatr Serv 2020 May 01;71(5):427-432. [ CrossRef ] [ Medline ]
- Huckins JF, daSilva AW, Wang W, Hedlund E, Rogers C, Nepal SK, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res 2020 Jun 17;22(6):e20185 [ FREE Full text ] [ CrossRef ] [ Medline ]
- McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry 2007 Apr;52(4):241-247. [ CrossRef ] [ Medline ]
Abbreviations
Edited by G Eysenbach, G Fagherazzi, J Torous; submitted 10.06.20; peer-reviewed by T Liu, V Hagger; comments to author 28.07.20; revised version received 01.08.20; accepted 15.08.20; published 03.09.20
©Changwon Son, Sudeep Hegde, Alec Smith, Xiaomei Wang, Farzan Sasangohar. Originally published in the Journal of Medical Internet Research (http://www.jmir.org), 03.09.2020.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on http://www.jmir.org/, as well as this copyright and license information must be included.
News & Articles

Malta: Increasing mental health literacy among secondary school students and educators

The Ministry for Education, Sports, Youth, Research and Innovation (MEYR) in Malta, through the People Management Department and in collaboration with the Commissioner for Mental Health and Richmond Foundation, embarked on a 3-year-long project aimed at increasing mental health literacy (MHL) among secondary school educators and students.
The project involved training 20% of state secondary school educators in Youth Mental Health (YMHFA) and training all Year 9 students (13-14-year-olds) each scholastic year in teen Mental Health First Aid (tMHFA). YMHFA is a mental health literacy (MHL) programme designed for adults working with young people whilst tMHFA is a school-based universal programme that aims to increase student supportive behaviours towards peers, MHL and beliefs about help and support available.
During the scholastic year 2022-2023, 2561 students were trained in tMHFA and during the scholastic year 2023-2024, 2450 students benefited from the training. Over the two scholastic years 328 educators were trained in YMHFA. The current 3-year programme will continue up until the school year 2024-2025, during which a further 2554 Year 9 students will be trained in tMHFA and a further 119 educators will be trained in YMHFA.
Source: Eurydice Unit Malta
Latest News and Articles

Spain has introduced new national programmes aimed at improving student competence in mathematics and reading comprehension. The Ministry of Education has allocated nearly €95 million

The Ministry for Education, Sports, Youth, Research and Innovation (MEYR) in Malta, through the People Management Department and in collaboration with the Commissioner for Mental

As the world is becoming increasingly innovative and technologically advanced, rapid adaptation to new challenges is essential. Vocational education and training (VET) plays a pivotal

A draft resolution of the Council of Ministers on the establishment of the Digital Transformation Policy for Education has been submitted for public consultation, and
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
research@BSPH
The School’s research endeavors aim to improve the public’s health in the U.S. and throughout the world.
- Funding Opportunities and Support
- Faculty Innovation Award Winners
Conducting Research That Addresses Public Health Issues Worldwide
Systematic and rigorous inquiry allows us to discover the fundamental mechanisms and causes of disease and disparities. At our Office of Research ( research@BSPH), we translate that knowledge to develop, evaluate, and disseminate treatment and prevention strategies and inform public health practice. Research along this entire spectrum represents a fundamental mission of the Johns Hopkins Bloomberg School of Public Health.
From laboratories at Baltimore’s Wolfe Street building, to Bangladesh maternity wards in densely packed neighborhoods, to field studies in rural Botswana, Bloomberg School faculty lead research that directly addresses the most critical public health issues worldwide. Research spans from molecules to societies and relies on methodologies as diverse as bench science and epidemiology. That research is translated into impact, from discovering ways to eliminate malaria, increase healthy behavior, reduce the toll of chronic disease, improve the health of mothers and infants, or change the biology of aging.
120+ countries
engaged in research activity by BSPH faculty and teams.
of all federal grants and contracts awarded to schools of public health are awarded to BSPH.
citations on publications where BSPH was listed in the authors' affiliation in 2019-2023.
publications where BSPH was listed in the authors' affiliation in 2019-2023.
Departments
Our 10 departments offer faculty and students the flexibility to focus on a variety of public health disciplines
Centers and Institutes Directory
Our 80+ Centers and Institutes provide a unique combination of breadth and depth, and rich opportunities for collaboration
Institutional Review Board (IRB)
The Institutional Review Board (IRB) oversees two IRBs registered with the U.S. Office of Human Research Protections, IRB X and IRB FC, which meet weekly to review human subjects research applications for Bloomberg School faculty and students
Generosity helps our community think outside the traditional boundaries of public health, working across disciplines and industries, to translate research into innovative health interventions and practices
Introducing the research@BSPH Ecosystem
The research@BSPH ecosystem aims to foster an interdependent sense of community among faculty researchers, their research teams, administration, and staff that leverages knowledge and develops shared responses to challenges. The ultimate goal is to work collectively to reduce administrative and bureaucratic barriers related to conducting experiments, recruiting participants, analyzing data, hiring staff, and more, so that faculty can focus on their core academic pursuits.
Research at the Bloomberg School is a team sport.
In order to provide extensive guidance, infrastructure, and support in pursuit of its research mission, research@BSPH employs three core areas: strategy and development, implementation and impact, and integrity and oversight. Our exceptional research teams comprised of faculty, postdoctoral fellows, students, and committed staff are united in our collaborative, collegial, and entrepreneurial approach to problem solving. T he Bloomberg School ensures that our research is accomplished according to the highest ethical standards and complies with all regulatory requirements. In addition to our institutional review board (IRB) which provides oversight for human subjects research, basic science studies employee techniques to ensure the reproducibility of research.
Research@BSPH in the News
Four bloomberg school faculty elected to national academy of medicine.
Considered one of the highest honors in the fields of health and medicine, NAM membership recognizes outstanding professional achievements and commitment to service.
The Maryland Maternal Health Innovation Program Grant Renewed with Johns Hopkins
Lerner center for public health advocacy announces inaugural sommer klag advocacy impact award winners.
Bloomberg School faculty Nadia Akseer and Cass Crifasi selected winners at Advocacy Impact Awards Pitch Competition
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Stress and the Mental Health of Populations of Color:Advancing Our Understanding of Race-related Stressors
David r williams , phd, mph.
- Author information
- Copyright and License information
Corresponding Author David R. Williams, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, 677 Huntington Avenue, 6 th Floor, Boston, MA 02115, [email protected]
This article provides an overview of research on race-related stressors that can affect the mental health of socially disadvantaged racial and ethnic populations. It begins by reviewing the research on self-reported discrimination and mental health. Although discrimination is the most studied aspect of racism, racism can also affect mental health through structural/institutional mechanisms and racism that is deeply embedded in the larger culture. Key priorities for research include more systematic attention to stress-proliferation processes due to institutional racism, the assessment of stressful experiences linked to natural or manmade environmental crises, documenting and understanding the health effects of hostility against immigrants and people of color, cataloguing and quantifying protective resources, and enhancing our understanding of the complex association between physical and mental health.
Keywords: race, stress, racial discrimination, racism, mental health, mental disorders
There is considerable complexity in the association between race and mental health. The patterning of racial differences in mental health appear to vary by indicator of mental health status. For several decades, research has shown that while blacks (or African Americans) often have higher rates of psychological distress than whites, some studies also find that whites have elevated levels of depressive and anxiety symptoms compared to blacks ( Dohrenwend 1969 , Vega and Rumbaut 1991 ). Blacks tend to report lower levels of psychological well-being on cognitively focused measures such as life satisfaction and happiness ( Hughes and Thomas 1998 ), but also report higher levels of flourishing than whites ( Keyes 2007 ). Flourishing refers to the absence of mental disorders and the presence of high levels of psychological well-being. With regards to defined psychiatric disorders, Hispanics (or Latinos),with the exception of Puerto Ricans, blacks, and Asians all have lower rates of lifetime and past year psychiatric disorders than whites ( Miranda et al. 2008 ). However, when blacks and Latinos experience mental illness, their episodes tend to be are more severe, persist for longer periods of time, and are more debilitating than for any other race/ethnic group ( Breslau et al. 2005 ). For example, in the national Study of American Life (NSAL), African Americans and Caribbean Blacks had lower current and lifetime rates of major depression than whites ( Williams et al. 2007 ). However, once depressed, both black groups were more likely than whites to be chronically or persistently depressed, have more severe symptoms, higher levels of impairment, and not receive treatment.
We do not currently have a clear sense of either the determinants of the levels of mental health status for the major racial/ethnic groups in the U.S. or the patterning of the various indicators of mental health status for all of these minority populations. However, there is broad agreement that social contextual factors that reflect exposure to chronic and acute stressors linked to the living and working conditions of these populations play a role in shaping their mental health risk ( Pearlin et al. 2005 , Turner 2013 , Vega and Rumbaut 1991 ). Historically, the assessment of stressful life experiences was heavily driven by the stressors experienced by middle class white males. There has been enormous scientific interest and effort in recent decades in conceptualizing and measuring the stressors that may be distinctive to, or more prevalent among, socially stigmatized racial and ethnic minority populations and how these stressors can affect their physical and mental health. These stressors are viewed as interconnected and driven by exposures in social contexts, structures, and roles ( Pearlin et al. 1981 ). This article provides an overview of research that suggests that the mental health of racial/ethnic socially stigmatized populations is embedded in these larger contextual factors. It begins with an overview of the research on racial discrimination and health and then situates this research in the need to more clearly document the other pathways by which racism can also adversely affect mental health.
Racial Discrimination and Mental Health
In recent decades, research on racial discrimination and mental health has been a rapidly growing area of scientific investigation. However, racial discrimination is best understood as one of the pathways by which racism affects health ( Williams and Mohammed 2013 ). The term “racism” refers to an organized system that is premised on the categorization and ranking of societal groups into races ( Bonilla-Silva 1996 ). The dominant group devalues, disempowers, and differentially allocates desirable societal opportunities and resources to racial groups categorized as inferior. Supporting and buttressing the structure of racism is an ideology that is deeply embedded in the culture of the society, that provides the rationale for the ranking of groups. This leads to the development of negative attitudes and beliefs toward racial out-groups (prejudice and stereotypes), and differential treatment (discrimination) of these groups by both individuals and social institutions. There is a large body of high quality scientific evidence that documents the persistence of racial discrimination in employment, housing, banking and other commercial transactions, and a broad range of domains of life ( Pager and Shepherd 2008 ).
Targets of discrimination are aware of at least some of these incidents of bias and they are often experienced as stressors that can adversely affect mental and physical health. Historically, such experiences had not been included in the typical scales used to assess acute and chronic stress. Considerable evidence now suggests that these experiences are commonplace in contemporary society. For example, a recent national survey assessed discrimination both as acute major experiences (e.g., not being hired for a job or being unfairly harassed by the police) and as chronic, minor experiences captured by the Everyday Discrimination scale (e.g., being treated with less courtesy and respect than others and receiving poorer service in restaurants and stores) ( American Psychological Association 2016 ). This study found that 69% of American adults reported experiencing at least one experience of discrimination and 61% reported experiencing everyday discrimination. Importantly these experiences were patterned by race. For example, 35% of African Americans and Native Americans, 25% of Latinos, 22% of Asians, and 18% of whites reported that they had had an experience of being unfairly not being hired for a job. Similarly, 34% of American Indians, 23% of blacks, 19% of Hispanics, and 11% of Asians and non-Hispanic whites reported that they experienced Everyday Discrimination almost every day or at least once a week ( American Psychological Association 2016 ).
Early Empirical Research on Racial Discrimination
Early studies of discrimination and health found that self-report measures of discrimination were inversely associated with good mental and physical health. Reviews of this early literature revealed that most studies were cross-sectional, most assessed mental health outcomes or other self-reported indicators of health, and most focused on African American adults in the U.S. ( Krieger 1999 , Williams, Neighbors and Jackson 2003 ). Although these findings were consistent with the notion that experiences of discrimination were neglected psychosocial stressors, there were serious scientific limitations. There was the possibility of shared response bias between self-reported measures of discrimination and self-reported measures of health in cross-sectional analyses. It was possible that mentally ill individuals could be (mis-)perceiving discrimination that did not even exist. There was also concern that key psychological confounding factors such as social desirability, negative affect, neuroticism, or self-esteem could drive the observed associations.
Subsequent research has addressed these methodological concerns. An important early study analyzed longitudinal data from 779 black adults in the National Study of Black Americans (NSBA) ( Brown et al. 2000 ). This study found that psychological distress and diagnosed major depression at Wave 2 (1987–1988) were unrelated to reports of discrimination at Wave 3 (1988–1989), indicating that poor mental health did not predict subsequent reports of discrimination. The study also found that racial discrimination at Wave 2 was positively associated with psychological distress, but not depression, at Wave 3. Although the majority of studies of discrimination and health are still cross-sectional, there are a growing number of prospective studies that link changes over time in discrimination to increases in symptoms of distress and depression ( Lewis, Cogburn and Williams 2015 , Paradies et al. 2015 , Pascoe and Richman 2009 , Schulz et al. 2006 , Wallace, Nazroo and Bécares 2016 , Williams and Mohammed 2009 ). Personality traits are not routinely included as potential confounders in studies of self-reported discrimination. However, several studies have found that the association between discrimination and health remains robust after adjustment for personality characteristics such as hostility, neuroticism, social desirability, negative affect, and trait anxiety ( Lewis, Cogburn and Williams 2015 , Williams and Mohammed 2009 ). Research has also documented that discrimination is associated with a broad range of disease states (e.g., cancer, cardiovascular disease, diabetes) and preclinical indicators of disease (e.g., allostatic load, inflammation, shorter telomere length, BMI, incident obesity, coronary artery calcification, cortisol dysregulation, and oxidative stress) that are not assessed via self-report ( Lewis, Cogburn and Williams 2015 , Paradies et al. 2015 ).
Recent Empirical Research on Discrimination and Mental Health - Adults
A recent review documented that discrimination is positively associated with measures of depression and anxiety symptoms and psychological distress, as well as, with defined psychiatric disorders ( Lewis, Cogburn and Williams 2015 ). For example, in the NSAL, among African American and Caribbean Black adults 55 years and older, positive but small associations were evident between both racial and non-racial every day discrimination and the risk of any lifetime (LT) disorder, as well as LT mood, and anxiety disorders. Discrimination was also associated with a small increased risk of depressive symptoms and serious psychological distress ( Mouzon et al. 2017 ). Similarly, in the National Latino and Asian American Study (NLAAS), Everyday Discrimination was associated, in multivariate models, with increased odds of any DSM-IV disorder (Odds Ratio [OR] = 1.90), depressive disorder (OR=1.72), and anxiety disorder (OR=2.24) among Asian Americans ( Gee et al. 2007 ). Discrimination was also associated with comorbidity. Compared to persons with no disorders, Everyday Discrimination was associated with a 2-fold risk of having two disorders and a 3-fold risk of having three or more disorders. This pattern in the overall sample of Asian Americans was similar to that observed among the subset who were immigrants. In the NLAAS and NSAL national studies, among Latino, Asian, African Americans, and Caribbean Black adults, Everyday Discrimination was positively associated with both 12-month (OR=4.59) and lifetime psychotic experiences (OR=4.27) ( Oh et al. 2014 ). This pattern was evident for visual (OR=3.75) and auditory (OR=5.65) hallucinatory experiences as well as for delusional ideation (OR=7.21).
Discrimination has also been associated with increased risk of mental disorders in international contexts. For example, in the national South Africa Study of Stress and Health, acute and chronic nonracial discrimination were moderately associated with elevated risk of 12-month and lifetime rates of any disorder, even after adjustment for other stressors and potentially confounding psychological factors ( Moomal et al. 2009 ). For example, chronic everyday non-racial discrimination was associated with increased risk of lifetime mood (OR=1.68), anxiety (OR=1.94), and substance use disorders (OR=1.72) in the fully adjusted models. The UK Household Longitudinal Study also assessed discrimination in four domains and related those exposures to changes in mental health from wave one to wave three ( Wallace, Nazroo and Bécares 2016 ). It found a dose-response relationship between the number of experiences of discrimination with the degree of deterioration in mental health over time, as measured by a scale of psychological distress. The study found that those participants who had reported only one prior experience of discrimination had greater deterioration in mental health (1.93 points lower on a scale of psychological distress) than those who reported none. Those who reported two or more experiences of discrimination at one prior time point had even greater mental health deterioration (2.98 points lower). The level of mental health decline further increased for those who reported two or more experiences of discrimination at one time point and one incident at the other time point (5.65 points lower), with the greatest degree of mental health deterioration evident among those who reported two or more experiences of discrimination at both time points (8.26 points lower).
Based on in-depth qualitative interviews, Fleming and colleagues conclude that incidents of racial discrimination matter so profoundly for mental health because they are experiences of exclusion that trigger feelings of a ‘defilement of self’ ( Fleming, Lamont and Welburn 2012 ). This includes feelings of being over-scrutinized, overlooked, underappreciated, misunderstood and, disrespected. Importantly, experiences of discrimination violate cultural expectations of fairness, morality, dignity, and rights. Pearlin and colleagues (2005) had earlier argued that stressors linked to race may be especially pathogenic because they could be perceived as a direct attack on an individual’s identity.
Most studies of discrimination and health have not explored the role of discrimination in contributing to racial disparities in health. However, a few studies in the U.S. and internationally have documented that perceived discrimination makes an incremental contribution over SES in accounting for racial/ethnic inequities in mental health and self-reported measures of physical health. This is evident for measures of distress and global measures of mental and physical health in community and national studies in the U.S. ( Pole et al. 2005 , Ren, Amick and Williams 1999 , Williams et al. 1997 ). This has also been observed, in national data from New Zealand, for Maori-European disparities on a global measure of mental health and three other indicators of self-reported health ( Harris et al. 2006 ). A similar pattern has been documented in Australia for Aboriginal–non Aboriginal variations in self- reported mental and physical health ( Larson et al. 2007 ). A national study in South Africa also found that experiences of discrimination were positively related to psychological distress and reduced the residual association between race and distress after adjustment had been made for SES ( Williams et al. 2008 ).
Empirical Research on Discrimination and Mental Health – Children and Adolescents
Research reveals that exposure to discrimination and its negative consequences for mental health begins early in life. A review of research of discrimination among children and adolescents found 121 studies (and 461 outcomes) that had examined the association between discrimination and health among persons zero to 18 years old ( Priest et al. 2013 ). Exposure to discrimination predicted worse mental health (e.g., anxiety and depression symptoms) in 76% of the 127 associations examined. Similarly, discrimination was inversely associated with positive mental health (e.g., resilience, self-worth, self-esteem) in 62% of the 108 associations examined. As in studies of adults, most studies are cross-sectional, but there is also an emerging body of longitudinal research. For example, a study in rural Georgia of 714 black adolescents, aged 10–12 at baseline, assessed their exposure to discrimination three times over the next five years ( Brody et al. 2006 ). It found that increases in racial discrimination were associated with conduct problems and depressive symptoms, with the association between discrimination and conduct problems stronger for boys but no gender difference evident for depressive symptoms.
Several studies in this review documented that parental exposure to discrimination can adversely affect the child. For example, a study of black adolescents found that parental racial discrimination was associated with symptoms of anxiety and depression in the child, independent of the child’s experiences of racial discrimination ( Gibbons et al. 2004 ). In this study, parental experiences of discrimination were also associated with substance use in children that was mediated by both parental and child anxiety and depression ( Gibbons et al. 2004 ). Another study of 10 and 11 year olds found that mother reports of racial discrimination were associated with poor parental mental health, which in turn adversely affected parenting behaviors and parenting satisfaction ( Murry et al. 2001 ).
A large study in the U.K., the Millennium Cohort Study, examined, longitudinally, the pathways by which maternal discrimination among Ethnic Minority mothers can affect four domains of social and emotional behavior in children—conduct, peer problems, emotional symptoms, and hyperactivity ( Becares, Nazroo and Kelly 2015 ). The study found that adjusted for socio-demographic factors and mother’s mental health in the year 2006, there were three pathways by which maternal racial/ethnic discrimination in 2006 were associated with children’s social and emotional behavior in 2012. First, maternal discrimination in 2006 directly predicted child outcomes in 2012. In addition, mother’s discrimination in 2006 was associated with poorer maternal mental health and harsh parenting practices in 2008, and both of these factors were associated with child social and emotional development in 2012.
A recent systematic review documented how children can often be the unintended victims of discrimination because of their links to other individuals ( Heard-Garris et al. 2018 ). This review found 30 studies that had examined the association between vicarious discrimination (secondhand exposure to racism) and child health. Most of the studies were longitudinal and had been published after 2011. Two-thirds of the studies focused on African Americans in urban areas of the U.S., but there were also studies of Asian Americans, Hispanics, whites, and indigenous groups in Australia, New Zealand, and the U.S. Socio-emotional and mental health outcomes were most frequently assessed, and the review found that in almost half of the examined associations, indirect exposure to racism by children was inversely related to child health. There is clearly a need for sustained research attention that would comprehensively characterize both direct and indirect exposure to discrimination and document how these experiences accumulate over the life course to affect the onset and course of illness ( Gee, Walsemann and Brondolo 2012 , Heard-Garris et al. 2018 ). Greater attention needs to be given in future research to identifying sensitive periods, the interdependence in exposures among persons, latency periods, stress proliferation processes, and effects that may be linked to historical period and birth cohort ( Gee, Walsemann and Brondolo 2012 ).
Vigilance and the Threat of Exposure to Discrimination
Discrimination, like other stressors, can affect health through both actual exposure and the threat of exposure. Heightened vigilance refers to living in a state of psychological arousal in order to monitor, respond to, and attempt to protect oneself from threats linked to potential experiences of discrimination and other dangers in one’s immediate environment ( Williams, Lavizzo-Mourey and Warren 1994 ). The Heightened Vigilance scale was developed as a companion measure to the Everyday Discrimination scale and seeks to capture efforts to protect oneself from discrimination and minimize exposure ( Williams et al. 1997 ) Studies with this scale or abbreviated versions of it highlight the importance of assessing the health consequences of race-related vigilance. Research reveals that race-related vigilance is positively associated with large arterial elasticity (a preclinical index of cardiovascular function) for African American boys but not girls ( Clark, Benkert and Flack 2006 ), the risk of sleep difficulties and racial disparities in sleep ( Hicken et al. 2013 ), the odds of hypertension for blacks and Hispanics but not Whites and the racial gap in hypertension ( Hicken et al. 2014 ), and waist circumference and BMI among black women ( Hicken, Lee and Hing 2018 ).
Vigilance also matters for mental health. A study of Baltimore adults found that blacks have higher levels of heightened vigilance than whites, and vigilance was positively associated with depressive symptoms and contributed to the black-white disparity in depression ( LaVeist et al. 2014 ). Similarly, Lindstrom (2008) found that a single-item measure of anticipatory ethnic discrimination was associated with lower levels of psychological health in a national sample of adults in Sweden. A study of Latino college students also found that the anticipation of being discriminated against led to greater concern and threat emotions before an encounter with a potential perpetrator of discrimination and more stress and greater cardiovascular responses after the encounter ( Sawyer et al. 2012 ). Our current understanding is limited with regard to all of the contexts and conditions that give rise to perceptions of threat, the optimal ways to assess vigilance with regards to discrimination, and the ways in which vigilance combines with other risk factors to affect mental health.
Discrimination and Other Stressors
Discrimination must be understood and assessed within the context of other mechanisms of racism. Social disadvantages and stressors often cluster in people and places. In addition, institutional/structural racism can give rise to what Pearlin and colleagues (2005) called stress proliferation processes, in which an initial stressor can initiate or exacerbate stressors in other domains of life. Thus, living and working conditions created by racism can initiate and sustain differential exposure to a broad range of stressors that, at face value, may not appear to be related to racism. These can include “traditional stressors” such as violence, criminal victimization, neighborhood conditions, financial stress, and relationship stress. According to Pearlin and colleagues, these are the “serious stressors,” patterned by social disadvantage, that capture major hardships, conflicts, and disruptions in life, and are especially virulent when they are chronic and recur in major social roles and domains ( Pearlin et al. 2005 ).
An example of the comprehensive assessment of stressors comes from the Chicago Community Adult Health Study. This study measured stressors in eight domains that reflect key arenas in which people operate (e.g., home, work, neighborhood) and major roles/statuses they occupy ( Sternthal, Slopen and Williams 2011 ). The stressors included a brief battery of acute life events (lifetime traumatic experiences and recent life events), childhood adversity, chronic stressors in relationships, finances, neighborhoods and at work, and acute and chronic life experiences of discrimination (Everyday Discrimination, discrimination at work and major experiences of discrimination). Blacks and American-born Hispanics tended to have higher prevalence of each of the individual classes of stressors, and greater clustering of multiple stressors, compared to whites. The analyses found that each stressor was positively associated with depressive symptoms, in models that considered all eight stressors simultaneously. Moreover, in models that counted the number of domains in which an individual scored high on stress, the study found a graded association between the number of stressors and an increase in depressive symptoms. In addition, the study found that the association between SES (especially income) and depressive symptoms was reduced substantially after coefficients for stress were added to the model, suggesting that stress exposure operates apart from SES but also through exposure to stressors that accompany low SES ( Sternthal, Slopen and Williams 2011 ).
However, research attention is needed to fully characterize the ways in which institutional mechanisms of racism shape exposure to stressors. For example, residential racial segregation is recognized as one of the most striking and consequential legacies of institutional racism that has pervasive negative effects on living conditions and health ( Williams and Collins 2001 ). It is a major contributor to racial differences in income, education, and employment, and the concentration of poverty, isolation, marginalization, and other social ills that tend to co-occur with segregation ( Cutler and Glaeser 1997 , Williams and Collins 2001 ). However, prior assessments of stressors have failed to fully capture all of the stress inducing aspects of what Chester Pierce called the “extreme mundane environment” of disadvantaged neighborhoods ( Pierce 1975 ).
A recent qualitative study of Baltimore residents who resided in public housing illustrates how segregation can create the concentration of poverty and poor housing and neighborhood conditions that trigger a range of acute and chronic secondary stressors ( Turney, Kissane and Edin 2013 ). The study found that residents were exposed to high levels of stressors linked to the social environment, including pervasive witnessing shootings, seeing drug activity, resorting to violence to defend oneself, high levels of break-ins and theft, incessant shouting and cursing, undesirable role models for children, unsafe places to raise children, and the resultant constant worry about child safety. In addition, stressors linked to the physical environment included broken elevators, roach and rodent infestation, trash buildup, dampness in the walls, extremely hot (or cold) interior temperatures, the absence of green open spaces, crumbling sidewalks, graffiti, litter, and inadequate lighting. It is not clear that existing batteries to capture acute and chronic stressors capture all of these aspects of stressful exposures. This is important because failure to measure stress comprehensively underestimates the negative effects of stressors on physical and mental health ( Thoits 2010 ).
Comprehensively capturing the full mental health impact of exposure to discrimination requires careful attention to the changing nature of racism in society and assessing it in all of the contexts where it becomes evident. Research on discrimination in online contexts illustrates this point. A recent study of Latino adolescents found that both individual online discrimination (derogatory text, images, and symbols directly targeted at individuals because of their race and ethnicity) and vicarious online discrimination (derogatory incidents targeted to people of one’s own racial or ethnic group) were adversely related to adolescent mental health ( Umaña-Taylor et al. 2015 ).
Capturing “Hidden” Aspects of Race-Related Stressors on Mental Health
A related need is to give more systematic attention to understanding how some life experiences that are not explicitly linked to racism can indeed reflect the effects of racism, and to better document their contribution to mental health. For example, the death of a loved one is a standard indicator of stress on scales of life events, but the ways in which such exposures are driven by the larger racism in the society is not typically understood and appreciated. Deborah Umberson’s (2017) research on community bereavement illustrates the value of this approach. She shows that structural conditions linked to racism lead to lower life expectancy for African Americans. A consequence of the large racial differences in life expectancy is that compared to whites, black Americans are exposed to more deaths of friends and relatives from early childhood through late life and to more losses earlier in the life course. For example, compared with whites, black children are three times as likely to lose a mother by age 10, and black adults are more than twice as likely to lose a child by age 30, and a spouse by age 60. Umberson indicates that this elevated rate of bereavement and loss of social ties is a unique stressor that adversely affects levels of supportive social ties and mental (and physical health) across the life course ( Umberson 2017 ).
The Criminal Justice system has also been identified as an instrument of institutional racism, a societal system that generates policies and procedures that have differential negative effects on stigmatized racial ethnic populations. Emerging evidence suggests that policies within this system that have differential impact on racial groups are an example of institutional racism. With approximately 700 per 100,000 citizens incarcerated at any given time, the United States has the largest number and rate of incarcerated people in the world ( Wildeman and Wang 2017 ). The rates of incarceration increased dramatically in the 1970s. Disparities in surveillance, prosecution, and sentencing have been associated with a 10-fold increase in risk of incarceration for non-Hispanic blacks compared to white men in the United States, often reinforced by policies which have differentially criminalized substance abuse and mental illness ( Wildeman and Wang 2017 ).
One factor contributing to the marked increase in incarceration rates for racial minorities was the laws that linked criminal penalties for cocaine to an arbitrary distinction of whether cocaine was used in powder form or as crack-cocaine, the cheaper, solid, adulterated version of the former. The 1986 Anti-Drug Abuse Act created a 100:1 sentence disparity—a mandatory minimum prison sentence of five years for a defendant possessing five grams of crack cocaine (primarily used by blacks) or 500 grams of powder cocaine (primarily used by whites) ( Free Jr. 1997 ). Thus, despite similar rates of cocaine use among black and white Americans and despite crack and powder cocaine having the same chemical make-up and similar physiologic effects, black people were more likely to be charged for drug possession and to serve markedly longer prison sentences than whites ( Free Jr. 1997 ).
Incarceration, in turn, has negative ripple effects on mental health for families and communities. Paternal incarceration is associated with poorer school outcomes and increases in aggressive behaviors, problematic externalizing and internalizing behaviors in their children ( Wildeman, Goldman and Turney 2018 ). In contrast, there is not a consistent association between maternal incarceration and mental health and school outcomes. Factors that exacerbate the effects of parental incarceration include the presence of domestic violence, parental residence in the home before incarceration, child sex being male, and child race being white. Some studies have also quantified the impact of parental incarceration on racial disparities in child health and well-being ( Wildeman, Goldman and Turney 2018 ). These studies reveal that mass incarceration has increased racial inequities in children’s behavioral and mental health problems by 15% to 25% for externalizing problems and by 24% to 46% for internalizing problems. In addition, the black-white disparity in infant mortality would be 10% lower if mass incarceration did not exist.
Aggressive policing can also adversely affect the mental health of those targeted and the larger community. A study in New York City of 1261 young men aged 18 to 26 years assessed whether and how many times they had been stopped by the police, and what had occurred during the encounter ( Geller et al. 2014 ). The study found that the frequency of stops, the intrusiveness of the encounter, and the perception of injustice and disrespect in the encounter were all positively associated with symptoms of PTSD and anxiety. These associations were robust after adjustment for race, education, public housing residence, and criminal activity.
There are also frequent media reports of incidents of police violence directed towards black, Latino, and Native American communities, and there is emerging evidence that the steady drumbeat and reminders of these police shootings can be chronic stressors that adversely affect the mental health of the larger community. A recent nationally-representative, quasi-experimental study, found that police killings of unarmed black Americans worsened mental health among blacks in the general population but had no effect on whites ( Bor et al. 2018 ). The effect was not evident for police shootings of armed black men. Each police killing led to a per capita increase of.14 poor mental health days per month in the three months after the event. At the population level, police killings of unarmed black Americans resulted in 55 million poor mental health days annually in the black American community.
Other evidence indicates that witnessing community violence is also a risk factor for mental health problems ( Clark et al. 2008 ). A study of 386 women receiving care at an urban health center reported on the location and timing of witnessing incidents of violence in their neighborhoods. The study found that women who witnessed violence in their community were twice as likely to report depressive and anxiety symptoms compared to those who reported no violence (adjusted for marital status, age, education, and IPV victimization). There is also an emerging body of evidence that suggests that there may be a complex pattern of association between the stressor of community violence and mental health, at least for male adolescents of color ( Gaylord-Harden et al. 2017a , Gaylord-Harden et al. 2017b ). In longitudinal studies of African American and Latino male adolescents in Chicago, this research has found that higher levels of exposure to community violence is positively associated with aggression, delinquency, and PTSD symptoms such as hyperarousal. However, the association between violence and depressive symptoms is curvilinear, with depressive symptoms increasing only up to a point, then beginning to decline. The authors suggest that youth of color may become emotionally desensitized to community violence as violence increases. Moreover, both emotional numbing and physiological arousal mediate the association between violence exposure and aggressive and delinquent behavior in these adolescent males. Future research needs to explore the extent to which these patterns are generalizable to other population subgroups and the extent to which community violence is a unique stressor in terms of its effect on mental health and behavior.
Cultural Racism and Mental Health
Research also reveals that racism is deeply embedded in American culture and can contribute to adversely affecting mental health in multiple ways ( Williams and Mohammed 2013 ). One indicator of the persistence of racism in the culture is the high levels of negative stereotypes in the population. A recent national study documented that it is not only adult members of disadvantaged racial/ethnic groups that are stereotyped negatively, but even young children (aged 0 to 8 years) and youth of color in the U.S. face high levels of negative racial stereotyping from adults who work with them ( Priest et al. 2018 ). The study analyzed the stereotypes held by white adults who work or volunteer with children across the U.S., examining their reported views towards adults, teenagers, and children from a range of racial and ethnic backgrounds (blacks, Hispanics, whites, Native Americans, Asians, and Arab Americans). The study found high levels of negative racial stereotyping towards non-Whites of all ages, among adults working or volunteering with children. The highest levels of negative stereotypes were found towards blacks across all stereotypes measured (lazy, unintelligent, violent, and having unhealthy habits), with Native Americans and Hispanics seen as similarly negative on several stereotypes.
Negative stereotyping by whites were most pronounced towards adults, but were seen even towards young children. For example, young black children (aged 0–8 years) were almost three times more likely as white adults to be rated as being lazy, with Native American and Hispanic children also more likely to be considered lazy than white adults. Young black children were more than twice as likely to be rated as unintelligent or violence-prone compared to white children of the same age, with Hispanic children also seen as more unintelligent or violence-prone than White children. Some of the strongest levels of negative stereotyping by white adults working with children were reported towards teenagers, with black and Native American teens being almost ten times as likely to be viewed as lazy as white adults. African American and Hispanic teens were between one and a half to two times more likely to be considered violence-prone and unintelligent than white adults and teens.
Provider Biases and Access and Quality of Care
Cultural racism can trigger unconscious bias that can result in reduced access to health enhancing opportunities and resources for non-dominant racial/ethnic groups. This has been well-documented in the case of medical care, including mental health care. Research reveals that high levels of negative stereotypes, through normal, subtle and often subconscious processes, can guide expectations and interactions with others in ways that reduce the quality of service provided by mental health professionals to persons who belong to stigmatized social groups ( American Psychological Assocation Presidential Task Force on Preventing Discrimination and Promoting Diversity 2012 ). Importantly, even the most well-meaning and consciously egalitarian individual who holds a negative stereotype of a social group will likely discriminate against a member of that group when s/he has an encounter with that individual. These are universal processes and all persons are capable of them.
Considerable scientific research indicates that these processes affect the care provided by physicians and other clinicians. A landmark 2003 report from the National Academy of Medicine concluded that across virtually every type of medical intervention, from the most simple to the most sophisticated, blacks and other minorities receive fewer procedures and poorer quality medical care than whites ( Smedley, Stith and Nelson 2003 ). Most physicians, like other professionals and ordinary Americans, have an implicit preference for whites over blacks ( Sabin et al. 2009 ), and this implicit bias among providers is often associated with biased treatment recommendations in the care of black and other minority patients ( van Ryn et al. 2011 ). Provider implicit bias is also associated with poorer quality of patient provider communication and lower patient evaluation of the quality of the medical encounter including provider nonverbal behavior ( Cooper et al. 2012 , van Ryn et al. 2011 ).
For example, a study of 422 patients independently observed over five years in a psychiatric emergency room (ER) illustrates how race can play a role in mental health care ( Segal, Bola and Watson 1996 ). The study found that after adjusting for psychotic disorders, severity of disturbance, dangerousness, psychiatric history, use of restraints, time spent in ER, and other factors, compared to other patients, black patients received, on average, one additional dose of psychiatric medication, one additional anti-psychotic dose and an additional half dose of anti-psychotic medication by injection. In addition, clinicians spent less time to evaluate a black patient than a white one, and the tendency to overmedicate black patients was lower when clinicians’ efforts to engage the patient in treatment (e.g. elicit information, include patient in planning, respond with empathy) were rated as higher.
A recent phone-based experimental study documented discrimination by race, gender, and class in getting access to mental health care ( Kugelmass 2016 ). As part of the study, 326 licensed psychotherapists in New York city received a voice mail message from a black middle-class and a white middle-class individual or from a black and white working-class person seeking an appointment. Each message used a racially distinctive name and a race- and class-based speech pattern. The study found that middle-class seekers were offered appointments at a rate almost three times higher than their working-class peers. Among the middle-class, whites were more likely than blacks to get appointments. And among middle class males, white males were more than twice as likely to get an appointment than their black counterparts. Appointment offer rates did not differ by gender, but women were more likely than men to get an offer of an appointment during their preferred time range. Future research needs to quantify the contribution of provider biases to the well-documented patterns of racial and ethnic inequities in seeking mental health care, engagement with treatment, and in the severity and course of disease.
Internalized Racism
Internalized racism (or internalized stigma or self-stereotyping) is another pathway by which cultural racism can harm mental health. It refers to the acceptance and personal endorsement, by marginalized racial populations, of the negative societal beliefs and stereotypes about the inherent deficiencies of one’s group in the larger society. Thus, the normative cultural characterization of the superiority of whiteness and the devaluing of non-white groups can lead to the perception of self as worthless and lower self-esteem and psychological well-being in stigmatized groups and have broad negative effects on mental health by adversely affecting identity, self-competence, and health behaviors ( Kwate and Meyer 2011 ).
Several studies have empirically examined the association of internalized racism and mental health. The Nandanolitization scale was an early measure of internalized racism ( Taylor and Grundy 1996 ). It captures the extent to which blacks are socially uncomfortable with other blacks and endorse traditional racist stereotypes of blacks such as blacks are mentally defective (intellectually, morally, emotionally) or blacks are physically gifted (athletically, sexually, artistically). Research by Jerome Taylor and colleagues revealed that internalized racism was associated with higher consumption of alcohol and higher levels of psychological distress and depressive symptoms ( Taylor and Jackson 1990 , Taylor, Henderson and Jackson 1991 , Taylor and Jackson 1991 ).
In the National Survey of Black Americans (NSBA), internalized racism was assessed by capturing the degree of agreement with positive and negative stereotypes of black people. A study of the 2,107 black American adults in that sample found that both the rejection of positive stereotypes and the endorsement of negative stereotypes were associated with lower levels of self-esteem ( Brown, Sellers and Gomez 2002 ). More recently, the NSAL has also measured internalized racism by capturing the extent to which blacks endorse negative stereotypes of blacks. One study found that African Americans who had high levels of racial identity but also scored high on internalized racism were more likely to have lower levels of mastery and higher levels of depressive symptoms ( Hughes et al. 2015 ). Another study using this same sample found that internalized racism was positively associated with depressive symptoms and serious psychological distress among African Americans, U.S.-born Caribbean Blacks, and foreign-born Caribbean Blacks ( Mouzon and McLean 2017 ). However, African Americans had the highest levels of internalized racism, followed by U.S.-born Caribbean Blacks, and then foreign-born Caribbean Blacks, and the association with mental health symptoms was weakest for the foreign-born group. Another study using the NSAL data found, surprisingly, that among Caribbean Blacks, but not African Americans, internalized racism was associated with a reduced risk of having major depressive disorder in the past year ( Molina and James 2016 ).
The internalization of negative cultural images by stigmatized groups may also create expectations, anxieties, and reactions that can adversely affect not only psychological wellbeing but also decrease motivation for socioeconomic attainment ( Kwate and Meyer 2011 ). Research in the U.S. reveals that when a stigma of inferiority was activated under experimental conditions, student performance on an examination was adversely affected ( Steele 1997 ). African Americans who were told in advance that blacks perform more poorly on exams than whites, women who were told that they perform more poorly than men, and white men who were told that they usually do worse than Asians, all had lower scores on an examination than control groups who were not confronted with a stigma of inferiority ( Fischer et al. 1996 , Steele 1997 ). Limited scientific evidence also indicates that the presence of stereotype threat in the encounter of a minority patient with a provider may adversely affect the quality of interaction with the provider and patient adherence to medical recommendations ( Aronson et al. 2013 ). This may be especially important in the context of mental health care where the quality of patient-provider interpersonal interaction can be a critical contributor to the quality of the therapeutic relationship.
Unlike the case of discrimination and health, research on internalized racism and mental health is in its infancy. At the present time, we are unaware of the optimal assessment of internalized racism and of the mechanisms and processes by which this type of racism adversely affects mental health. However, it is urgent that future research addresses this gap, given that studies with the Nandanolitization scale using non-representative community and student samples have estimated that one in three blacks score high on internalized racism ( Taylor and Grundy 1996 ). A similar estimate comes from a study of Indigenous adults in Australia in which internalized racism was measured by a four-item scale that captured agreement with not feeling good about being Indigenous, wanting Indigenous people to think and act more like other Australians, disagreeing that Indigenous people have fewer opportunities than other Australians, and reporting not being accepted by other Indigenous people ( Paradies and Cunningham 2009 ). The study found that one third of Aboriginal adults had high levels of internalized racism. We are also not clear about the factors that increase the likelihood that processes of internalized racism are triggered. For example, research reveals that exposure of American Indians to mascots can adversely affect a sense of self-esteem and community worth ( Fryberg et al. 2008 ). Future research needs to identify the extent to which processes of internalized racism are operative within this context or if there are other processes linked to cultural racism that are at work.
Other Key Priorities for Future Research
There are a number of emerging mental risks that require more systematic attention in order to identify and effectively address current and future sources of stress and mental health challenges for populations of color. These include hostility and stress in the current political environment, the complex relationships between mental health and physical health, the mental health consequences of climate change and other emerging environmental risks, identifying sources of psychological resilience, and understanding and confronting patterns of increased mental health risks.
Hostility and Stress in the Larger Culture
There is an urgent need to quantify and better understand the mental health consequences of stressors linked to the increasing levels of racial hostility and political polarization in recent years. The election of President Barack Obama played a critical role. A review of research on this topic revealed that his election led to the rise of the Tea Party movement with its racist rhetoric, declining white support for the Democratic party, and increases in the belief among whites that racism no longer exists, that was combined with opposition to efforts to address racial inequities ( Parker 2016 ). His election also triggered a large increase in racial animosity in social media that included the emergence of anti-Obama Facebook pages, hate websites, and the proliferation online of historical racial stereotypes that are no longer utilized in most mainstream media outlets ( Moody 2012 ). The campaign of Donald Trump further brought to the surface pre-existing negative attitudes towards immigrants, Muslims, and racial and ethnic minorities. A national but non-representative survey of 2,000 Kindergarten through grade 12 teachers documented that more than a half of them indicated that since the Trump presidential campaign had begun, there had been an increase among some of their students in using slurs, name-calling, and saying bigoted and hostile things about immigrants, minorities, and Muslims, and many students in these targeted groups were afraid and worried about potential negative effects on their families after the election ( Costello 2016 ). For example, some African American children whose families had been in the U.S. for centuries were concerned about a return to slavery and black people being sent back to Africa.
And in the wake of Trump’s election there was a marked spike in hate crimes and harassment with K-12 schools being the most commonly reported location where these incidents of harassment had occurred ( Lenz, 2016 ). This hostility in the larger environment contributed to high levels of fear and stress in the population. A national survey conducted by the American Psychological Association in January 2017 reported that two-thirds of all American adults said that they were stressed about the future of the country. Moreover, 69% of blacks, 57% of Asians, 56% of Hispanics, and 42% of non-Hispanic Whites reported that the outcome of the 2016 presidential election was a “very significant” or “somewhat significant” source of stress ( American Psychological Association 2017 ). Some 72% of Democrats and 26% of Republicans were similarly stressed. Recent studies have documented that residing in communities with high levels of racial prejudice is associated with an elevated risk of mortality, especially for racial minorities who reside in those communities ( Chae et al. 2015 , Lee et al. 2015 , Leitner et al. 2016 ). Similarly, elevated mortality risk has been found among lesbian, gay and bisexual individuals living in areas with high levels of anti-gay prejudice ( Hatzenbuehler et al. 2014 ). However, inadequate research attention has been given to documenting the short-term and long-term mental health consequences of residence in hostile environments.
Relatedly, research also suggests that anti-immigrant policies and initiatives can trigger hostility toward immigrants that can lead to perceptions of vulnerability, fear, and psychological distress for both immigrants who are directly targeted and those who are not direct targets ( Szkupinski Quiroga, Medina and Glick 2014 ). A study in Arizona documented that this hostility in the environment led to reductions in the use of health care and social services among Hispanic women, with the effect being larger among Latinas who were U.S. born than among those who were foreign-born ( Toomey et al. 2014 ). Descriptions of federal immigration raids also suggest that they can have negative emotional effects on an entire community ( Novak, Geronimus and Martinez-Cardoso 2017 ). A recent study documented that a large immigration raid at a meat-processing plant was associated with an increase in low birth weight to infants born to Hispanic, but not non-Hispanic white mothers, in that community in the year after the raid compared with infants born in the year before the raid ( Novak, Geronimus and Martinez-Cardoso 2017 ). Similarly, a study in a midwestern U.S. community found that immigration enforcement stressors and levels of self-rated ill health were higher for the Latino community residents who were interviewed after an immigration raid compared to those interviewed before the raid ( Lopez et al. 2017 ). More systematic efforts are needed to document and quantify this stress, fear, and vulnerability, and assess their consequences for mental health. An earlier body of research found that increases in hostility in the media and general society against Muslims and persons from the Middle East in the wake of the September 11, 2011 terrorist attacks were associated with increased risk of low birthweight and preterm birth for Arab American women ( Lauderdale 2006 ) and to elevated levels of mental health symptoms among persons from the Middle East ( Padela and Heisler 2010 ).
Understanding Complex Interactions between Physical Health and Mental Health Risks
Several lines of evidence suggest that among racial minorities, there are complex and sometimes paradoxical associations between mental and physical health that we need to better understand so that we can improve overall health. First, some evidence suggests that psychological resources and positive emotional health can be associated with negative effects on physical health. For example, a study that followed a sample of relatively economically disadvantaged African American adolescents in the rural southeast over time, found that those low SES youth with high self-control and self-regulation at age 11 succeeded academically and emotionally in young adulthood and at age 20 use fewer drugs and drink less alcohol ( Brody et al. 2013 ). However, these same youth had greater obesity, higher blood pressure, and higher levels of stress hormones and epigenetic aging (based on DNA methylation profiles) than their low SES peers who were low on self-control, and than their higher SES peers( Chen et al. 2015 , Miller et al. 2015 ).
Similarly, in the National Longitudinal Study of Adolescent to Adult Health, lower levels of depression are associated with college completion, irrespective of childhood disadvantage and for all racial/ethnic groups (blacks, whites, Hispanics) ( Gaydosh et al. 2018 ). In contrast, college completion is associated with lower metabolic syndrome for whites, irrespective of exposure to childhood disadvantage, but among black and Hispanic youth, college completion is associated with higher metabolic syndrome among those from disadvantaged childhood environments. Future research needs to better understand the contexts and exposures that appear to have opposite effects on mental health versus physical health. One useful framework is John Henryism, or high-effort, active coping, that is a positive attribute among well-resourced racial minorities but is associated with worse health among those who lack the resources to facilitate success (are low SES) or encounter blocked opportunity ( James 1994 ). However, it is unclear how processes linked to John Henryism and blocked opportunity relate to each other and can combine to affect physical and mental health. One national study of African Americans found that education was positively associated with experiences of racial discrimination and both John Henryism and discrimination were associated with the increased odds of major depression, but John Henryism did not moderate the relationship between discrimination and depression ( Hudson et al. 2016 ).
Analyses of longitudinal data also indicate that African American and Hispanic youth who experience upward socioeconomic mobility report greater increases in acute and chronic discrimination compared to their peers whose SES was stable ( Colen et al. 2018 ). These experiences of discrimination are adversely related to health and partially contributed to disparities in health between these minority young adults and their white counterparts. This research is broadly consistent with a larger paradox in the research literature between mental and physical health risks among African Americans. African Americans tend to have worse health than whites on virtually every indicator of physical health, but, as noted earlier, despite higher levels of stress, they have lower rates of stress-related mental health outcomes, such as major depression, than whites. We do not understand what drives this phenomenon. Analyses of national data revealed that lower levels of depression among blacks than whites was evident across virtually every demographic subgroup defined by sex, age, and education—a finding that is not consistent with the view that the observed pattern is due to selection bias because of limited coverage of some subgroups of the black population in surveys due to incarceration or homelessness ( Barnes, Keyes and Bates 2013 ). Other recent analyses have documented that neither high levels of social support among blacks ( Mouzon 2013 ) nor the elevated levels of religious involvement among African Americans compared to whites account for the racial differences in depression ( Mouzon 2017 ). A novel hypothesis to account for this paradox was that engagement in unhealthy behaviors (eating, alcohol and tobacco use) to cope with stress is more protective of depression risk for blacks than whites ( Jackson, Knight and Rafferty 2010 ). Using a large national sample, Keyes and colleagues ( Keyes, Barnes and Bates 2011 ) did not find support for this hypothesis. Engaging in unhealthy behaviors was not associated with reduced risk of depression for blacks or for whites. So the paradox remains as an important scientific question to be answered.
Future research must also pay greater attention to the contribution that mental health symptoms among racial/ethnic minorities may play in the elevated risk of chronic physical conditions. A recent study that pooled data from 16 prospective studies in the U.K. and followed people for about 10 years, found that higher levels of distress were associated with increased risk of cancer of all sites, cancers not related to smoking as well as leukemia and colorectal, prostate, pancreatic, and esophageal cancer ( Batty et al. 2017 ). The associations persisted after adjustment for demographic factors, SES, smoking and alcohol use. A graded stepwise risk was evident between psychological distress and prostate and colorectal cancer. This research highlights the value of sustained research attention that would enable us to better understand how risk and protective factors relate to each other and combine over time to affect physical and mental health and the relationship between them.
Climate Change, Environmental Risks, and Mental Health
As we look to the future, it is also important to give attention to assessing the mental health consequences of the stressors that may emerge from natural and manmade disasters. For example, a monthly survey in Flint, Michigan, during the time of the recent water crisis, found that community respondents reported stress, anxiety, depression and fear within the community due to the ongoing crisis ( Cuthbertson et al. 2016 ). These negative mental health consequences were viewed as being related not only to the actual contamination of the water but also to distrust of the official response to the crisis and the inadequacy of their response ( Cuthbertson et al. 2016 ). Similarly, a review of research on the mental health impact of a devastating earthquake in Japan in 2011 found long-term negative mental health impact for the population affected ( Ando et al. 2017 ). While posttraumatic stress symptoms tended to decline over time, and initial increases in suicide decreased two years after the quake, elevated symptoms of depression persisted during the entire follow-up period. These findings suggest the need for long-term and ongoing mental health support for communities and populations that face high levels of exposure to traumatic experiences.
Climate change is also likely to exacerbate the challenges faced by vulnerable populations and add to their mental health burden. Because of climate change, many cities are likely to get warmer, heat waves are expected to last longer, increase in frequency, and be more intense ( Jesdale, Morello-Frosch and Cushing 2013 ). Prior research has found that there are large racial disparities in heat-related deaths. Urban tree canopy can mitigate the negative effects of extreme heat and urban trees can provide shade, reduce waste water loads, reduce air pollution, and reduce noise pollution. However, disadvantaged SES and racial/ethnic groups are more vulnerable to heat exposure because they are more likely to have higher rates of illness (e.g. CVD, respiratory, renal, diabetes), reside in high crime areas (fear of assault is a barrier to opening windows or traveling to cooler locations), and occupy poorer quality housing ( Gronlund 2014 ). They also have lower access to working fans, cool public spaces, and air conditioning ( Gronlund 2014 ). All of these factors suggest that the mental health burden will be greater for socially disadvantaged racial and ethnic populations. Inadequate attention has been given to examining the short- and long-term mental health impact of natural or manmade environmental crises.
Protective Factors
A few studies have identified psychosocial resources that can reduce the negative effects of the stress of discrimination on mental health. Religious involvement has reduced the negative effects of discrimination on health in two national studies. In prospective analyses using data from the NSBA, higher levels of religious involvement (church attendance, and seeking religious guidance in everyday life) reduced the positive association between racial discrimination and psychological distress ( Ellison, Musick and Henderson 2008 ). In the national MIDUS study, church attendance buffered the adverse effect of discrimination on negative affect among African-Americans but not among Whites ( Bierman 2006 ). In a study of 414 rural low-income black mothers, Church-based social support captured by a 21 item scale that assessed support from one’s relationship with God, with the congregation, and from the clergy, buffered the negative effect of discrimination on depressive symptoms ( Odom, Vernon‐Feagans and Investigators 2010 ). A measure of optimism also reduced the negative effect of discrimination on depression. Relatedly, a study using a 31 item measure of trait mindfulness in a non-representative community sample of 605 adults found that mindfulness reduced the negative effects of discrimination on depressive symptoms ( Brown-Iannuzzi et al. 2014 ).
The receipt of social support from family members and friends is widely recognized as a psychosocial resource that can reduce the negative effects of stressful life experiences on health. A few studies have documented a similar pattern for the stress of discrimination. A study of 714 black adolescents, ages 10–12 at baseline, interviewed three times over five years, found that the negative effects of discrimination on depressive symptoms was reduced among those adolescents who had had high levels of support from their parents and friends ( Brody et al. 2006 ). A subsequent follow-up of this same study found that high levels of social support (caregiver emotional and instrumental support and peer support) reduced the negative effect of discrimination on allostatic load ( Brody et al. 2014 ).
Future research is needed to better understand the conditions under which particular aspects of religious involvement, social support, and psychological resources can reduce the negative effects of the stress of discrimination on mental health. Research is also needed to characterize the full range of resources that might play a role in ameliorating the negative impacts of discrimination on mental health.
Emerging Mental Health Challenges
There is evidence of large and worsening mental health challenges for minority youth. Suicide data is illustrative. Native Americans have the highest rates of suicide. It is the 8 th leading cause of death overall and the second leading cause between the ages of 10 to 34 ( Odafe et al. 2016 ). There are also marked increases in suicide rates among Hispanics, especially among adolescents and young adults. Suicide is the third leading cause of death for blacks aged 15 to 24, and although blacks still have lower suicide rates than whites, an increase in suicide among black youth in recent decades has narrowed the racial gap. A recent study documented that suicide was the leading cause of death among school-aged children aged 5 to 11 years in the U.S. ( Bridge et al. 2015 ). The study found that although overall suicide rates for children aged 5 to 11 years had remained stable between 1993 to 1997 and 2008 to 2012, the rate had declined for whites and remained stable for Hispanics and other racial groups, but had almost doubled for blacks.
More research is needed to identify the determinants of these challenges and identify how they can be effectively addressed. A recent study ( Edwards et al. 2017 ) of 365 emerging adults (96% African American), aged 18 to 24 years old affiliated with a university in a northeastern metro area, sheds light on the significant stressful challenges that youth perceive. The young adults report that their biggest concerns were aggressive policing, high levels of community violence, and the instability of their housing. These youth reported that they faced constant threat and fear, high levels of hopelessness, and low perceived economic opportunity. Accordingly, they lived in the moment because of their uncertainty about their future. Changing the current trajectory of stress and mental health problems will require significant investment in enabling youth to develop skills and resources to confront and cope with the stressors they face.
Understanding the ways in which the social context of populations of color affect their mental health requires detailed and comprehensive characterization of the exposures in their social context that can affect health. The overview of the research provided here highlights the multiple ways in which racism can affect mental health. Other conditions linked to race and ethnicity can also play a role in shaping the mental health of disadvantaged populations, and we need to understand these stressors in their full complexity. Future research must characterize this full range of risk factors and resources that may be unique to, or more prevalent among, stigmatized racial and ethnic populations and identify how they combine with each other, over the life course, to affect patterns of mental health. Such research must be attentive to the changing social context of racial/ethnic status and incorporate emerging threats to mental health as well as opportunities that may arise to promote enhanced mental wellbeing.
Acknowledgments
FUNDING AND ACKNOWLEDGMENTS
Preparation of this paper was supported in part by the National Institute on Minority Health and Health Disparities (NIMHD) of the National Institutes of Health under Award Number R01 MD009719. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health. The author thanks Sandra Krumholz for her assistance in preparing the manuscript.
David R. Williams is the Norman Professor of Public Health, African and African American Studies and Sociology at Harvard University and an Honorary Professor, Department of Psychiatry and Mental Health, University of Cape Town, South Africa. His research focuses on the ways in which socioeconomic status, race, stress, racism and religious involvement can affect health. He is the author of over 400 scholarly papers and is an elected member of the National Academy of Medicine and the American Academy of Arts and Sciences. In 2014, he was ranked as one of the World’s Most Influential Scientific Minds.
- American Psychological Assocation Presidential Task Force on Preventing Discrimination and Promoting Diversity. 2012. “Dual Pathways to a Better America: Preventing Discrimination and Promoting Diversity” Washington, D.C.: American Psychological Association. [ Google Scholar ]
- American Psychological Association. 2016, “Stress in America: The Impact of Discrimination. Stress in America Survey”. Retrieved 2016 ( https://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf ).
- American Psychological Association. 2017, “Stress in America: Coping with Change. Stress in America Survey”. Retrieved February 22, 2017, ( https://www.apa.org/news/press/releases/stress/2016/coping-with-change.PDF ).
- Ando Shuntaro, Kuwabara Hitoshi, Araki Tsuyoshi, Kanehara Akiko, Tanaka Shintaro, Morishima Ryo, Kondo Shinsuke and Kasai Kiyoto. 2017. “Mental Health Problems in a Community after the Great East Japan Earthquake in 2011: A Systematic Review.” Harvard review of psychiatry 25(1):15–28. doi: 10.1097/hrp.0000000000000124. [ DOI ] [ PubMed ] [ Google Scholar ]
- Aronson Joshua, Burgess Diana, Phelan Sean M. and Juarez Lindsay. 2013. “Unhealthy Interactions: The Role of Stereotype Threat in Health Disparities.” American Journal of Public Health 103(1):50–56. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnes David M., Keyes Katherine M. and Bates Lisa M. 2013. “Racial Differences in Depression in the United States: How Do Subgroup Analyses Inform a Paradox?”. Social Psychiatry and Psychiatric Epidemiology 48(12):1941–49. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Batty G. David, Russ Tom C., Stamatakis Emmanuel and Kivimaki Mika. 2017. “Psychological Distress in Relation to Site Specific Cancer Mortality: Pooling of Unpublished Data from 16 Prospective Cohort Studies.” BMJ 356:j108. doi: 10.1136/bmj.j108. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Becares Laia, Nazroo James and Kelly Yvonee. 2015. “A Longitudinal Examination of Maternal, Family, and Area-Level Experiences of Racism on Children’s Socioemotional Development: Patterns and Possible Explanations.” Social Science & Medicine 142:128–35. doi: 10.1016/j.socscimed.2015.08.025. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bierman Alex. 2006. “Does Religion Buffer the Effects of Discrimination on Mental Health? Differing Effects by Race.” Journal for the Scientific Study of Religion 45(4):551–65. [ Google Scholar ]
- Bonilla-Silva Eduardo. 1996. “Rethinking Racism: Toward a Structural Interpretation.” American Sociological Review 62(3):465–80. [ Google Scholar ]
- Bor Jacob, Venkataramani Atheendar S., Williams David R. and Tsai Alexander C. 2018. “Police Killings and Their Spillover Effects on the Mental Health of Black Americans: A Population-Based, Quasi-Experimental Study.” The Lancet 392(10144):302–10. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Breslau Joshua, Kendler Kenneth S., Su Maxwell, Gaxiola-Aguilar Sergio and Kessler Ronald C. 2005. “Lifetime Risk and Persistence of Psychiatric Disorders across Ethnic Groups in the United States.” Psychological Medicine 35(3):317–27. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bridge Jeffrey A., Asti Lindsey, Horowitz Lisa M., Greenhouse Joel B., Fontanella Cynthia A., Sheftall Arielle H., Kelleher Kelly J. and Campo John V. 2015. “Suicide Trends among Elementary School–Aged Children in the United States from 1993 to 2012.” JAMA Pediatrics 169(7):673–77. [ DOI ] [ PubMed ] [ Google Scholar ]
- Brody Gene H., Chen Yi-Fu, Murry Velma McBride, Xiaojia Ge, Simons RL, Gibbons Frederick X., Gerrard Meg and Cutrona Carolyn E. 2006. “Perceived Discrimination and the Adjustment of African American Youths: A Five-Year Longitudinal Analysis with Contextual Moderation Effects.” Child Development 77(5):1170–89. [ DOI ] [ PubMed ] [ Google Scholar ]
- Brody Gene H., Yu Tianyi, Chen Edith, Miller Gregory E., Kogan Steven M. and Beach Steven RH. 2013. “Is Resilience Only Skin Deep? Rural African Americans’ Socioeconomic Status–Related Risk and Competence in Preadolescence and Psychological Adjustment and Allostatic Load at Age 19.” Psychological Science 24(7):1285–93. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brody Gene H., Lei Man-Kit, Chae David H., Yu Tianyi, Kogan Steven M. and Beach Steven R. H. 2014. “Perceived Discrimination among African American Adolescents and Allostatic Load: A Longitudinal Analysis with Buffering Effects.” Child Development 85(3):989–1002. doi: 10.1111/cdev.12213. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown-Iannuzzi Jazmin L., Adair Kathryn C., Payne B. Keith, Richman Laura Smart and Fredrickson Barbara L. 2014. “Discrimination Hurts, but Mindfulness May Help: Trait Mindfulness Moderates the Relationship between Perceived Discrimination and Depressive Symptoms.” Personality and Individual Differences 56:201–05. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown Tony N., Williams David R., Jackson James S., Neighbors Harold W., Torres Myriam, Sellers Sherill L. and Brown Kendrick T. 2000. “Being Black and Feeling Blue: The Mental Health Consequences of Racial Discrimination.” Race and Society 2(2):117–31. [ Google Scholar ]
- Brown Tony N., Sellers Sherrill L. and Gomez John P. 2002. “The Relationship between Internalization and Self-Esteem among Black Adults.” Sociological Focus 35(1):55–71. [ Google Scholar ]
- Chae David H., Clouston Sean, Hatzenbuehler Mark L., Kramer Michael R., Cooper Hannah LF, Wilson Sacoby M., Stephens-Davidowitz Seth I., Gold Robert S. and Link Bruce G. 2015. “Association between an Internet-Based Measure of Area Racism and Black Mortality.” PloS one 10(4):e0122963. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen Edith, Miller Gregory E., Brody Gene H. and Lei ManKit. 2015. “Neighborhood Poverty, College Attendance, and Diverging Profiles of Substance Use and Allostatic Load in Rural African American Youth.” Clinical Psychological Science 3(5):675–85. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Clark Cheryl, Ryan Louise, Kawachi Ichiro, Canner Marina, Berkman Lisa and Wright Rosalind. 2008. “Witnessing Community Violence in Residential Neighborhoods: A Mental Health Hazard for Urban Women.” Journal of Urban Health 85(1):22–38. doi: 10.1007/s11524-007-9229-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Clark Rodney, Benkert Ramona A. and Flack John M. 2006. “Large Arterial Elasticity Varies as a Function of Gender and Racism-Related Vigilance in Black Youth.” Journal of Adolescent Health 39(4):562–69. [ DOI ] [ PubMed ] [ Google Scholar ]
- Colen Cynthia G., Ramey David M., Cooksey Elizabeth C. and Williams David R. 2018. “Racial Disparities in Health among Nonpoor African Americans and Hispanics: The Role of Acute and Chronic Discrimination.” Social Science & Medicine 199:167–80. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cooper Lisa A., Roter Debra L., Carson Kathryn A., Mary Catherine Beach Janice A. Sabin, Greenwald Anthony G. and Inui Thomas S. 2012. “The Associations of Clinicians’ Implicit Attitudes About Race with Medical Visit Communication and Patient Ratings of Interpersonal Care.” American Journal of Public Health 102(5):979–87. doi: 10.2105/ajph.2011.300558. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Costello Maureen B. 2016, “The Trump Effect: The Impact of the Presidential Campaign on Our Nation’s Schools”, Montgomery, AL: Southern Poverty Law Center; Retrieved 2016, ( https://www.splcenter.org/sites/default/files/splc_the_trump_effect.pdf .) [ Google Scholar ]
- Cuthbertson Courtney A., Newkirk Cathy, Ilardo Joan, Loveridge Scott and Skidmore Mark. 2016. “Angry, Scared, and Unsure: Mental Health Consequences of Contaminated Water in Flint, Michigan.” Journal of Urban Health: Bulletin of the New York Academy of Medicine 93(6):899–908. doi: 10.1007/s11524-016-0089-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cutler David M. and Glaeser Edward L. 1997. “Are Ghettos Good or Bad?”. The Quarterly Journal of Economics 112(3):827–72. [ Google Scholar ]
- Dohrenwend Bruce P. Dohrenwend Barbara S. 1969. Social Status and Psychological Disorder: A Casual Inquiry. New York: Wiley. [ Google Scholar ]
- Edwards Lorece V., Lindong Ian, Brown Lawrence, Hawkins Anita S., Dennis Sabriya, Fajobi Olaoluwa, Rowel Randolph, Braithwaite Ronald and Sydnor Kim D. 2017. “None of Us Will Get out of Here Alive: The Intersection of Perceived Risk for Hiv, Risk Behaviors and Survival Expectations among African American Emerging Adults.” Journal of Health Care for the Poor and Underserved 28(2):48–68. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ellison Christopher G., Musick Marc A. and Henderson Andrea K. 2008. “Balm in Gilead: Racism, Religious Involvement, and Psychological Distress among African‐American Adults.” Journal for the Scientific Study of Religion 47(2):291–309. [ Google Scholar ]
- Fischer Claude S., Hout Michael, Jankowski Martín Sánchezs, Lucas Samuel R., Swidler Ann and Voss Kim 1996. Inequality by Design: Cracking the Bell Curve Myth. Princeton, NJ: Princeton University Press. [ Google Scholar ]
- Fleming Crystal M., Lamont Michèle and Welburn Jessica S. 2012. “African Americans Respond to Stigmatization: The Meanings and Salience of Confronting, Deflecting Conflict, Educating the Ignorant and ‘Managing the Self’.” Ethnic and Racial Studies 35(3):400–17. [ Google Scholar ]
- Free Marvin D Jr. 1997. “The Impact of Federal Sentencing Reforms on African Americans.” Journal of Black Studies 28(2):268–86. [ Google Scholar ]
- Fryberg Stephanie A., Markus Hazel Rose, Oyserman Daphna and Stone Joseph M. 2008. “Of Warrior Chiefs and Indian Princesses: The Psychological Consequences of American Indian Mascots.” Basic and Applied Social Psychology 30(3):208–18. [ Google Scholar ]
- Gaydosh Lauren, Schorpp Kristen M., Chen Edith, Miller Gregory E. and Harris Kathleen Mullan 2018. “College Completion Predicts Lower Depression but Higher Metabolic Syndrome among Disadvantaged Minorities in Young Adulthood.” Proceedings of the National Academy of Sciences 115(1):109–14. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gaylord-Harden Noni K., So Suzanna, Bai Grace J., Henry David B. and Tolan Patrick H. 2017a. “Examining the Pathologic Adaptation Model of Community Violence Exposure in Male Adolescents of Color.” Journal of Clinical Child & Adolescent Psychology 46(1):125–35. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gaylord-Harden Noni K., So Suzanna, Bai Grace J. and Tolan Patrick H. 2017b. “Examining the Effects of Emotional and Cognitive Desensitization to Community Violence Exposure in Male Adolescents of Color.” American Journal of Orthopsychiatry 87(4):463–73. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gee Gilbert C., Spencer Michael, Chen Juan, Yip Tiffany and Takeuchi David T. 2007. “The Association between Self-Reported Racial Discrimination and 12-Month Dsm-Iv Mental Disorders among Asian Americans Nationwide.” Social Science & Medicine 64(10):1984–96. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gee Gilbert C., Walsemann Katrina M. and Brondolo Elizabeth 2012. “A Life Course Perspective on How Racism May Be Related to Health Inequities.” American Journal of Public Health 102(5):967–74. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Geller Amanda, Fagan Jeffrey, Tyler Tom and Link Bruce G. 2014. “Aggressive Policing and the Mental Health of Young Urban Men.” American Journal of Public Health 104(12):2321–27. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gibbons Frederick X., Gerrard Meg, Cleveland Michael J., Wills Thomas A. and Brody Gene 2004. “Perceived Discrimination and Substance Use in African American Parents and Their Children: A Panel Study.” Journal of Personality and Social Psychology 86(4):517–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gronlund Carina J. 2014. “Racial and Socioeconomic Disparities in Heat-Related Health Effects and Their Mechanisms: A Review.” Current Epidemiology Reports 1(3):165–73. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harris Ricci, Tobias Martin, Jeffreys Mona, Waldegrave Kiri, Karlsen Saffron and Nazroo James 2006. “Effects of Self-Reported Racial Discrimination and Deprivation on Maori Health and Inequalities in New Zealand: Cross-Sectional Study.” Lancet 367(9527):2005–9. doi: 10.1016/S0140-6736(06)68890-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hatzenbuehler Mark L., Bellatorre Anna, Lee Yeonjin, Finch Brian K., Muennig Peter and Fiscella Kevin 2014. “Structural Stigma and All-Cause Mortality in Sexual Minority Populations.” Social Science & Medicine 103:33–41. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Heard-Garris NJ, Cale M, Camaj L, Hamati MC and Dominguez TP 2018. “Transmitting Trauma: A Systematic Review of Vicarious Racism and Child Health.” Social Science & Medicine 199:230–40. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hicken Margaret T., Lee Hedwig, Ailshire Jennifer, Burgard Sarah A. and Williams David R. 2013. ““Every Shut Eye, Ain’t Sleep”: The Role of Racism-Related Vigilance in Racial/Ethnic Disparities in Sleep Difficulty.” Race and Social Problems 5(2):100–12. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hicken Margaret T., Lee Hedwig, Morenoff Jeffrey, House James S. and Williams David R. 2014. “Racial/Ethnic Disparities in Hypertension Prevalence: Reconsidering the Role of Chronic Stress.” American Journal of Public Health 104(1):117–23. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hicken Margaret T., Lee Hedwig and Hing Anna K. 2018. “The Weight of Racism: Vigilance and Racial Inequalities in Weight-Related Measures.” Social Science & Medicine 199:157–66. doi: 10.1016/j.socscimed.2017.03.058. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hudson Darrell L., Neighbors Harold W., Geronimus Arline T. and Jackson James S. 2016. “Racial Discrimination, John Henryism, and Depression among African Americans.” Journal of Black Psychology 42(3):221–43. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hughes Michael and Thomas Melvin E. 1998. “The Continuing Significance of Race Revisited: A Study of Race, Class, and Quality of Life in America, 1972 to 1996.” American Sociological Review 63:785–95. [ PubMed ] [ Google Scholar ]
- Hughes Michael, Kiecolt K. Jill, Keith Verna M. and Demo David H. 2015. “Racial Identity and Well-Being among African Americans.” Social Psychology Quarterly 78(1):25–48. [ Google Scholar ]
- Jackson James S., Knight Katherine M. and Rafferty Jane A. 2010. “Race and Unhealthy Behaviors: Chronic Stress, the Hpa Axis, and Physical and Mental Health Disparities over the Life Course.” American Journal of Public Health 100(5):933–9. doi: 10.2105/ajph.2008.143446. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- James Sherman A. 1994. “John Henryism and the Health of African-Americans.” Culture, Medicine and Psychiatry 18(2):163–82. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jesdale Bill M., Morello-Frosch Rachel and Cushing Lara 2013. “The Racial/Ethnic Distribution of Heat Risk–Related Land Cover in Relation to Residential Segregation.” Environmental Health Perspectives 121(7):811–17. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Keyes Corey LM 2007. “Promoting and Protecting Mental Health as Flourishing: A Complementary Strategy for Improving National Mental Health.” American Psychologist 62(2):95–108. [ DOI ] [ PubMed ] [ Google Scholar ]
- Keyes Katherine M., Barnes David M. and Bates Lisa M. 2011. “Stress, Coping, and Depression: Testing a New Hypothesis in a Prospectively Studied General Population Sample of U.S.-Born Whites and Blacks.” Social Science & Medicine 72(5):650–9. doi: 10.1016/j.socscimed.2010.12.005. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Krieger Nancy 1999. “Embodying Inequality: A Review of Concepts, Measures, and Methods for Studying Health Consequences of Discrimination.” International Journal of Health Services 29(2):295–352. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kugelmass Heather 2016. ““Sorry, I’m Not Accepting New Patients” an Audit Study of Access to Mental Health Care.” Journal of Health and Social Behavior 57(2):168–83. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kwate Naa Oyo A. and Meyer Ilan H. 2011. “On Sticks and Stones and Broken Bones: Stereotypes and African American Health.” Du Bois Review: Social Science Research on Race 8(1):191–98. doi: doi: 10.1017/S1742058X11000014. [ DOI ] [ Google Scholar ]
- Larson Ann, Gillies Marisa, Howard Peter J. and Coffin Juli 2007. “It’s Enough to Make You Sick: The Impact of Racism on the Health of Aboriginal Australians.” Australian and New Zealand Journal of Public Health 31(4):322–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lauderdale Diane S. 2006. “Birth Outcomes for Arabic-Named Women in California before and after September 11.” Demography 43(1):185–201. [ DOI ] [ PubMed ] [ Google Scholar ]
- LaVeist Thomas A., Thorpe Roland J. Jr., Pierre Geraldine, Mance GiShawn A. and Williams David R. 2014. “The Relationships among Vigilant Coping Style, Race, and Depression.” Journal of Social Issues 70(2):241–55. doi: 10.1111/josi.12058. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee Yoenjin, Muennig Peter, Kawachi Ichiro and Hatzenbuehler Mark L. 2015. “Effects of Racial Prejudice on the Health of Communities: A Multilevel Survival Analysis.” American Journal of Public Health 105(11):2349–55. doi: 10.2105/ajph.2015.302776. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leitner Jordan B., Hehman Eric, Ayduk Ozlem and Mendoza-Denton Rodolfo 2016. “Blacks’ Death Rate Due to Circulatory Diseases Is Positively Related to Whites’ Explicit Racial Bias: A Nationwide Investigation Using Project Implicit.” Psychological Science 27(10):1299–311. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lenz Ryan “Neo-Nazi Andrew Anglin Cheers on Anti-Muslim Harassment as Reports of Attacks Mount": Southern Poverty Law Center; Retrieved November 10, 2016, ( https://www.splcenter.org/hatewatch/2016/11/10/neo-nazi-andrew-anglin-cheers-anti-muslim-harassment-reports-attacks-mount .) [ Google Scholar ]
- Lewis Tené T., Cogburn Courtney D. and Williams David R. 2015. “Self-Reported Experiences of Discrimination and Health: Scientific Advances, Ongoing Controversies, and Emerging Issues.” Annual review of clinical psychology 11:407–40. doi: 10.1146/annurev-clinpsy-032814-112728. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lindström Martin 2008. “Social Capital, Anticipated Ethnic Discrimination and Self-Reported Psychological Health: A Population-Based Study.” Social Science & Medicine 66(1):1–13. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lopez William D., Kruger Daniel J., Delva Jorge, Llanes Mikel, Ledón Charo, Waller Adreanne, Harner Melanie, Martinez Ramiro, Sanders Laura, Harner Margaret and Israel Barbara 2017. “Health Implications of an Immigration Raid: Findings from a Latino Community in the Midwestern United States.” Journal of Immigrant and Minority Health 19:702–08. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miller Gregory E., Yu Tianyi, Chen Edith and Brody Gene H. 2015. “Self-Control Forecasts Better Psychosocial Outcomes but Faster Epigenetic Aging in Low-Ses Youth.” Proceedings of the National Academy of Sciences 112(33):10325–30. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miranda Jeanne, McGuire Tomas G., Williams David R. and Wang Philip 2008. “Mental Health in the Context of Health Disparities.” American Journal of Psychiatry 165(9):1102–8. doi: 10.1176/appi.ajp.2008.08030333 [ DOI ] [ PubMed ] [ Google Scholar ]
- Molina Kristine M. and James Drexler 2016. “Discrimination, Internalized Racism, and Depression: A Comparative Study of African American and Afro-Caribbean Adults in the Us.” Group Processes & Intergroup Relations 19(4):439–61. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moody Mia 2012. “New Media-Same Stereotypes: An Analysis of Social Media Depictions of President Barack Obama and Michelle Obama.” The Journal of New Media & Culture 8(1):1–23. [ Google Scholar ]
- Moomal Hashim, Jackson Pamela B., Stein Dan. J., Herman Allen, Myer Landon, Seedat Soraya, Madela-Mntla Edith and Williams David R. 2009. “Perceived Discrimination and Mental Health Disorders: The South African Stress and Health Study.” South African Medical Journal 99(5 Pt 2):383–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mouzon Dawne M. 2013. “Can Family Relationships Explain the Race Paradox in Mental Health?”. Journal of Marriage and Family 75(2):470–85. [ Google Scholar ]
- Mouzon Dawne M. 2017. “Religious Involvement and the Black–White Paradox in Mental Health.” Race and Social Problems 9(1):63–78. [ Google Scholar ]
- Mouzon Dawne M. and McLean Jamila S. 2017. “Internalized Racism and Mental Health among African-Americans, Us-Born Caribbean Blacks, and Foreign-Born Caribbean Blacks.” Ethnicity & Health 22(1):36–48. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mouzon Dawne M., Taylor Robert Joseph, Keith Verna M., Nicklett Emily J. and Chatters Linda M. 2017. “Discrimination and Psychiatric Disorders among Older African Americans.” International Journal of Geriatric Psychiatry 32(2):175–82. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Murry Velma McBride, Bynum Mia S., Brody Gene H., Willert Amanda and Stephens Dionne 2001. “African American Single Mothers and Children in Context: A Review of Studies on Risk and Resilience.” Clinical Child and Family Psychology Review 4(2):133–55. [ DOI ] [ PubMed ] [ Google Scholar ]
- Novak Nicole L., Geronimus Arline T. and Martinez-Cardoso Aresha M. 2017. “Change in Birth Outcomes among Infants Born to Latina Mothers after a Major Immigration Raid.” International journal of epidemiology 46(3):839–49. doi: 10.1093/ije/dyw346. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Odafe Mary O., Talavera David C., Cheref Soumia, Hong Judy H. and Walker Rheeda L. 2016. “Suicide in Racial and Ethnic Minority Adults: A Review of the Last Decade.” Current Psychiatry Reviews 12(2):181–98. [ Google Scholar ]
- Odom Erica C., Vernon‐Feagans Lynne and Family Life Project Key Investigators. 2010. “Buffers of Racial Discrimination: Links with Depression among Rural African American Mothers.” Journal of Marriage and Family 72(2):346–59. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Oh Hans, Yang Lawrence H., Anglin Deidre M. and DeVylder Jordan E. 2014. “Perceived Discrimination and Psychotic Experiences across Multiple Ethnic Groups in the United States.” Schizophrenia Research 157(1–3):259–65. doi: 10.1016/j.schres.2014.04.036. [ DOI ] [ PubMed ] [ Google Scholar ]
- Padela Aasim I. and Heisler Michele 2010. “The Association of Perceived Abuse and Discrimination after September 11, 2001, with Psychological Distress, Level of Happiness, and Health Status among Arab Americans.” American Journal of Public Health 100(2):284–91. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pager Devah and Shepherd Hana 2008. “The Sociology of Discrimination: Racial Discrimination in Employment, Housing, Credit, and Consumer Markets.” Annual Review of Sociology 34:181–209. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Paradies Yin and Cunningham Joan 2009. “Experiences of Racism among Urban Indigenous Australians: Findings from the Druid Study.” Ethnic and Racial Studies 32(3):548–73. [ Google Scholar ]
- Paradies Yin, Ben Jehonathan, Denson Nida, Elias Amanuel, Priest Naomi, Pieterse Alex, Gupta Arpana, Kelaher Margaret and Gee Gilbert 2015. “Racism as a Determinant of Health: A Systematic Review and Meta-Analysis.” PloS one 10(9):e0138511. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Parker Christopher Sebastian 2016. “Race and Politics in the Age of Obama.” Annual Review of Sociology 42:217–30. [ Google Scholar ]
- Pascoe Elizabeth A. and Richman Laura S. 2009. “Perceived Discrimination and Health: A Meta-Analytic Review.” Psychological Bulletin 135(4):531–54. doi: 10.1037/a0016059. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pearlin Leonard I., Menaghan Elizabeth G., Lieberman Morton A. and Mullan Joseph T. 1981. “The Stress Process.” Journal of Health and Social Behavior 22:337–56. [ PubMed ] [ Google Scholar ]
- Pearlin Leonard I., Schieman Scott, Fazio Elena M. and Meersman Stephen C. 2005. “Stress, Health, and the Life Course: Some Conceptual Perspectives.” Journal of Health and Social Behavior 46(June):205–19. [ DOI ] [ PubMed ] [ Google Scholar ]
- Pierce Chester M. 1975. “The Ghetto: An Extreme Sleep Environment.” Journal of the National Medical Association 67(2):162. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pole Nnamdi, Best Suzanne R., Metsler Thomas and Marmar Charles R. 2005. “Why Are Hispanics at Greater Risk for Ptsd?”. Cultural Diversity and Ethnic Minority Psychology 11(2):144–61. [ DOI ] [ PubMed ] [ Google Scholar ]
- Priest Naomi, Paradies Yin, Trenerry Brigid, Truong Mandy, Karlsen Saffron and Kelly Yvonne 2013. “A Systematic Review of Studies Examining the Relationship between Reported Racism and Health and Wellbeing for Children and Young People.” Social Science & Medicine 95:115–27. [ DOI ] [ PubMed ] [ Google Scholar ]
- Priest Naomi, Slopen Natalie, Woolford Susan, Philip Jeny Tony, Singer Dianne, Kauffman Anna Daly, Moseley Kathryn, Davis Matthew, Ransome Yusuf and Williams David R. 2018. “Stereotyping across Intersections of Race and Age: Racial Stereotyping among White Adults Working with Children.” PLoS One 13(9):e0205614. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ren Xinhua S., Amick Benjamin C. and Williams David R. 1999. “Racial/Ethnic Disparities in Health: The Interplay between Discrimination and Socioeconomic Status.” Ethnicity & Disease 9(2):151–65. [ PubMed ] [ Google Scholar ]
- Sabin Janice A., Nosek Brian A., Greenwald Anthony G. and Rivara Frederick P. 2009. “Physicians’ Implicit and Explicit Attitudes About Race by Md Race, Ethnicity, and Gender.” Journal of Health Care for the Poor and Underserved 20(3):896–913. doi: 10.1353/hpu.0.0185. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sawyer Pamela J., Major Brenda, Casad Bettina J., Townsend Sarah SM and Mendes Wendy Berry 2012. “Discrimination and the Stress Response: Psychological and Physiological Consequences of Anticipating Prejudice in Interethnic Interactions.” American Journal of Public Health 102(5):1020–26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schulz Amy J., Gravlee Clarence C., Williams David R., Israel Barbara A., Mentz Graciela and Rowe Zachary 2006. “Discrimination, Symptoms of Depression, and Self-Rated Health among African American Women in Detroit: Results from a Longitudinal Analysis.” American Journal of Public Health 96(7):1265–70. doi: 10.2105/ajph.2005.064543. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Segal Steven R., Bola John R. and Watson Margaret A. 1996. “Race, Quality of Care, and Antipsychotic Prescribing Practices in Psychiatric Emergency Services.” Pscyhiatric Services 47(3):282–86. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smedley Brian D., Stith Adrienne Y. and Nelson Alan R. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press. [ PubMed ] [ Google Scholar ]
- Steele Claude M. 1997. “A Threat in the Air: How Stereotypes Shape Intellectual Identity and Performance.” American Psychologist 52(6):613–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sternthal Michelle J., Slopen Natalie and Williams David R. 2011. “Racial Disparities in Health: How Much Does Stress Really Matter?”. Du Bois Review: Social Science Research on Race 8(1):95–113. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Quiroga Szkupinski, Seline Medina, Dulce M and Glick Jennifer 2014. “In the Belly of the Beast: Effects of Anti-Immigration Policy on Latino Community Members.” American Behavioral Scientist 58(13):1723–42. [ Google Scholar ]
- Taylor J and Grundy C 1996. “Nadanolitization [Nad] Scale (1978).” Pp. 217–26 in Handbook of Tests and Measurements for Black Populations, Vol. 2, edited by Jones RL Hampton, VA: Cobb & Henry Publishers. [ Google Scholar ]
- Taylor Jerome and Jackson Beryl 1990. “Factors Affecting Alcohol Consumption in Black Women, Part Ii.” The International Journal of Addictions 25(12):1415–27. [ DOI ] [ PubMed ] [ Google Scholar ]
- Taylor Jerome, Henderson Delores and Jackson Beryl. B. 1991. “A Holistic Model for Understanding and Predicting Depression in African American Women.” Journal of Community Psychology 19:306–20. [ Google Scholar ]
- Taylor Jerome and Jackson Beryl B. 1991. “Evaluation of a Holistic Model of Mental Health Symptoms in African American Women.” Journal of Black Psychology 18:19–45. [ Google Scholar ]
- Thoits Peggy A. 2010. “Stress and Health Major Findings and Policy Implications.” Journal of Health and Social Behavior 51(1 suppl):S41–S53. doi: 10.1177/0022146510383499. [ DOI ] [ PubMed ] [ Google Scholar ]
- Toomey Russell B., Umaña-Taylor Adriana J., Williams David R., Harvey-Mendoza Elizabeth, Jahromi Laudan B. and Updegraff Kimberly A. 2014. “Impact of Arizona’s Sb 1070 Immigration Law on Utilization of Health Care and Public Assistance among Mexican-Origin Adolescent Mothers and Their Mother Figures.” American Journal of Public Health 104 Suppl 1:S28–34. doi: 10.2105/ajph.2013.301655. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jay. Turner, R. 2013. “Understanding Health Disparities: The Relevance of the Stress Process Model.” Society and Mental Health 3(3):170–86. [ Google Scholar ]
- Turney Kristin, Kissane Rebecca and Edin Kathryn 2013. “After Moving to Opportunity: How Moving to a Low-Poverty Neighborhood Improves Mental Health among African American Women.” Society and Mental Health 3(1):1–21. [ Google Scholar ]
- Umaña-Taylor Adriana J., Tynes Brendesha M., Toomey Russell B., Williams David R. and Mitchell Kimberly J. 2015. “Latino Adolescents’ Perceived Discrimination in Online and Offline Settings: An Examination of Cultural Risk and Protective Factors.” Developmental Psychology 51(1):87–100. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Umberson Debra 2017. “Black Deaths Matter: Race, Relationship Loss, and Effects on Survivors.” Journal of Health and Social Behavior 58(4):405–20. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- van Ryn Michelle, Burgess Diana J., Dovidio John F., Phelan Sean M., Saha Somnath, Malat Jennifer, Griffin Joan M., Fu Steven S. and Perry Sylvia 2011. “The Impact of Racism on Clinician Cognition, Behavior, and Clinical Decision Making.” Du Bois Review 8(1):199–218. doi: 10.1017/S1742058X11000191. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vega William A. and Rumbaut Ruben G. 1991. “Ethnic Minorities and Mental Health.” Annual Review of Sociology 17:351–83. [ Google Scholar ]
- Wallace Stephanie, Nazroo James and Bécares Laia 2016. “Cumulative Effect of Racial Discrimination on the Mental Health of Ethnic Minorities in the United Kingdom.” American Journal of Public Health 106(7):1294–300. doi: 10.2105/AJPH.2016.303121. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wildeman Christopher and Wang Emily A. 2017. “Mass Incarceration, Public Health, and Widening Inequality in the USA.” The Lancet 389(10077):1464–74. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wildeman Christopher, Goldman Alyssa W. and Turney Kristin 2018. “Parental Incarceration and Child Health in the United States.” Epidemiologic Reviews 40(1):146–56. [ DOI ] [ PubMed ] [ Google Scholar ]
- Williams David R., Lavizzo-Mourey Risa and Warren Rueben C. 1994. “The Concept of Race and Health Status in America.” Public Health Reports 109(1):26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams David R., Yu Yan, Jackson James S. and Anderson Norman B. 1997. “Racial Differences in Physical and Mental Health: Socioeconomic Status, Stress, and Discrimination.” Journal of Health Psychology 2(3):335–51. [ DOI ] [ PubMed ] [ Google Scholar ]
- Williams David R. and Collins Chiquita 2001. “Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health.” Public Health Reports 116(5):404–16. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams David R., Neighbors Harold W. and Jackson James S. 2003. “Racial/Ethnic Discrimination and Health: Findings from Community Studies.” American Journal of Public Health 93(2):200–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams David R., Gonzalez Hector M., Neighbors Harold, Nesse Randolph, Abelson Jamie, Sweetman Julie and Jackson James S. 2007. “Prevalence and Distribution of Major Depressive Disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: Results from the National Survey of American Life.” Archives of General Psychiatry 64(3):305–15. [ DOI ] [ PubMed ] [ Google Scholar ]
- Williams David R., Gonzalez Hector M., Williams Stacey, Mohammed Selina. A., Moomal Hashim and Stein Dan J. 2008. “Perceived Discrimination, Race and Health in South Africa.” Social Science & Medicine 67(3):441–52. doi: 10.1016/j.socscimed.2008.03.021. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams David R. and Mohammed Selina A. 2009. “Discrimination and Racial Disparities in Health: Evidence and Needed Research.” Journal of Behavioral Medicine 32(1):20–47. doi: 10.1007/s10865-008-9185-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams David R. and Mohammed Selina A. 2013. “Racism and Health I: Pathways and Scientific Evidence.” American Behavioral Scientist 57(8):1152–73. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (367.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
COMMENTS
This manuscript summarizes areas of school mental health (SMH) research relevant to the interplay between students' academic and social-emotional outcomes.
The scale. relates to the four typ es of the mental disorders among students, such a s tired or headaches, mood swings or insomnia. Previous. results showed that more the 38% studen ts are ...
Introduction. In 2022, there were roughly 19 million undergraduate students enrolled in U.S. postsecondary education National Center for Education Statistics, (Citation 2022).A mounting body of evidence reveals that college student mental health outcomes are worsening over time; in the 2020-2021 academic year, over 60% of students were experiencing at least one clinically-significant mental ...
pandemic, the percentage of students seeking mental health services at school had increased. • The Centers for Disease Control and Prevention (CDC) reported that emergency room visits due to suicide attempts among girls aged 12-17 were over 50 percent higher in the spring of 2021 compared to the same time in 2019.
Depression, anxiety and stress are currently the most common mental health problems among university students (Aldiabat et al., 2014). Hence this study aims to find out the prevalence of stress ...
Limitations of the study and futures lines in mental health research among adolescents are briefly discussed. ... the existing research offers insights into the role played by individual and contextual factors in secondary school students' mental health, ... An overview of vulnerabilities and risk factors background paper by who secretariat ...
Abstract. This review aims to focus on the effects of COVID-19 on university students' mental health and deepen our understanding of it. The conclusions are based on the review of 32 studies conducted during the pandemic. This review confirms that university students were at high risk for mental health disorders, heightened stress, and ...
The number of students seeking help at campus counseling centers increased almost 40% between 2009 and 2015 and continued to rise until the pandemic began, according to data from Penn State University's Center for Collegiate Mental Health (CCMH), a research-practice network of more than 700 college and university counseling centers (CCMH Annual Report, 2015).
College Students' Self-reported Mental Health Symptoms 9DULDEOHa Male (%))HPDOH +RSHOHVVQHVV )HHOLQJ RYHUZKHOPHG 9HU\ ORQHO\ 9HU\ VDG 'LIÀFXOW\ IXQFWLRQLQJ GXH WR GHSUHVVLRQ 2YHUZKHOPLQJ DQ[LHW\ &RQVLGHUHG VXLFLGH
significant student mental health challenges. School mental health addresses all aspects of social-emotional development of school-age children including wellness, mental illness, substance abuse, and effects of adverse childhood experiences" (2015, p.3). Similarly, for Cefai and Cooper (2017), mental health promotion in
One meta-analysis of psychosocial risk factors for mental health problems among secondary school students in China found that higher levels of academic pressure ... Mental Health Test (Zhou, 1991) Students who reported very high levels of academic pressure were more likely to have moderate (OR = 6.52, 95 % CI: 2.67-16.0) and severe anxiety (OR ...
Research paper. Trends in college student mental health and help-seeking by race/ethnicity: Findings from the national healthy minds study, 2013-2021 ... For each of the seven prevalence outcomes, annual trends reveal worsening mental health among all students. (1) For flourishing, there was a 32.5% decrease among all students from 2013 to ...
Students are struggling with mental health difficulties that impact their ability to learn while in school, and many students lack access to mental health providers in their communities. ... School administrators are in a prime position to lead systemic change aimed at supporting student mental health. The purpose of this paper is to provide ...
Background Worsening mental health of students in higher education is a public policy concern and the impact of measures to reduce transmission of COVID-19 has heightened awareness of this issue. Preventing poor mental health and supporting positive mental wellbeing needs to be based on an evidence informed understanding what factors influence the mental health of students. Objectives To ...
Methods. A single author (MP) searched PubMed and Google Scholar for peer-reviewed articles published at any time in English. Search terms included academic, school, university, stress, mental health, depression, anxiety, youth, young people, resilience, stress management, stress education, substance use, sleep, drop-out, physical health with a combination of any and/or all of the preceding terms.
This research paper explores the intricate relationship between students' mental health and their academic success in college. In light of the rising reports of mental health concerns among ...
Use of the assessment tool is recommended for students to distinguish between those at decreased and increased risk in terms of mental health. Mental health services should be offered to students at higher risk. Keywords: assessment tool, mental health, likelihood ratio, predictive ability, students. 1. Introduction.
Background: Student mental health in higher education has been an increasing concern. The COVID-19 pandemic situation has brought this vulnerable population into renewed focus. Objective: Our study aims to conduct a timely assessment of the effects of the COVID-19 pandemic on the mental health of college students. Methods: We conducted interview surveys with 195 students at a large public ...
Depression and anxiety are among the most prevalent mental health concerns among youth (Institute for Health Metrics and Evaluation [IHME], 2018) and have been frequently linked to academic performance in adolescents.Among 98 secondary students age 12 to 16 in Spain, cross-sectional depression scores were inversely correlated with lower grades in nearly every subject area assessed, as well as ...
What factors are associated with the development and detection of poor student mental health? McIntyre et al. (Citation 2018) carefully examined both academic and non-academic predictors of distress among 1135 UK undergraduates and found different factors associated with different outcomes.Loneliness was the strongest overall predictor of distress, academic stress was the strongest for ...
Social Media and Youth Mental Health: The U.S. Surgeon General's Advisory 19 • Establish the impact of social media on youth mental health as a research priority and develop a shared research agenda. Research should include but not be limited to: 102 » Rigorous evaluation of social media's impact on youth mental health and well-being,
The Ministry for Education, Sports, Youth, Research and Innovation (MEYR) in Malta, through the People Management Department and in collaboration with the Commissioner for Mental Health and Richmond Foundation, embarked on a 3-year-long project aimed at increasing mental health literacy (MHL) among secondary school educators and students.
In order to provide extensive guidance, infrastructure, and support in pursuit of its research mission, research@BSPH employs three core areas: strategy and development, implementation and impact, and integrity and oversight. Our exceptional research teams comprised of faculty, postdoctoral fellows, students, and committed staff are united in our collaborative, collegial, and entrepreneurial ...
This research is broadly consistent with a larger paradox in the research literature between mental and physical health risks among African Americans. African Americans tend to have worse health than whites on virtually every indicator of physical health, but, as noted earlier, despite higher levels of stress, they have lower rates of stress ...