REVIEW article
Environmental and health impacts of air pollution: a review.

- 1 Delphis S.A., Kifisia, Greece
- 2 Laboratory of Hygiene and Environmental Protection, Faculty of Medicine, Democritus University of Thrace, Alexandroupolis, Greece
- 3 Centre Hospitalier Universitaire Vaudois (CHUV), Service de Médicine Interne, Lausanne, Switzerland
- 4 School of Social and Political Sciences, University of Glasgow, Glasgow, United Kingdom
One of our era's greatest scourges is air pollution, on account not only of its impact on climate change but also its impact on public and individual health due to increasing morbidity and mortality. There are many pollutants that are major factors in disease in humans. Among them, Particulate Matter (PM), particles of variable but very small diameter, penetrate the respiratory system via inhalation, causing respiratory and cardiovascular diseases, reproductive and central nervous system dysfunctions, and cancer. Despite the fact that ozone in the stratosphere plays a protective role against ultraviolet irradiation, it is harmful when in high concentration at ground level, also affecting the respiratory and cardiovascular system. Furthermore, nitrogen oxide, sulfur dioxide, Volatile Organic Compounds (VOCs), dioxins, and polycyclic aromatic hydrocarbons (PAHs) are all considered air pollutants that are harmful to humans. Carbon monoxide can even provoke direct poisoning when breathed in at high levels. Heavy metals such as lead, when absorbed into the human body, can lead to direct poisoning or chronic intoxication, depending on exposure. Diseases occurring from the aforementioned substances include principally respiratory problems such as Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, and also lung cancer, cardiovascular events, central nervous system dysfunctions, and cutaneous diseases. Last but not least, climate change resulting from environmental pollution affects the geographical distribution of many infectious diseases, as do natural disasters. The only way to tackle this problem is through public awareness coupled with a multidisciplinary approach by scientific experts; national and international organizations must address the emergence of this threat and propose sustainable solutions.

Approach to the Problem
The interactions between humans and their physical surroundings have been extensively studied, as multiple human activities influence the environment. The environment is a coupling of the biotic (living organisms and microorganisms) and the abiotic (hydrosphere, lithosphere, and atmosphere).
Pollution is defined as the introduction into the environment of substances harmful to humans and other living organisms. Pollutants are harmful solids, liquids, or gases produced in higher than usual concentrations that reduce the quality of our environment.
Human activities have an adverse effect on the environment by polluting the water we drink, the air we breathe, and the soil in which plants grow. Although the industrial revolution was a great success in terms of technology, society, and the provision of multiple services, it also introduced the production of huge quantities of pollutants emitted into the air that are harmful to human health. Without any doubt, the global environmental pollution is considered an international public health issue with multiple facets. Social, economic, and legislative concerns and lifestyle habits are related to this major problem. Clearly, urbanization and industrialization are reaching unprecedented and upsetting proportions worldwide in our era. Anthropogenic air pollution is one of the biggest public health hazards worldwide, given that it accounts for about 9 million deaths per year ( 1 ).
Without a doubt, all of the aforementioned are closely associated with climate change, and in the event of danger, the consequences can be severe for mankind ( 2 ). Climate changes and the effects of global planetary warming seriously affect multiple ecosystems, causing problems such as food safety issues, ice and iceberg melting, animal extinction, and damage to plants ( 3 , 4 ).
Air pollution has various health effects. The health of susceptible and sensitive individuals can be impacted even on low air pollution days. Short-term exposure to air pollutants is closely related to COPD (Chronic Obstructive Pulmonary Disease), cough, shortness of breath, wheezing, asthma, respiratory disease, and high rates of hospitalization (a measurement of morbidity).
The long-term effects associated with air pollution are chronic asthma, pulmonary insufficiency, cardiovascular diseases, and cardiovascular mortality. According to a Swedish cohort study, diabetes seems to be induced after long-term air pollution exposure ( 5 ). Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ).
National reports have mentioned the increased risk of morbidity and mortality ( 1 ). These studies were conducted in many places around the world and show a correlation between daily ranges of particulate matter (PM) concentration and daily mortality. Climate shifts and global planetary warming ( 3 ) could aggravate the situation. Besides, increased hospitalization (an index of morbidity) has been registered among the elderly and susceptible individuals for specific reasons. Fine and ultrafine particulate matter seems to be associated with more serious illnesses ( 6 ), as it can invade the deepest parts of the airways and more easily reach the bloodstream.
Air pollution mainly affects those living in large urban areas, where road emissions contribute the most to the degradation of air quality. There is also a danger of industrial accidents, where the spread of a toxic fog can be fatal to the populations of the surrounding areas. The dispersion of pollutants is determined by many parameters, most notably atmospheric stability and wind ( 6 ).
In developing countries ( 7 ), the problem is more serious due to overpopulation and uncontrolled urbanization along with the development of industrialization. This leads to poor air quality, especially in countries with social disparities and a lack of information on sustainable management of the environment. The use of fuels such as wood fuel or solid fuel for domestic needs due to low incomes exposes people to bad-quality, polluted air at home. It is of note that three billion people around the world are using the above sources of energy for their daily heating and cooking needs ( 8 ). In developing countries, the women of the household seem to carry the highest risk for disease development due to their longer duration exposure to the indoor air pollution ( 8 , 9 ). Due to its fast industrial development and overpopulation, China is one of the Asian countries confronting serious air pollution problems ( 10 , 11 ). The lung cancer mortality observed in China is associated with fine particles ( 12 ). As stated already, long-term exposure is associated with deleterious effects on the cardiovascular system ( 3 , 5 ). However, it is interesting to note that cardiovascular diseases have mostly been observed in developed and high-income countries rather than in the developing low-income countries exposed highly to air pollution ( 13 ). Extreme air pollution is recorded in India, where the air quality reaches hazardous levels. New Delhi is one of the more polluted cities in India. Flights in and out of New Delhi International Airport are often canceled due to the reduced visibility associated with air pollution. Pollution is occurring both in urban and rural areas in India due to the fast industrialization, urbanization, and rise in use of motorcycle transportation. Nevertheless, biomass combustion associated with heating and cooking needs and practices is a major source of household air pollution in India and in Nepal ( 14 , 15 ). There is spatial heterogeneity in India, as areas with diverse climatological conditions and population and education levels generate different indoor air qualities, with higher PM 2.5 observed in North Indian states (557–601 μg/m 3 ) compared to the Southern States (183–214 μg/m 3 ) ( 16 , 17 ). The cold climate of the North Indian areas may be the main reason for this, as longer periods at home and more heating are necessary compared to in the tropical climate of Southern India. Household air pollution in India is associated with major health effects, especially in women and young children, who stay indoors for longer periods. Chronic obstructive respiratory disease (CORD) and lung cancer are mostly observed in women, while acute lower respiratory disease is seen in young children under 5 years of age ( 18 ).
Accumulation of air pollution, especially sulfur dioxide and smoke, reaching 1,500 mg/m3, resulted in an increase in the number of deaths (4,000 deaths) in December 1952 in London and in 1963 in New York City (400 deaths) ( 19 ). An association of pollution with mortality was reported on the basis of monitoring of outdoor pollution in six US metropolitan cities ( 20 ). In every case, it seems that mortality was closely related to the levels of fine, inhalable, and sulfate particles more than with the levels of total particulate pollution, aerosol acidity, sulfur dioxide, or nitrogen dioxide ( 20 ).
Furthermore, extremely high levels of pollution are reported in Mexico City and Rio de Janeiro, followed by Milan, Ankara, Melbourne, Tokyo, and Moscow ( 19 ).
Based on the magnitude of the public health impact, it is certain that different kinds of interventions should be taken into account. Success and effectiveness in controlling air pollution, specifically at the local level, have been reported. Adequate technological means are applied considering the source and the nature of the emission as well as its impact on health and the environment. The importance of point sources and non-point sources of air pollution control is reported by Schwela and Köth-Jahr ( 21 ). Without a doubt, a detailed emission inventory must record all sources in a given area. Beyond considering the above sources and their nature, topography and meteorology should also be considered, as stated previously. Assessment of the control policies and methods is often extrapolated from the local to the regional and then to the global scale. Air pollution may be dispersed and transported from one region to another area located far away. Air pollution management means the reduction to acceptable levels or possible elimination of air pollutants whose presence in the air affects our health or the environmental ecosystem. Private and governmental entities and authorities implement actions to ensure the air quality ( 22 ). Air quality standards and guidelines were adopted for the different pollutants by the WHO and EPA as a tool for the management of air quality ( 1 , 23 ). These standards have to be compared to the emissions inventory standards by causal analysis and dispersion modeling in order to reveal the problematic areas ( 24 ). Inventories are generally based on a combination of direct measurements and emissions modeling ( 24 ).
As an example, we state here the control measures at the source through the use of catalytic converters in cars. These are devices that turn the pollutants and toxic gases produced from combustion engines into less-toxic pollutants by catalysis through redox reactions ( 25 ). In Greece, the use of private cars was restricted by tracking their license plates in order to reduce traffic congestion during rush hour ( 25 ).
Concerning industrial emissions, collectors and closed systems can keep the air pollution to the minimal standards imposed by legislation ( 26 ).
Current strategies to improve air quality require an estimation of the economic value of the benefits gained from proposed programs. These proposed programs by public authorities, and directives are issued with guidelines to be respected.
In Europe, air quality limit values AQLVs (Air Quality Limit Values) are issued for setting off planning claims ( 27 ). In the USA, the NAAQS (National Ambient Air Quality Standards) establish the national air quality limit values ( 27 ). While both standards and directives are based on different mechanisms, significant success has been achieved in the reduction of overall emissions and associated health and environmental effects ( 27 ). The European Directive identifies geographical areas of risk exposure as monitoring/assessment zones to record the emission sources and levels of air pollution ( 27 ), whereas the USA establishes global geographical air quality criteria according to the severity of their air quality problem and records all sources of the pollutants and their precursors ( 27 ).
In this vein, funds have been financing, directly or indirectly, projects related to air quality along with the technical infrastructure to maintain good air quality. These plans focus on an inventory of databases from air quality environmental planning awareness campaigns. Moreover, pollution measures of air emissions may be taken for vehicles, machines, and industries in urban areas.
Technological innovation can only be successful if it is able to meet the needs of society. In this sense, technology must reflect the decision-making practices and procedures of those involved in risk assessment and evaluation and act as a facilitator in providing information and assessments to enable decision makers to make the best decisions possible. Summarizing the aforementioned in order to design an effective air quality control strategy, several aspects must be considered: environmental factors and ambient air quality conditions, engineering factors and air pollutant characteristics, and finally, economic operating costs for technological improvement and administrative and legal costs. Considering the economic factor, competitiveness through neoliberal concepts is offering a solution to environmental problems ( 22 ).
The development of environmental governance, along with technological progress, has initiated the deployment of a dialogue. Environmental politics has created objections and points of opposition between different political parties, scientists, media, and governmental and non-governmental organizations ( 22 ). Radical environmental activism actions and movements have been created ( 22 ). The rise of the new information and communication technologies (ICTs) are many times examined as to whether and in which way they have influenced means of communication and social movements such as activism ( 28 ). Since the 1990s, the term “digital activism” has been used increasingly and in many different disciplines ( 29 ). Nowadays, multiple digital technologies can be used to produce a digital activism outcome on environmental issues. More specifically, devices with online capabilities such as computers or mobile phones are being used as a way to pursue change in political and social affairs ( 30 ).
In the present paper, we focus on the sources of environmental pollution in relation to public health and propose some solutions and interventions that may be of interest to environmental legislators and decision makers.
Sources of Exposure
It is known that the majority of environmental pollutants are emitted through large-scale human activities such as the use of industrial machinery, power-producing stations, combustion engines, and cars. Because these activities are performed at such a large scale, they are by far the major contributors to air pollution, with cars estimated to be responsible for approximately 80% of today's pollution ( 31 ). Some other human activities are also influencing our environment to a lesser extent, such as field cultivation techniques, gas stations, fuel tanks heaters, and cleaning procedures ( 32 ), as well as several natural sources, such as volcanic and soil eruptions and forest fires.
The classification of air pollutants is based mainly on the sources producing pollution. Therefore, it is worth mentioning the four main sources, following the classification system: Major sources, Area sources, Mobile sources, and Natural sources.
Major sources include the emission of pollutants from power stations, refineries, and petrochemicals, the chemical and fertilizer industries, metallurgical and other industrial plants, and, finally, municipal incineration.
Indoor area sources include domestic cleaning activities, dry cleaners, printing shops, and petrol stations.
Mobile sources include automobiles, cars, railways, airways, and other types of vehicles.
Finally, natural sources include, as stated previously, physical disasters ( 33 ) such as forest fire, volcanic erosion, dust storms, and agricultural burning.
However, many classification systems have been proposed. Another type of classification is a grouping according to the recipient of the pollution, as follows:
Air pollution is determined as the presence of pollutants in the air in large quantities for long periods. Air pollutants are dispersed particles, hydrocarbons, CO, CO 2 , NO, NO 2 , SO 3 , etc.
Water pollution is organic and inorganic charge and biological charge ( 10 ) at high levels that affect the water quality ( 34 , 35 ).
Soil pollution occurs through the release of chemicals or the disposal of wastes, such as heavy metals, hydrocarbons, and pesticides.
Air pollution can influence the quality of soil and water bodies by polluting precipitation, falling into water and soil environments ( 34 , 36 ). Notably, the chemistry of the soil can be amended due to acid precipitation by affecting plants, cultures, and water quality ( 37 ). Moreover, movement of heavy metals is favored by soil acidity, and metals are so then moving into the watery environment. It is known that heavy metals such as aluminum are noxious to wildlife and fishes. Soil quality seems to be of importance, as soils with low calcium carbonate levels are at increased jeopardy from acid rain. Over and above rain, snow and particulate matter drip into watery ' bodies ( 36 , 38 ).
Lastly, pollution is classified following type of origin:
Radioactive and nuclear pollution , releasing radioactive and nuclear pollutants into water, air, and soil during nuclear explosions and accidents, from nuclear weapons, and through handling or disposal of radioactive sewage.
Radioactive materials can contaminate surface water bodies and, being noxious to the environment, plants, animals, and humans. It is known that several radioactive substances such as radium and uranium concentrate in the bones and can cause cancers ( 38 , 39 ).
Noise pollution is produced by machines, vehicles, traffic noises, and musical installations that are harmful to our hearing.
The World Health Organization introduced the term DALYs. The DALYs for a disease or health condition is defined as the sum of the Years of Life Lost (YLL) due to premature mortality in the population and the Years Lost due to Disability (YLD) for people living with the health condition or its consequences ( 39 ). In Europe, air pollution is the main cause of disability-adjusted life years lost (DALYs), followed by noise pollution. The potential relationships of noise and air pollution with health have been studied ( 40 ). The study found that DALYs related to noise were more important than those related to air pollution, as the effects of environmental noise on cardiovascular disease were independent of air pollution ( 40 ). Environmental noise should be counted as an independent public health risk ( 40 ).
Environmental pollution occurs when changes in the physical, chemical, or biological constituents of the environment (air masses, temperature, climate, etc.) are produced.
Pollutants harm our environment either by increasing levels above normal or by introducing harmful toxic substances. Primary pollutants are directly produced from the above sources, and secondary pollutants are emitted as by-products of the primary ones. Pollutants can be biodegradable or non-biodegradable and of natural origin or anthropogenic, as stated previously. Moreover, their origin can be a unique source (point-source) or dispersed sources.
Pollutants have differences in physical and chemical properties, explaining the discrepancy in their capacity for producing toxic effects. As an example, we state here that aerosol compounds ( 41 – 43 ) have a greater toxicity than gaseous compounds due to their tiny size (solid or liquid) in the atmosphere; they have a greater penetration capacity. Gaseous compounds are eliminated more easily by our respiratory system ( 41 ). These particles are able to damage lungs and can even enter the bloodstream ( 41 ), leading to the premature deaths of millions of people yearly. Moreover, the aerosol acidity ([H+]) seems to considerably enhance the production of secondary organic aerosols (SOA), but this last aspect is not supported by other scientific teams ( 38 ).
Climate and Pollution
Air pollution and climate change are closely related. Climate is the other side of the same coin that reduces the quality of our Earth ( 44 ). Pollutants such as black carbon, methane, tropospheric ozone, and aerosols affect the amount of incoming sunlight. As a result, the temperature of the Earth is increasing, resulting in the melting of ice, icebergs, and glaciers.
In this vein, climatic changes will affect the incidence and prevalence of both residual and imported infections in Europe. Climate and weather affect the duration, timing, and intensity of outbreaks strongly and change the map of infectious diseases in the globe ( 45 ). Mosquito-transmitted parasitic or viral diseases are extremely climate-sensitive, as warming firstly shortens the pathogen incubation period and secondly shifts the geographic map of the vector. Similarly, water-warming following climate changes leads to a high incidence of waterborne infections. Recently, in Europe, eradicated diseases seem to be emerging due to the migration of population, for example, cholera, poliomyelitis, tick-borne encephalitis, and malaria ( 46 ).
The spread of epidemics is associated with natural climate disasters and storms, which seem to occur more frequently nowadays ( 47 ). Malnutrition and disequilibration of the immune system are also associated with the emerging infections affecting public health ( 48 ).
The Chikungunya virus “took the airplane” from the Indian Ocean to Europe, as outbreaks of the disease were registered in Italy ( 49 ) as well as autochthonous cases in France ( 50 ).
An increase in cryptosporidiosis in the United Kingdom and in the Czech Republic seems to have occurred following flooding ( 36 , 51 ).
As stated previously, aerosols compounds are tiny in size and considerably affect the climate. They are able to dissipate sunlight (the albedo phenomenon) by dispersing a quarter of the sun's rays back to space and have cooled the global temperature over the last 30 years ( 52 ).
Air Pollutants
The World Health Organization (WHO) reports on six major air pollutants, namely particle pollution, ground-level ozone, carbon monoxide, sulfur oxides, nitrogen oxides, and lead. Air pollution can have a disastrous effect on all components of the environment, including groundwater, soil, and air. Additionally, it poses a serious threat to living organisms. In this vein, our interest is mainly to focus on these pollutants, as they are related to more extensive and severe problems in human health and environmental impact. Acid rain, global warming, the greenhouse effect, and climate changes have an important ecological impact on air pollution ( 53 ).
Particulate Matter (PM) and Health
Studies have shown a relationship between particulate matter (PM) and adverse health effects, focusing on either short-term (acute) or long-term (chronic) PM exposure.
Particulate matter (PM) is usually formed in the atmosphere as a result of chemical reactions between the different pollutants. The penetration of particles is closely dependent on their size ( 53 ). Particulate Matter (PM) was defined as a term for particles by the United States Environmental Protection Agency ( 54 ). Particulate matter (PM) pollution includes particles with diameters of 10 micrometers (μm) or smaller, called PM 10 , and extremely fine particles with diameters that are generally 2.5 micrometers (μm) and smaller.
Particulate matter contains tiny liquid or solid droplets that can be inhaled and cause serious health effects ( 55 ). Particles <10 μm in diameter (PM 10 ) after inhalation can invade the lungs and even reach the bloodstream. Fine particles, PM 2.5 , pose a greater risk to health ( 6 , 56 ) ( Table 1 ).
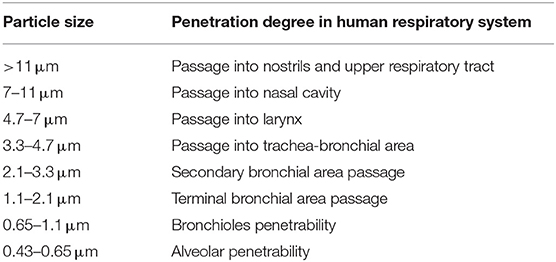
Table 1 . Penetrability according to particle size.
Multiple epidemiological studies have been performed on the health effects of PM. A positive relation was shown between both short-term and long-term exposures of PM 2.5 and acute nasopharyngitis ( 56 ). In addition, long-term exposure to PM for years was found to be related to cardiovascular diseases and infant mortality.
Those studies depend on PM 2.5 monitors and are restricted in terms of study area or city area due to a lack of spatially resolved daily PM 2.5 concentration data and, in this way, are not representative of the entire population. Following a recent epidemiological study by the Department of Environmental Health at Harvard School of Public Health (Boston, MA) ( 57 ), it was reported that, as PM 2.5 concentrations vary spatially, an exposure error (Berkson error) seems to be produced, and the relative magnitudes of the short- and long-term effects are not yet completely elucidated. The team developed a PM 2.5 exposure model based on remote sensing data for assessing short- and long-term human exposures ( 57 ). This model permits spatial resolution in short-term effects plus the assessment of long-term effects in the whole population.
Moreover, respiratory diseases and affection of the immune system are registered as long-term chronic effects ( 58 ). It is worth noting that people with asthma, pneumonia, diabetes, and respiratory and cardiovascular diseases are especially susceptible and vulnerable to the effects of PM. PM 2.5 , followed by PM 10 , are strongly associated with diverse respiratory system diseases ( 59 ), as their size permits them to pierce interior spaces ( 60 ). The particles produce toxic effects according to their chemical and physical properties. The components of PM 10 and PM 2.5 can be organic (polycyclic aromatic hydrocarbons, dioxins, benzene, 1-3 butadiene) or inorganic (carbon, chlorides, nitrates, sulfates, metals) in nature ( 55 ).
Particulate Matter (PM) is divided into four main categories according to type and size ( 61 ) ( Table 2 ).
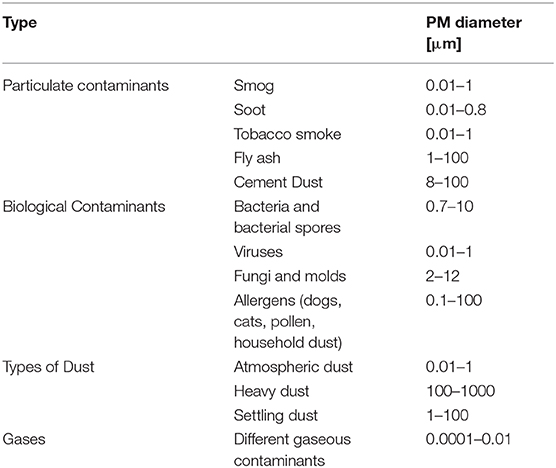
Table 2 . Types and sizes of particulate Matter (PM).
Gas contaminants include PM in aerial masses.
Particulate contaminants include contaminants such as smog, soot, tobacco smoke, oil smoke, fly ash, and cement dust.
Biological Contaminants are microorganisms (bacteria, viruses, fungi, mold, and bacterial spores), cat allergens, house dust and allergens, and pollen.
Types of Dust include suspended atmospheric dust, settling dust, and heavy dust.
Finally, another fact is that the half-lives of PM 10 and PM 2.5 particles in the atmosphere is extended due to their tiny dimensions; this permits their long-lasting suspension in the atmosphere and even their transfer and spread to distant destinations where people and the environment may be exposed to the same magnitude of pollution ( 53 ). They are able to change the nutrient balance in watery ecosystems, damage forests and crops, and acidify water bodies.
As stated, PM 2.5 , due to their tiny size, are causing more serious health effects. These aforementioned fine particles are the main cause of the “haze” formation in different metropolitan areas ( 12 , 13 , 61 ).
Ozone Impact in the Atmosphere
Ozone (O 3 ) is a gas formed from oxygen under high voltage electric discharge ( 62 ). It is a strong oxidant, 52% stronger than chlorine. It arises in the stratosphere, but it could also arise following chain reactions of photochemical smog in the troposphere ( 63 ).
Ozone can travel to distant areas from its initial source, moving with air masses ( 64 ). It is surprising that ozone levels over cities are low in contrast to the increased amounts occuring in urban areas, which could become harmful for cultures, forests, and vegetation ( 65 ) as it is reducing carbon assimilation ( 66 ). Ozone reduces growth and yield ( 47 , 48 ) and affects the plant microflora due to its antimicrobial capacity ( 67 , 68 ). In this regard, ozone acts upon other natural ecosystems, with microflora ( 69 , 70 ) and animal species changing their species composition ( 71 ). Ozone increases DNA damage in epidermal keratinocytes and leads to impaired cellular function ( 72 ).
Ground-level ozone (GLO) is generated through a chemical reaction between oxides of nitrogen and VOCs emitted from natural sources and/or following anthropogenic activities.
Ozone uptake usually occurs by inhalation. Ozone affects the upper layers of the skin and the tear ducts ( 73 ). A study of short-term exposure of mice to high levels of ozone showed malondialdehyde formation in the upper skin (epidermis) but also depletion in vitamins C and E. It is likely that ozone levels are not interfering with the skin barrier function and integrity to predispose to skin disease ( 74 ).
Due to the low water-solubility of ozone, inhaled ozone has the capacity to penetrate deeply into the lungs ( 75 ).
Toxic effects induced by ozone are registered in urban areas all over the world, causing biochemical, morphologic, functional, and immunological disorders ( 76 ).
The European project (APHEA2) focuses on the acute effects of ambient ozone concentrations on mortality ( 77 ). Daily ozone concentrations compared to the daily number of deaths were reported from different European cities for a 3-year period. During the warm period of the year, an observed increase in ozone concentration was associated with an increase in the daily number of deaths (0.33%), in the number of respiratory deaths (1.13%), and in the number of cardiovascular deaths (0.45%). No effect was observed during wintertime.
Carbon Monoxide (CO)
Carbon monoxide is produced by fossil fuel when combustion is incomplete. The symptoms of poisoning due to inhaling carbon monoxide include headache, dizziness, weakness, nausea, vomiting, and, finally, loss of consciousness.
The affinity of carbon monoxide to hemoglobin is much greater than that of oxygen. In this vein, serious poisoning may occur in people exposed to high levels of carbon monoxide for a long period of time. Due to the loss of oxygen as a result of the competitive binding of carbon monoxide, hypoxia, ischemia, and cardiovascular disease are observed.
Carbon monoxide affects the greenhouses gases that are tightly connected to global warming and climate. This should lead to an increase in soil and water temperatures, and extreme weather conditions or storms may occur ( 68 ).
However, in laboratory and field experiments, it has been seen to produce increased plant growth ( 78 ).
Nitrogen Oxide (NO 2 )
Nitrogen oxide is a traffic-related pollutant, as it is emitted from automobile motor engines ( 79 , 80 ). It is an irritant of the respiratory system as it penetrates deep in the lung, inducing respiratory diseases, coughing, wheezing, dyspnea, bronchospasm, and even pulmonary edema when inhaled at high levels. It seems that concentrations over 0.2 ppm produce these adverse effects in humans, while concentrations higher than 2.0 ppm affect T-lymphocytes, particularly the CD8+ cells and NK cells that produce our immune response ( 81 ).It is reported that long-term exposure to high levels of nitrogen dioxide can be responsible for chronic lung disease. Long-term exposure to NO 2 can impair the sense of smell ( 81 ).
However, systems other than respiratory ones can be involved, as symptoms such as eye, throat, and nose irritation have been registered ( 81 ).
High levels of nitrogen dioxide are deleterious to crops and vegetation, as they have been observed to reduce crop yield and plant growth efficiency. Moreover, NO 2 can reduce visibility and discolor fabrics ( 81 ).
Sulfur Dioxide (SO 2 )
Sulfur dioxide is a harmful gas that is emitted mainly from fossil fuel consumption or industrial activities. The annual standard for SO 2 is 0.03 ppm ( 82 ). It affects human, animal, and plant life. Susceptible people as those with lung disease, old people, and children, who present a higher risk of damage. The major health problems associated with sulfur dioxide emissions in industrialized areas are respiratory irritation, bronchitis, mucus production, and bronchospasm, as it is a sensory irritant and penetrates deep into the lung converted into bisulfite and interacting with sensory receptors, causing bronchoconstriction. Moreover, skin redness, damage to the eyes (lacrimation and corneal opacity) and mucous membranes, and worsening of pre-existing cardiovascular disease have been observed ( 81 ).
Environmental adverse effects, such as acidification of soil and acid rain, seem to be associated with sulfur dioxide emissions ( 83 ).
Lead is a heavy metal used in different industrial plants and emitted from some petrol motor engines, batteries, radiators, waste incinerators, and waste waters ( 84 ).
Moreover, major sources of lead pollution in the air are metals, ore, and piston-engine aircraft. Lead poisoning is a threat to public health due to its deleterious effects upon humans, animals, and the environment, especially in the developing countries.
Exposure to lead can occur through inhalation, ingestion, and dermal absorption. Trans- placental transport of lead was also reported, as lead passes through the placenta unencumbered ( 85 ). The younger the fetus is, the more harmful the toxic effects. Lead toxicity affects the fetal nervous system; edema or swelling of the brain is observed ( 86 ). Lead, when inhaled, accumulates in the blood, soft tissue, liver, lung, bones, and cardiovascular, nervous, and reproductive systems. Moreover, loss of concentration and memory, as well as muscle and joint pain, were observed in adults ( 85 , 86 ).
Children and newborns ( 87 ) are extremely susceptible even to minimal doses of lead, as it is a neurotoxicant and causes learning disabilities, impairment of memory, hyperactivity, and even mental retardation.
Elevated amounts of lead in the environment are harmful to plants and crop growth. Neurological effects are observed in vertebrates and animals in association with high lead levels ( 88 ).
Polycyclic Aromatic Hydrocarbons(PAHs)
The distribution of PAHs is ubiquitous in the environment, as the atmosphere is the most important means of their dispersal. They are found in coal and in tar sediments. Moreover, they are generated through incomplete combustion of organic matter as in the cases of forest fires, incineration, and engines ( 89 ). PAH compounds, such as benzopyrene, acenaphthylene, anthracene, and fluoranthene are recognized as toxic, mutagenic, and carcinogenic substances. They are an important risk factor for lung cancer ( 89 ).
Volatile Organic Compounds(VOCs)
Volatile organic compounds (VOCs), such as toluene, benzene, ethylbenzene, and xylene ( 90 ), have been found to be associated with cancer in humans ( 91 ). The use of new products and materials has actually resulted in increased concentrations of VOCs. VOCs pollute indoor air ( 90 ) and may have adverse effects on human health ( 91 ). Short-term and long-term adverse effects on human health are observed. VOCs are responsible for indoor air smells. Short-term exposure is found to cause irritation of eyes, nose, throat, and mucosal membranes, while those of long duration exposure include toxic reactions ( 92 ). Predictable assessment of the toxic effects of complex VOC mixtures is difficult to estimate, as these pollutants can have synergic, antagonistic, or indifferent effects ( 91 , 93 ).
Dioxins originate from industrial processes but also come from natural processes, such as forest fires and volcanic eruptions. They accumulate in foods such as meat and dairy products, fish and shellfish, and especially in the fatty tissue of animals ( 94 ).
Short-period exhibition to high dioxin concentrations may result in dark spots and lesions on the skin ( 94 ). Long-term exposure to dioxins can cause developmental problems, impairment of the immune, endocrine and nervous systems, reproductive infertility, and cancer ( 94 ).
Without any doubt, fossil fuel consumption is responsible for a sizeable part of air contamination. This contamination may be anthropogenic, as in agricultural and industrial processes or transportation, while contamination from natural sources is also possible. Interestingly, it is of note that the air quality standards established through the European Air Quality Directive are somewhat looser than the WHO guidelines, which are stricter ( 95 ).
Effect of Air Pollution on Health
The most common air pollutants are ground-level ozone and Particulates Matter (PM). Air pollution is distinguished into two main types:
Outdoor pollution is the ambient air pollution.
Indoor pollution is the pollution generated by household combustion of fuels.
People exposed to high concentrations of air pollutants experience disease symptoms and states of greater and lesser seriousness. These effects are grouped into short- and long-term effects affecting health.
Susceptible populations that need to be aware of health protection measures include old people, children, and people with diabetes and predisposing heart or lung disease, especially asthma.
As extensively stated previously, according to a recent epidemiological study from Harvard School of Public Health, the relative magnitudes of the short- and long-term effects have not been completely clarified ( 57 ) due to the different epidemiological methodologies and to the exposure errors. New models are proposed for assessing short- and long-term human exposure data more successfully ( 57 ). Thus, in the present section, we report the more common short- and long-term health effects but also general concerns for both types of effects, as these effects are often dependent on environmental conditions, dose, and individual susceptibility.
Short-term effects are temporary and range from simple discomfort, such as irritation of the eyes, nose, skin, throat, wheezing, coughing and chest tightness, and breathing difficulties, to more serious states, such as asthma, pneumonia, bronchitis, and lung and heart problems. Short-term exposure to air pollution can also cause headaches, nausea, and dizziness.
These problems can be aggravated by extended long-term exposure to the pollutants, which is harmful to the neurological, reproductive, and respiratory systems and causes cancer and even, rarely, deaths.
The long-term effects are chronic, lasting for years or the whole life and can even lead to death. Furthermore, the toxicity of several air pollutants may also induce a variety of cancers in the long term ( 96 ).
As stated already, respiratory disorders are closely associated with the inhalation of air pollutants. These pollutants will invade through the airways and will accumulate at the cells. Damage to target cells should be related to the pollutant component involved and its source and dose. Health effects are also closely dependent on country, area, season, and time. An extended exposure duration to the pollutant should incline to long-term health effects in relation also to the above factors.
Particulate Matter (PMs), dust, benzene, and O 3 cause serious damage to the respiratory system ( 97 ). Moreover, there is a supplementary risk in case of existing respiratory disease such as asthma ( 98 ). Long-term effects are more frequent in people with a predisposing disease state. When the trachea is contaminated by pollutants, voice alterations may be remarked after acute exposure. Chronic obstructive pulmonary disease (COPD) may be induced following air pollution, increasing morbidity and mortality ( 99 ). Long-term effects from traffic, industrial air pollution, and combustion of fuels are the major factors for COPD risk ( 99 ).
Multiple cardiovascular effects have been observed after exposure to air pollutants ( 100 ). Changes occurred in blood cells after long-term exposure may affect cardiac functionality. Coronary arteriosclerosis was reported following long-term exposure to traffic emissions ( 101 ), while short-term exposure is related to hypertension, stroke, myocardial infracts, and heart insufficiency. Ventricle hypertrophy is reported to occur in humans after long-time exposure to nitrogen oxide (NO 2 ) ( 102 , 103 ).
Neurological effects have been observed in adults and children after extended-term exposure to air pollutants.
Psychological complications, autism, retinopathy, fetal growth, and low birth weight seem to be related to long-term air pollution ( 83 ). The etiologic agent of the neurodegenerative diseases (Alzheimer's and Parkinson's) is not yet known, although it is believed that extended exposure to air pollution seems to be a factor. Specifically, pesticides and metals are cited as etiological factors, together with diet. The mechanisms in the development of neurodegenerative disease include oxidative stress, protein aggregation, inflammation, and mitochondrial impairment in neurons ( 104 ) ( Figure 1 ).
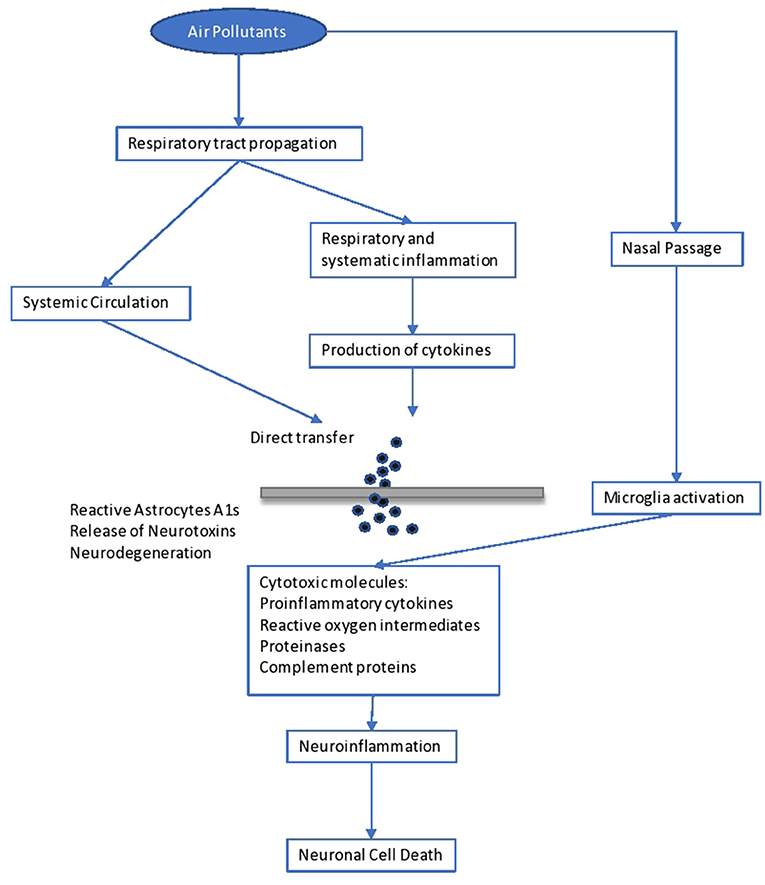
Figure 1 . Impact of air pollutants on the brain.
Brain inflammation was observed in dogs living in a highly polluted area in Mexico for a long period ( 105 ). In human adults, markers of systemic inflammation (IL-6 and fibrinogen) were found to be increased as an immediate response to PNC on the IL-6 level, possibly leading to the production of acute-phase proteins ( 106 ). The progression of atherosclerosis and oxidative stress seem to be the mechanisms involved in the neurological disturbances caused by long-term air pollution. Inflammation comes secondary to the oxidative stress and seems to be involved in the impairment of developmental maturation, affecting multiple organs ( 105 , 107 ). Similarly, other factors seem to be involved in the developmental maturation, which define the vulnerability to long-term air pollution. These include birthweight, maternal smoking, genetic background and socioeconomic environment, as well as education level.
However, diet, starting from breast-feeding, is another determinant factor. Diet is the main source of antioxidants, which play a key role in our protection against air pollutants ( 108 ). Antioxidants are free radical scavengers and limit the interaction of free radicals in the brain ( 108 ). Similarly, genetic background may result in a differential susceptibility toward the oxidative stress pathway ( 60 ). For example, antioxidant supplementation with vitamins C and E appears to modulate the effect of ozone in asthmatic children homozygous for the GSTM1 null allele ( 61 ). Inflammatory cytokines released in the periphery (e.g., respiratory epithelia) upregulate the innate immune Toll-like receptor 2. Such activation and the subsequent events leading to neurodegeneration have recently been observed in lung lavage in mice exposed to ambient Los Angeles (CA, USA) particulate matter ( 61 ). In children, neurodevelopmental morbidities were observed after lead exposure. These children developed aggressive and delinquent behavior, reduced intelligence, learning difficulties, and hyperactivity ( 109 ). No level of lead exposure seems to be “safe,” and the scientific community has asked the Centers for Disease Control and Prevention (CDC) to reduce the current screening guideline of 10 μg/dl ( 109 ).
It is important to state that impact on the immune system, causing dysfunction and neuroinflammation ( 104 ), is related to poor air quality. Yet, increases in serum levels of immunoglobulins (IgA, IgM) and the complement component C3 are observed ( 106 ). Another issue is that antigen presentation is affected by air pollutants, as there is an upregulation of costimulatory molecules such as CD80 and CD86 on macrophages ( 110 ).
As is known, skin is our shield against ultraviolet radiation (UVR) and other pollutants, as it is the most exterior layer of our body. Traffic-related pollutants, such as PAHs, VOCs, oxides, and PM, may cause pigmented spots on our skin ( 111 ). On the one hand, as already stated, when pollutants penetrate through the skin or are inhaled, damage to the organs is observed, as some of these pollutants are mutagenic and carcinogenic, and, specifically, they affect the liver and lung. On the other hand, air pollutants (and those in the troposphere) reduce the adverse effects of ultraviolet radiation UVR in polluted urban areas ( 111 ). Air pollutants absorbed by the human skin may contribute to skin aging, psoriasis, acne, urticaria, eczema, and atopic dermatitis ( 111 ), usually caused by exposure to oxides and photochemical smoke ( 111 ). Exposure to PM and cigarette smoking act as skin-aging agents, causing spots, dyschromia, and wrinkles. Lastly, pollutants have been associated with skin cancer ( 111 ).
Higher morbidity is reported to fetuses and children when exposed to the above dangers. Impairment in fetal growth, low birth weight, and autism have been reported ( 112 ).
Another exterior organ that may be affected is the eye. Contamination usually comes from suspended pollutants and may result in asymptomatic eye outcomes, irritation ( 112 ), retinopathy, or dry eye syndrome ( 113 , 114 ).
Environmental Impact of Air Pollution
Air pollution is harming not only human health but also the environment ( 115 ) in which we live. The most important environmental effects are as follows.
Acid rain is wet (rain, fog, snow) or dry (particulates and gas) precipitation containing toxic amounts of nitric and sulfuric acids. They are able to acidify the water and soil environments, damage trees and plantations, and even damage buildings and outdoor sculptures, constructions, and statues.
Haze is produced when fine particles are dispersed in the air and reduce the transparency of the atmosphere. It is caused by gas emissions in the air coming from industrial facilities, power plants, automobiles, and trucks.
Ozone , as discussed previously, occurs both at ground level and in the upper level (stratosphere) of the Earth's atmosphere. Stratospheric ozone is protecting us from the Sun's harmful ultraviolet (UV) rays. In contrast, ground-level ozone is harmful to human health and is a pollutant. Unfortunately, stratospheric ozone is gradually damaged by ozone-depleting substances (i.e., chemicals, pesticides, and aerosols). If this protecting stratospheric ozone layer is thinned, then UV radiation can reach our Earth, with harmful effects for human life (skin cancer) ( 116 ) and crops ( 117 ). In plants, ozone penetrates through the stomata, inducing them to close, which blocks CO 2 transfer and induces a reduction in photosynthesis ( 118 ).
Global climate change is an important issue that concerns mankind. As is known, the “greenhouse effect” keeps the Earth's temperature stable. Unhappily, anthropogenic activities have destroyed this protecting temperature effect by producing large amounts of greenhouse gases, and global warming is mounting, with harmful effects on human health, animals, forests, wildlife, agriculture, and the water environment. A report states that global warming is adding to the health risks of poor people ( 119 ).
People living in poorly constructed buildings in warm-climate countries are at high risk for heat-related health problems as temperatures mount ( 119 ).
Wildlife is burdened by toxic pollutants coming from the air, soil, or the water ecosystem and, in this way, animals can develop health problems when exposed to high levels of pollutants. Reproductive failure and birth effects have been reported.
Eutrophication is occurring when elevated concentrations of nutrients (especially nitrogen) stimulate the blooming of aquatic algae, which can cause a disequilibration in the diversity of fish and their deaths.
Without a doubt, there is a critical concentration of pollution that an ecosystem can tolerate without being destroyed, which is associated with the ecosystem's capacity to neutralize acidity. The Canada Acid Rain Program established this load at 20 kg/ha/yr ( 120 ).
Hence, air pollution has deleterious effects on both soil and water ( 121 ). Concerning PM as an air pollutant, its impact on crop yield and food productivity has been reported. Its impact on watery bodies is associated with the survival of living organisms and fishes and their productivity potential ( 121 ).
An impairment in photosynthetic rhythm and metabolism is observed in plants exposed to the effects of ozone ( 121 ).
Sulfur and nitrogen oxides are involved in the formation of acid rain and are harmful to plants and marine organisms.
Last but not least, as mentioned above, the toxicity associated with lead and other metals is the main threat to our ecosystems (air, water, and soil) and living creatures ( 121 ).
In 2018, during the first WHO Global Conference on Air Pollution and Health, the WHO's General Director, Dr. Tedros Adhanom Ghebreyesus, called air pollution a “silent public health emergency” and “the new tobacco” ( 122 ).
Undoubtedly, children are particularly vulnerable to air pollution, especially during their development. Air pollution has adverse effects on our lives in many different respects.
Diseases associated with air pollution have not only an important economic impact but also a societal impact due to absences from productive work and school.
Despite the difficulty of eradicating the problem of anthropogenic environmental pollution, a successful solution could be envisaged as a tight collaboration of authorities, bodies, and doctors to regularize the situation. Governments should spread sufficient information and educate people and should involve professionals in these issues so as to control the emergence of the problem successfully.
Technologies to reduce air pollution at the source must be established and should be used in all industries and power plants. The Kyoto Protocol of 1997 set as a major target the reduction of GHG emissions to below 5% by 2012 ( 123 ). This was followed by the Copenhagen summit, 2009 ( 124 ), and then the Durban summit of 2011 ( 125 ), where it was decided to keep to the same line of action. The Kyoto protocol and the subsequent ones were ratified by many countries. Among the pioneers who adopted this important protocol for the world's environmental and climate “health” was China ( 3 ). As is known, China is a fast-developing economy and its GDP (Gross Domestic Product) is expected to be very high by 2050, which is defined as the year of dissolution of the protocol for the decrease in gas emissions.
A more recent international agreement of crucial importance for climate change is the Paris Agreement of 2015, issued by the UNFCCC (United Nations Climate Change Committee). This latest agreement was ratified by a plethora of UN (United Nations) countries as well as the countries of the European Union ( 126 ). In this vein, parties should promote actions and measures to enhance numerous aspects around the subject. Boosting education, training, public awareness, and public participation are some of the relevant actions for maximizing the opportunities to achieve the targets and goals on the crucial matter of climate change and environmental pollution ( 126 ). Without any doubt, technological improvements makes our world easier and it seems difficult to reduce the harmful impact caused by gas emissions, we could limit its use by seeking reliable approaches.
Synopsizing, a global prevention policy should be designed in order to combat anthropogenic air pollution as a complement to the correct handling of the adverse health effects associated with air pollution. Sustainable development practices should be applied, together with information coming from research in order to handle the problem effectively.
At this point, international cooperation in terms of research, development, administration policy, monitoring, and politics is vital for effective pollution control. Legislation concerning air pollution must be aligned and updated, and policy makers should propose the design of a powerful tool of environmental and health protection. As a result, the main proposal of this essay is that we should focus on fostering local structures to promote experience and practice and extrapolate these to the international level through developing effective policies for sustainable management of ecosystems.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
IM is employed by the company Delphis S.A.
The remaining authors declare that the present review paper was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. WHO. Air Pollution . WHO. Available online at: http://www.who.int/airpollution/en/ (accessed October 5, 2019).
Google Scholar
2. Moores FC. Climate change and air pollution: exploring the synergies and potential for mitigation in industrializing countries. Sustainability . (2009) 1:43–54. doi: 10.3390/su1010043
CrossRef Full Text | Google Scholar
3. USGCRP (2009). Global Climate Change Impacts in the United States. In: Karl TR, Melillo JM, Peterson TC, editors. Climate Change Impacts by Sectors: Ecosystems . New York, NY: United States Global Change Research Program. Cambridge University Press.
4. Marlon JR, Bloodhart B, Ballew MT, Rolfe-Redding J, Roser-Renouf C, Leiserowitz A, et al. (2019). How hope and doubt affect climate change mobilization. Front. Commun. 4:20. doi: 10.3389/fcomm.2019.00020
5. Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long- term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int . (2014) 70:95–105. doi: 10.1016/j.envint.2014.05.014
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Kelishadi R, Poursafa P. Air pollution and non-respiratory health hazards for children. Arch Med Sci . (2010) 6:483–95. doi: 10.5114/aoms.2010.14458
7. Manucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health . (2017) 14:1048. doi: 10.3390/ijerph14091048
8. Burden of Disease from Ambient and Household Air Pollution . Available online: http://who.int/phe/health_topics/outdoorair/databases/en/ (accessed August 15, 2017).
9. Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health . (2014) 80:393–411. doi: 10.1016/j.aogh.2014.10.002
10. Guo Y, Zeng H, Zheng R, Li S, Pereira G, Liu Q, et al. The burden of lung cancer mortality attributable to fine particles in China. Total Environ Sci . (2017) 579:1460–6. doi: 10.1016/j.scitotenv.2016.11.147
11. Hou Q, An XQ, Wang Y, Guo JP. An evaluation of resident exposure to respirable particulate matter and health economic loss in Beijing during Beijing 2008 Olympic Games. Sci Total Environ . (2010) 408:4026–32. doi: 10.1016/j.scitotenv.2009.12.030
12. Kan H, Chen R, Tong S. Ambient air pollution, climate change, and population health in China. Environ Int . (2012) 42:10–9. doi: 10.1016/j.envint.2011.03.003
13. Burroughs Peña MS, Rollins A. Environmental exposures and cardiovascular disease: a challenge for health and development in low- and middle-income countries. Cardiol Clin . (2017) 35:71–86. doi: 10.1016/j.ccl.2016.09.001
14. Kankaria A, Nongkynrih B, Gupta S. Indoor air pollution in india: implications on health and its control. Indian J Comm Med . 39:203–7. doi: 10.4103/0970-0218.143019
15. Parajuli I, Lee H, Shrestha KR. Indoor air quality and ventilation assessment of rural mountainous households of Nepal. Int J Sust Built Env . (2016) 5:301–11. doi: 10.1016/j.ijsbe.2016.08.003
16. Saud T, Gautam R, Mandal TK, Gadi R, Singh DP, Sharma SK. Emission estimates of organic and elemental carbon from household biomass fuel used over the Indo-Gangetic Plain (IGP), India. Atmos Environ . (2012) 61:212–20. doi: 10.1016/j.atmosenv.2012.07.030
17. Singh DP, Gadi R, Mandal TK, Saud T, Saxena M, Sharma SK. Emissions estimates of PAH from biomass fuels used in rural sector of Indo-Gangetic Plains of India. Atmos Environ . (2013) 68:120–6. doi: 10.1016/j.atmosenv.2012.11.042
18. Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M BN. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ . (2008) 86:390–4. doi: 10.2471/BLT.07.044529
19. Kassomenos P, Kelessis A, Petrakakis M, Zoumakis N, Christides T, Paschalidou AK. Air Quality assessment in a heavily-polluted urban Mediterranean environment through Air Quality indices. Ecol Indic . (2012) 18:259–68. doi: 10.1016/j.ecolind.2011.11.021
20. Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med . (1993) 329:1753–9. doi: 10.1056/NEJM199312093292401
21. Schwela DH, Köth-Jahr I. Leitfaden für die Aufstellung von Luftreinhalteplänen [Guidelines for the Implementation of Clean Air Implementation Plans]. Landesumweltamt des Landes Nordrhein Westfalen. State Environmental Service of the State of North Rhine-Westphalia (1994).
22. Newlands M. Environmental Activism, Environmental Politics, and Representation: The Framing of the British Environmental Activist Movement . Ph.D. thesis. University of East London, United Kingdom (2015).
23. NEPIS (National Service Center for Environmental Publications) US EPA (Environmental Protection Agency) (2017). Available online at: https://www.epa.gov/clean-air-act-overview/air-pollution-current-and-future-challenges (accessed August 15, 2017).
24. NRC (National Research Council). Available online at: https://www.nap.edu/read/10728/chapter/1,2014 (accessed September 17, 2019).
25. Bull A. Traffic Congestion: The Problem and How to Deal With It . Santiago: Nationes Unidas, Cepal (2003).
26. Spiegel J, Maystre LY. Environmental Pollution Control, Part VII - The Environment, Chapter 55, Encyclopedia of Occupational Health and Safety . Available online at: http://www.ilocis.org/documents/chpt55e.htm (accessed September 17, 2019).
27. European Community Reports. Assessment of the Effectiveness of European Air Quality Policies and Measures: Case Study 2; Comparison of the EU and US Air Quality Standards and Planning Requirements. (2004). Available online at: https://ec.europa.eu/environment/archives/cafe/activities/pdf/case_study2.pdf (accessed September 22, 2019).
28. Gibson R, Ward S. Parties in the digital age; a review. J Represent Democracy . (2009) 45:87–100. doi: 10.1080/00344890802710888
29. Kaun A, Uldam J. Digital activism: after the hype. New Media Soc. (2017) 20:2099–106. doi: 10.1177/14614448177319
30. Sivitanides M, Shah V. The era of digital activism. In: 2011 Conference for Information Systems Applied Research(CONISAR) Proceedings Wilmington North Carolina, USA . Available online at: https://www.arifyildirim.com/ilt510/marcos.sivitanides.vivek.shah.pdf (accessed September 22, 2019).
31. Möller L, Schuetzle D, Autrup H. Future research needs associated with the assessment of potential human health risks from exposure to toxic ambient air pollutants. Environ Health Perspect . (1994) 102(Suppl. 4):193–210. doi: 10.1289/ehp.94102s4193
32. Jacobson MZ, Jacobson PMZ. Atmospheric Pollution: History, Science, and Regulation. Cambridge University Press (2002). p. 206. doi: 10.1256/wea.243.02
33. Stover RH. Flooding of soil for disease control. In: Mulder D, editor. Chapter 3. Developments in Agricultural and Managed Forest Ecology . Elsevier (1979). p. 19–28. Available online at: http://www.sciencedirect.com/science/article/pii/B9780444416926500094 doi: 10.1016/B978-0-444-41692-6.50009-4 (accessed July 1, 2019).
34. Maipa V, Alamanos Y, Bezirtzoglou E. Seasonal fluctuation of bacterial indicators in coastal waters. Microb Ecol Health Dis . (2001) 13:143–6. doi: 10.1080/089106001750462687
35. Bezirtzoglou E, Dimitriou D, Panagiou A. Occurrence of Clostridium perfringens in river water by using a new procedure. Anaerobe . (1996) 2:169–73. doi: 10.1006/anae.1996.0022
36. Kjellstrom T, Lodh M, McMichael T, Ranmuthugala G, Shrestha R, Kingsland S. Air and Water Pollution: Burden and Strategies for Control. DCP, Chapter 43. 817–32 p. Available online at: https://www.dcp-3.org/sites/default/files/dcp2/DCP43.pdf (accessed September 17, 2017).
37. Pathak RK, Wang T, Ho KF, Lee SC. Characteristics of summertime PM2.5 organic and elemental carbon in four major Chinese cities: implications of high acidity for water- soluble organic carbon (WSOC). Atmos Environ . (2011) 45:318–25. doi: 10.1016/j.atmosenv.2010.10.021
38. Bonavigo L, Zucchetti M, Mankolli H. Water radioactive pollution and related environmental aspects. J Int Env Appl Sci . (2009) 4:357–63
39. World Health Organization (WHO). Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease . 1106 p. Available online at: https://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf (accessed September 22, 2019).
40. Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health . (2015) 12:12735–60. doi: 10.3390/ijerph121012735
41. Ethical Unicorn. Everything You Need To Know About Aerosols & Air Pollution. (2019). Available online at: https://ethicalunicorn.com/2019/04/29/everything-you-need-to-know-about-aerosols-air-pollution/ (accessed October 4, 2019).
42. Colbeck I, Lazaridis M. Aerosols and environmental pollution. Sci Nat . (2009) 97:117–31. doi: 10.1007/s00114-009-0594-x
43. Incecik S, Gertler A, Kassomenos P. Aerosols and air quality. Sci Total Env . (2014) 355, 488–9. doi: 10.1016/j.scitotenv.2014.04.012
44. D'Amato G, Pawankar R, Vitale C, Maurizia L. Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res . (2016) 8:391–5. doi: 10.4168/aair.2016.8.5.391
45. Bezirtzoglou C, Dekas K, Charvalos E. Climate changes, environment and infection: facts, scenarios and growing awareness from the public health community within Europe. Anaerobe . (2011) 17:337–40. doi: 10.1016/j.anaerobe.2011.05.016
46. Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect . (2017) 23:283–9. doi: 10.1016/j.cmi.2017.03.012
47. Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis . (2007) 13:1–5. doi: 10.3201/eid1301.060779
48. Fenn B. Malnutrition in Humanitarian Emergencies . Available online at: https://www.who.int/diseasecontrol_emergencies/publications/idhe_2009_london_malnutrition_fenn.pdf . (accessed August 15, 2017).
49. Lindh E, Argentini C, Remoli ME, Fortuna C, Faggioni G, Benedetti E, et al. The Italian 2017 outbreak Chikungunya virus belongs to an emerging Aedes albopictus –adapted virus cluster introduced from the Indian subcontinent. Open Forum Infect Dis. (2019) 6:ofy321. doi: 10.1093/ofid/ofy321
50. Calba C, Guerbois-Galla M, Franke F, Jeannin C, Auzet-Caillaud M, Grard G, Pigaglio L, Decoppet A, et al. Preliminary report of an autochthonous chikungunya outbreak in France, July to September 2017. Eur Surveill . (2017) 22:17-00647. doi: 10.2807/1560-7917.ES.2017.22.39.17-00647
51. Menne B, Murray V. Floods in the WHO European Region: Health Effects and Their Prevention . Copenhagen: WHO; Weltgesundheits organisation, Regionalbüro für Europa (2013). Available online at: http://www.euro.who.int/data/assets/pdf_file/0020/189020/e96853.pdf (accessed 15 August 2017).
52. Schneider SH. The greenhouse effect: science and policy. Science . (1989) 243:771–81. doi: 10.1126/science.243.4892.771
53. Wilson WE, Suh HH. Fine particles and coarse particles: concentration relationships relevant to epidemiologic studies. J Air Waste Manag Assoc . (1997) 47:1238–49. doi: 10.1080/10473289.1997.10464074
54. US EPA (US Environmental Protection Agency) (2018). Available online at: https://www.epa.gov/pm-pollution/particulate-matter-pm-basics (accessed September 22, 2018).
55. Cheung K, Daher N, Kam W, Shafer MM, Ning Z, Schauer JJ, et al. Spatial and temporal variation of chemical composition and mass closure of ambient coarse particulate matter (PM10–2.5) in the Los Angeles area. Atmos Environ . (2011) 45:2651–62. doi: 10.1016/j.atmosenv.2011.02.066
56. Zhang L, Yang Y, Li Y, Qian ZM, Xiao W, Wang X, et al. Short-term and long-term effects of PM2.5 on acute nasopharyngitis in 10 communities of Guangdong, China. Sci Total Env. (2019) 688:136–42. doi: 10.1016/j.scitotenv.2019.05.470.
57. Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD. Long- and short-term exposure to PM2.5 and mortality using novel exposure models, Epidemiology . (2013) 24:555–61. doi: 10.1097/EDE.0b013e318294beaa
58. New Hampshire Department of Environmental Services. Current and Forecasted Air Quality in New Hampshire . Environmental Fact Sheet (2019). Available online at: https://www.des.nh.gov/organization/commissioner/pip/factsheets/ard/documents/ard-16.pdf (accessed September 22, 2019).
59. Kappos AD, Bruckmann P, Eikmann T, Englert N, Heinrich U, Höppe P, et al. Health effects of particles in ambient air. Int J Hyg Environ Health . (2004) 207:399–407. doi: 10.1078/1438-4639-00306
60. Boschi N (Ed.). Defining an educational framework for indoor air sciences education. In: Education and Training in Indoor Air Sciences . Luxembourg: Springer Science & Business Media (2012). 245 p.
61. Heal MR, Kumar P, Harrison RM. Particles, air quality, policy and health. Chem Soc Rev . (2012) 41:6606–30. doi: 10.1039/c2cs35076a
62. Bezirtzoglou E, Alexopoulos A. Ozone history and ecosystems: a goliath from impacts to advance industrial benefits and interests, to environmental and therapeutical strategies. In: Ozone Depletion, Chemistry and Impacts. (2009). p. 135–45.
63. Villányi V, Turk B, Franc B, Csintalan Z. Ozone Pollution and its Bioindication. In: Villányi V, editor. Air Pollution . London: Intech Open (2010). doi: 10.5772/10047
64. Massachusetts Department of Public Health. Massachusetts State Health Assessment . Boston, MA (2017). Available online at: https://www.mass.gov/files/documents/2017/11/03/2017%20MA%20SHA%20final%20compressed.pdf (accessed October 30, 2017).
65. Lorenzini G, Saitanis C. Ozone: A Novel Plant “Pathogen.” In: Sanitá di Toppi L, Pawlik-Skowrońska B, editors. Abiotic Stresses in Plant Springer Link (2003). p. 205–29. doi: 10.1007/978-94-017-0255-3_8
66. Fares S, Vargas R, Detto M, Goldstein AH, Karlik J, Paoletti E, et al. Tropospheric ozone reduces carbon assimilation in trees: estimates from analysis of continuous flux measurements. Glob Change Biol . (2013) 19:2427–43. doi: 10.1111/gcb.12222
67. Harmens H, Mills G, Hayes F, Jones L, Norris D, Fuhrer J. Air Pollution and Vegetation . ICP Vegetation Annual Report 2006/2007. (2012)
68. Emberson LD, Pleijel H, Ainsworth EA, den Berg M, Ren W, Osborne S, et al. Ozone effects on crops and consideration in crop models. Eur J Agron . (2018) 100:19–34. doi: 10.1016/j.eja.2018.06.002
69. Alexopoulos A, Plessas S, Ceciu S, Lazar V, Mantzourani I, Voidarou C, et al. Evaluation of ozone efficacy on the reduction of microbial population of fresh cut lettuce ( Lactuca sativa ) and green bell pepper ( Capsicum annuum ). Food Control . (2013) 30:491–6. doi: 10.1016/j.foodcont.2012.09.018
70. Alexopoulos A, Plessas S, Kourkoutas Y, Stefanis C, Vavias S, Voidarou C, et al. Experimental effect of ozone upon the microbial flora of commercially produced dairy fermented products. Int J Food Microbiol . (2017) 246:5–11. doi: 10.1016/j.ijfoodmicro.2017.01.018
71. Maggio A, Fagnano M. Ozone damages to mediterranean crops: physiological responses. Ital J Agron . (2008) 13–20. doi: 10.4081/ija.2008.13
72. McCarthy JT, Pelle E, Dong K, Brahmbhatt K, Yarosh D, Pernodet N. Effects of ozone in normal human epidermal keratinocytes. Exp Dermatol . (2013) 22:360–1. doi: 10.1111/exd.12125
73. WHO. Health Risks of Ozone From Long-Range Transboundary Air Pollution . Available online at: http://www.euro.who.int/data/assets/pdf_file/0005/78647/E91843.pdf (accessed August 15, 2019).
74. Thiele JJ, Traber MG, Tsang K, Cross CE, Packer L. In vivo exposure to ozone depletes vitamins C and E and induces lipid peroxidation in epidermal layers of murine skin. Free Radic Biol Med. (1997) 23:365–91. doi: 10.1016/S0891-5849(96)00617-X
75. Hatch GE, Slade R, Harris LP, McDonnell WF, Devlin RB, Koren HS, et al. Ozone dose and effect in humans and rats. A comparison using oxygen- 18 labeling and bronchoalveolar lavage. Am J Respir Crit Care Med . (1994) 150:676–83. doi: 10.1164/ajrccm.150.3.8087337
76. Lippmann M. Health effects of ozone. A critical review. JAPCA . (1989) 39:672–95. doi: 10.1080/08940630.1989.10466554
77. Gryparis A, Forsberg B, Katsouyanni K, Analitis A, Touloumi G, Schwartz J, et al. Acute effects of ozone on mortality from the “air pollution and health: a European approach” project. Am J Respir Crit Care Med . (2004) 170:1080–7. doi: 10.1164/rccm.200403-333OC
78. Soon W, Baliunas SL, Robinson AB, Robinson ZW. Environmental effects of increased atmospheric carbon dioxide. Climate Res . (1999) 13:149–64 doi: 10.1260/0958305991499694
79. Richmont-Bryant J, Owen RC, Graham S, Snyder M, McDow S, Oakes M, et al. Estimation of on-road NO2 concentrations, NO2/NOX ratios, and related roadway gradients from near-road monitoring data. Air Qual Atm Health . (2017) 10:611–25. doi: 10.1007/s11869-016-0455-7
80. Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA. Critical review of the human data on short-term nitrogen dioxide (NO 2 ) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol . (2009) 39:743–81. doi: 10.3109/10408440903294945
81. Chen T-M, Gokhale J, Shofer S, Kuschner WG. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci . (2007) 333:249–56. doi: 10.1097/MAJ.0b013e31803b900f
82. US EPA. Table of Historical SO 2 NAAQS, Sulfur US EPA . Available online at: https://www3.epa.gov/ttn/naaqs/standards/so2/s_so2_history.html (accessed October 5, 2019).
83. WHO Regional Office of Europe (2000). Available online at: https://euro.who.int/_data/assets/pdf_file/0020/123086/AQG2ndEd_7_4Sulfuroxide.pdf
84. Pruss-Ustun A, Fewrell L, Landrigan PJ, Ayuso-Mateos JL. Lead exposure. Comparative Quantification of Health Risks . World Health Organization. p. 1495–1542. Available online at: https://www.who.int/publications/cra/chapters/volume2/1495-1542.pdf?ua=1
PubMed Abstract | Google Scholar
85. Goyer RA. Transplacental transport of lead. Environ Health Perspect . (1990) 89:101–5. doi: 10.1289/ehp.9089101
86. National Institute of Environmental Health Sciences (NIH). Lead and Your Health . (2013). 1–4 p. Available online at: https://www.niehs.nih.gov/health/materials/lead_and_your_health_508.pdf (accessed September 17, 2019).
87. Farhat A, Mohammadzadeh A, Balali-Mood M, Aghajanpoor-Pasha M, Ravanshad Y. Correlation of blood lead level in mothers and exclusively breastfed infants: a study on infants aged less than six months. Asia Pac J Med Toxicol . (2013) 2:150–2.
88. Assi MA, Hezmee MNM, Haron AW, Sabri MYM, Rajion MA. The detrimental effects of lead on human and animal health. Vet World . (2016) 9:660–71. doi: 10.14202/vetworld.2016.660-671
89. Abdel-Shafy HI, Mansour MSM. A review on polycyclic aromatic hydrocarbons: source, environmental impact, effect on human health and remediation. Egypt J Pet . (2016) 25:107–23. doi: 10.1016/j.ejpe.2015.03.011
90. Kumar A, Singh BP, Punia M, Singh D, Kumar K, Jain VK. Assessment of indoor air concentrations of VOCs and their associated health risks in the library of Jawaharlal Nehru University, New Delhi. Environ Sci Pollut Res Int . (2014) 21:2240–8. doi: 10.1007/s11356-013-2150-7
91. Molhave L, Clausen G, Berglund B, Ceaurriz J, Kettrup A, Lindvall T, et al. Total Volatile Organic Compounds (TVOC) in Indoor Air Quality Investigations. Indoor Air . 7:225–240. doi: 10.1111/j.1600-0668.1997.00002.x
92. Gibb T. Indoor Air Quality May be Hazardous to Your Health . MSU Extension. Available online at: https://www.canr.msu.edu/news/indoor_air_quality_may_be_hazardous_to_your_health (accessed October 5, 2019).
93. Ebersviller S, Lichtveld K, Sexton KG, Zavala J, Lin Y-H, Jaspers I, et al. Gaseous VOCs rapidly modify particulate matter and its biological effects – Part 1: simple VOCs and model PM. Atmos Chem Phys Discuss . (2012) 12:5065–105. doi: 10.5194/acpd-12-5065-2012
94. WHO (World Health Organization). Dioxins and Their Effects on Human Health. Available online at: https://www.who.int/news-room/fact-sheets/detail/dioxins-and-their-effects-on-human-health (accessed October 5, 2019).
95. EEA (European Environmental Agency). Air Quality Standards to the European Union and WHO . Available online at: https://www.eea.europa.eu/themes/data-and-maps/figures/air-quality-standards-under-the
96. Nakano T, Otsuki T. [Environmental air pollutants and the risk of cancer]. (Japanese). Gan To Kagaku Ryoho . (2013) 40:1441–5.
97. Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med . (2016) 22:138–43. doi: 10.1097/MCP.0000000000000248
98. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet . (2014) 383:1581–92. doi: 10.1016/S0140-6736(14)60617-6
99. Jiang X-Q, Mei X-D, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis . (2016) 8:E31–40.
100. Bourdrel T, Bind M-A, Béjot Y, Morel O, Argacha J-F. Cardiovascular effects of air pollution. Arch Cardiovasc Dis . (2017) 110:634–42. doi: 10.1016/j.acvd.2017.05.003
101. Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential exposure to traffic is associated with coronary atherosclerosis. Circulation . (2007) 116:489–496. doi: 10.1161/CIRCULATIONAHA.107.693622
102. Katholi RE, Couri DM. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int J Hypertens . (2011) 2011:495349. doi: 10.4061/2011/495349
103. Leary PJ, Kaufman JD, Barr RG, Bluemke DA, Curl CL, Hough CL, et al. Traffic- related air pollution and the right ventricle. the multi-ethnic study of atherosclerosis. Am J Respir Crit Care Med . (2014) 189:1093–100. doi: 10.1164/rccm.201312-2298OC
104. Genc S, Zadeoglulari Z, Fuss SH, Genc K. The adverse effects of air pollution on the nervous system. J Toxicol . (2012) 2012:782462. doi: 10.1155/2012/782462
105. Calderon-Garciduenas L, Azzarelli B, Acuna H, et al. Air pollution and brain damage. Toxicol Pathol. (2002) 30:373–89. doi: 10.1080/01926230252929954
106. Rückerl R, Greven S, Ljungman P, Aalto P, Antoniades C, Bellander T, et al. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ Health Perspect . (2007) 115:1072–80. doi: 10.1289/ehp.10021
107. Peters A, Veronesi B, Calderón-Garcidueñas L, Gehr P, Chen LC, Geiser M, et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol . (2006) 3:13–8. doi: 10.1186/1743-8977-3-13
108. Kelly FJ. Dietary antioxidants and environmental stress. Proc Nutr Soc . (2004) 63:579–85. doi: 10.1079/PNS2004388
109. Bellinger DC. Very low lead exposures and children's neurodevelopment. Curr Opin Pediatr . (2008) 20:172–7. doi: 10.1097/MOP.0b013e3282f4f97b
110. Balbo P, Silvestri M, Rossi GA, Crimi E, Burastero SE. Differential role of CD80 and CD86 on alveolar macrophages in the presentation of allergen to T lymphocytes in asthma. Clin Exp Allergy J Br Soc Allergy Clin Immunol . (2001) 31:625–36. doi: 10.1046/j.1365-2222.2001.01068.x
111. Drakaki E, Dessinioti C, Antoniou C. Air pollution and the skin. Front Environ Sci Eng China . (2014) 15:2–8. doi: 10.3389/fenvs.2014.00011
112. Weisskopf MG, Kioumourtzoglou M-A, Roberts AL. Air pollution and autism spectrum disorders: causal or confounded? Curr Environ Health Rep . (2015) 2:430–9. doi: 10.1007/s40572-015-0073-9
113. Mo Z, Fu Q, Lyu D, Zhang L, Qin Z, Tang Q, et al. Impacts of air pollution on dry eye disease among residents in Hangzhou, China: a case-crossover study. Environ Pollut . (2019) 246:183–9. doi: 10.1016/j.envpol.2018.11.109
114. Klopfer J. Effects of environmental air pollution on the eye. J Am Optom Assoc . (1989) 60:773–8.
115. Ashfaq A, Sharma P. Environmental effects of air pollution and application of engineered methods to combat the problem. J Indust Pollut Control . (2012) 29.
116. Madronich S, de Gruijl F. Skin cancer and UV radiation. Nature . (1993) 366:23–9. doi: 10.1038/366023a0
117. Teramura A. Effects of UV-B radiation on the growth and yield of crop plants. Physiol Plant . (2006) 58:415–27. doi: 10.1111/j.1399-3054.1983.tb04203.x
118. Singh E, Tiwari S, Agrawal M. Effects of elevated ozone on photosynthesis and stomatal conductance of two soybean varieties: a case study to assess impacts of one component of predicted global climate change. Plant Biol Stuttg Ger . (2009) 11(Suppl. 1):101–8. doi: 10.1111/j.1438-8677.2009.00263.x
119. Manderson L. How global Warming is Adding to the Health Risks of Poor People . The Conversation. University of the Witwatersrand. Available online at: http://theconversation.com/how-global-warming-is-adding-to-the-health-risks-of-poor-people-109520 (accessed October 5, 2019).
120. Ministers of Energy and Environment. Federal/Provincial/Territorial Ministers of Energy and Environment (Canada), editor. The Canada-Wide Acid Rain Strategy for Post-2000 . Halifax: The Ministers (1999). 11 p.
121. Zuhara S, Isaifan R. The impact of criteria air pollutants on soil and water: a review. (2018) 278–84. doi: 10.30799/jespr.133.18040205
122. WHO. First WHO Global Conference on Air Pollution and Health. (2018). Available online at: https://www.who.int/airpollution/events/conference/en/ (accessed October 6, 2019).
123. What is the Kyoto Protocol? UNFCCC . Available online at: https://unfccc.int/kyoto__protocol (accessed October 6, 2019).
124. CopenhagenClimate Change Conference (UNFCCC) . Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
125. Durban Climate Change Conference,. UNFCCC (2011). Available online at: https://unfccc.int/process-and-meetings/conferences/past-conferences/copenhagen-climate-change-conference-december-2009/copenhagen-climate-change-conference-december-2009 (accessed October 6, 2019).
126. Paris Climate Change Agreement,. (2016). Available online at: https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement
Keywords: air pollution, environment, health, public health, gas emission, policy
Citation: Manisalidis I, Stavropoulou E, Stavropoulos A and Bezirtzoglou E (2020) Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 8:14. doi: 10.3389/fpubh.2020.00014
Received: 17 October 2019; Accepted: 17 January 2020; Published: 20 February 2020.
Reviewed by:
Copyright © 2020 Manisalidis, Stavropoulou, Stavropoulos and Bezirtzoglou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ioannis Manisalidis, giannismanisal@gmail.com ; Elisavet Stavropoulou, elisabeth.stavropoulou@gmail.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
February 8, 2024
Air Pollution Threatens Millions of Lives. Now the Sources Are Shifting
As EPA tightens air pollution standards for particulate matter, new research suggests some components of that pollution could worsen with climate change
By Virginia Gewin

Sergii Kolesnikov/Getty Images
Particle-based ambient air pollution causes more than 4 million premature deaths each year globally, according to the World Health Organization. The tiniest particles—2.5 microns or smaller, known as PM 2.5 —pose the greatest health risk because they can travel deep into the lungs and may even get into the bloodstream.
Although total PM 2.5 levels have decreased 42 percent in the U.S. since 2000 as a result of clean air regulations, scientists are concerned about the health impacts of even low levels of such pollution. The U.S. Environmental Protection Agency lowered the annual national air quality standard for PM 2.5 from 12 to nine micrograms per cubic meter (µg/m 3 ) this week. EPA administrator Michael Regan said in a press conference that officials estimate the new standard will save up to $46 billion dollars in avoided health care and hospitalization costs by 2032. “Health benefits will include up to 800,000 avoided cases of asthma symptoms, 4,500 avoided premature deaths, and 290,000 avoided lost workdays,” he said. The World Health Organization adopted an even lower 5 µg/m 3 standard in 2021, citing the growing evidence of deadly harm.
Beyond investigating their size, scientists are also digging into the chemistry of airborne particles, which, unlike other regulated pollutants such as lead and ozone, encompass a wide array of solid and liquid particles from soot to nitrate. Some airborne particles are directly emitted from car tailpipes or industrial sources; others form in the atmosphere. And the balance of those is shifting. To help states meet the tougher air standards, scientists will need more detailed studies of particle sources.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In July 2022, for the first time in more than a decade, teams of scientists conducted an intensive campaign to characterize what’s in the summertime soup of particles that New York City residents breathe. The researchers measured the chemical makeup of PM 2.5 over the course of a month.
The team found that the PM 2.5 was 80 to 83 percent organic, or carbon-based —up from roughly 50 percent in 2001, according to the study, which was published January 22 in ACS ES&T Air . “Over the past 20 years, summertime particulate matter has shifted to organic aerosols due largely to the successful reductions of sulfate and other inorganic compounds,” says Tori Hass-Mitchell, the study’s lead author and a doctoral student at Yale University.
Roughly 76 percent of the total organic aerosols measured by the study in New York City were not directly emitted from a source but rather formed in the atmosphere. These so-called secondary organic aerosols are produced when gases, including volatile organic compounds (VOCs), oxidize in the atmosphere. VOCs are produced by a wide range of sources such as cars, vegetation and household chemicals, including cosmetics and cleaners , which complicates efforts to identify the most impactful sources.
Hass-Mitchell and colleagues’ paper is the first to include data from the Atmospheric Science and Chemistry Measurement Network ( ASCENT)—a network of 12 sites around the U.S. that is the first long-term monitoring system able to chemically characterize distinct particle types. Sally Ng, who led the design of the $12-million, National Science Foundation–funded network, says Europe has had similar measurement capabilities for more than five years. “It’s time for the U.S. to modernize its air quality measurement infrastructure,” says Ng, an aerosol scientist at the Georgia Institute of Technology and a co-author of the New York City study.
Recent studies have shown that secondary organic aerosols may be linked to serious health problems—especially cardiovascular disease. A study published last September in Environmental Science & Technology found that as organic aerosols oxidize, they produce highly reactive molecules that can break down human cells and cause tissue damage . Oxidized organic aerosols are the most toxic organic component of PM 2.5 , Ng says. And her work suggests that secondary organic aerosols become more toxic the longer they oxidize in the atmosphere.
Havala Pye, an EPA research scientist, co-authored a separate 2021 Nature study that found that secondary organic aerosols are strongly associated with county-level heart and lung disease death rates in the U.S. Secondary organic aerosols were associated with a 6.5 times higher mortality rate than PM 2.5 .
“There’s a good chance the aerosols are becoming more toxic on a per mass basis, and secondary organic aerosols would be part of the reason why,” says Allen Robinson, an atmospheric scientist at Colorado State University, who was not involved in the new research or Pye’s study. In other words, breathing more oxidized aerosols may be more toxic to humans. But the literature looking at health effects of individual components of PM 2.5 is messy, Robinson notes. More work is needed to unravel the impact of complex combinations of different particle sizes and chemistries in PM 2.5 , he explains. Pye also cautions that consistent results from repeated experiments are needed to verify whether secondary organic aerosols carry significantly greater health risks than other particles that make up PM 2.5 .
Will a warming climate worsen air pollution health risks?
Previous studies have found that warmer temperatures can lead to greater production of these secondary organic aerosols. Hass-Mitchell and colleagues found in the new study that secondary organic aerosol production increased by 60 percent and 42 percent in Queens and Manhattan, respectively, during a sweltering five-day heat wave in July 2022. “We should expect higher health burdens as temperatures rise in a warming climate, with potentially more frequent extreme heat events in the future,” Hass-Mitchell says.
“Secondary organic aerosols are an increasingly important contributor to particulate matter in the summertime and urban air quality, and [they have] a temperature sensitivity that is really important to keep in mind in the context of future climate scenarios,” says Drew Gentner, a chemical and environmental engineer at Yale University and senior author of the new paper. These compounds “are becoming more oxidized at higher temperatures,” he adds, and increased temperatures can cause greater emissions of reactive volatile organic compounds.
And as temperatures increase amid climate change, more frequent and severe wildfires have already begun to chip away at air quality gains in western states. Although Hass-Mitchell and colleagues didn’t observe smoke from wildfires in the summer of 2022, they expect that organic aerosols from wildfires—such as those in the smoke that choked much of the Northeast and Midwest last summer—will also play a major role as the climate changes.
Many other cities, such as Los Angeles, Atlanta and Seoul, have also documented an increasing proportion of PM 2.5 from secondary organic aerosols. But the exact mix of natural versus human-produced sources varies widely from city to city. To continue reducing PM 2.5 , “we need to understand the underlying sources and chemistry contributing to secondary organic aerosol production,” Gentner says.
Until the early 2000s, both the tools to measure secondary organic aerosols and the understanding of their formation were limited, says Benjamin Nault, a co-author of the New York City study and a research scientist at Johns Hopkins University. Currently, most instruments are designed to measure either the size or the chemistry of aerosols but not both, he says. Scientists rely on models to determine how much secondary organic aerosol comes from, for example, live vegetation, asphalt or cooking. But it’s unclear whether some sources are more harmful than others. “There are different signatures for the chemicals that come from taking a shower versus painting [a house],” he says. “Now we’re trying to understand how they come together in an urban environment.”
And that improved understanding is leading to more nuanced pollution research. “As aerosol studies advance, with increasing capabilities to examine the various chemical components of aerosols, we can ask important questions about the relative impact of those components on air quality, human health and the environment,” Gentner says. “It may be less straightforward to address secondary organic aerosol sources compared to primary sources of pollution, but studies [like ours] demonstrate that secondary organic aerosols are the biggest contributor in some urban areas.”
Reporting for this piece was supported by the Nova Institute for Health.
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Sustainability
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Study finds natural sources of air pollution exceed air quality guidelines in many regions
Press contact :.

Previous image Next image
Alongside climate change, air pollution is one of the biggest environmental threats to human health. Tiny particles known as particulate matter or PM2.5 (named for their diameter of just 2.5 micrometers or less) are a particularly hazardous type of pollutant. These particles are produced from a variety of sources, including wildfires and the burning of fossil fuels, and can enter our bloodstream, travel deep into our lungs, and cause respiratory and cardiovascular damage. Exposure to particulate matter is responsible for millions of premature deaths globally every year.
In response to the increasing body of evidence on the detrimental effects of PM2.5, the World Health Organization (WHO) recently updated its air quality guidelines , lowering its recommended annual PM2.5 exposure guideline by 50 percent, from 10 micrograms per meter cubed (μm 3 ) to 5 μm 3 . These updated guidelines signify an aggressive attempt to promote the regulation and reduction of anthropogenic emissions in order to improve global air quality.
A new study by researchers in the MIT Department of Civil and Environmental Engineering explores if the updated air quality guideline of 5 μm 3 is realistically attainable across different regions of the world, particularly if anthropogenic emissions are aggressively reduced.
The first question the researchers wanted to investigate was to what degree moving to a no-fossil-fuel future would help different regions meet this new air quality guideline.
“The answer we found is that eliminating fossil-fuel emissions would improve air quality around the world, but while this would help some regions come into compliance with the WHO guidelines, for many other regions high contributions from natural sources would impede their ability to meet that target,” says senior author Colette Heald, the Germeshausen Professor in the MIT departments of Civil and Environmental Engineering, and Earth, Atmospheric and Planetary Sciences.
The study by Heald, Professor Jesse Kroll, and graduate students Sidhant Pai and Therese Carter, published June 6 in the journal Environmental Science and Technology Letters , finds that over 90 percent of the global population is currently exposed to average annual concentrations that are higher than the recommended guideline. The authors go on to demonstrate that over 50 percent of the world’s population would still be exposed to PM2.5 concentrations that exceed the new air quality guidelines, even in the absence of all anthropogenic emissions.
This is due to the large natural sources of particulate matter — dust, sea salt, and organics from vegetation — that still exist in the atmosphere when anthropogenic emissions are removed from the air.
“If you live in parts of India or northern Africa that are exposed to large amounts of fine dust, it can be challenging to reduce PM2.5 exposures below the new guideline,” says Sidhant Pai, co-lead author and graduate student. “This study challenges us to rethink the value of different emissions abatement controls across different regions and suggests the need for a new generation of air quality metrics that can enable targeted decision-making.”
The researchers conducted a series of model simulations to explore the viability of achieving the updated PM2.5 guidelines worldwide under different emissions reduction scenarios, using 2019 as a representative baseline year.
Their model simulations used a suite of different anthropogenic sources that could be turned on and off to study the contribution of a particular source. For instance, the researchers conducted a simulation that turned off all human-based emissions in order to determine the amount of PM2.5 pollution that could be attributed to natural and fire sources. By analyzing the chemical composition of the PM2.5 aerosol in the atmosphere (e.g., dust, sulfate, and black carbon), the researchers were also able to get a more accurate understanding of the most important PM2.5 sources in a particular region. For example, elevated PM2.5 concentrations in the Amazon were shown to predominantly consist of carbon-containing aerosols from sources like deforestation fires. Conversely, nitrogen-containing aerosols were prominent in Northern Europe, with large contributions from vehicles and fertilizer usage. The two regions would thus require very different policies and methods to improve their air quality.
“Analyzing particulate pollution across individual chemical species allows for mitigation and adaptation decisions that are specific to the region, as opposed to a one-size-fits-all approach, which can be challenging to execute without an understanding of the underlying importance of different sources,” says Pai.
When the WHO air quality guidelines were last updated in 2005, they had a significant impact on environmental policies. Scientists could look at an area that was not in compliance and suggest high-level solutions to improve the region’s air quality. But as the guidelines have tightened, globally-applicable solutions to manage and improve air quality are no longer as evident.
“Another benefit of speciating is that some of the particles have different toxicity properties that are correlated to health outcomes,” says Therese Carter, co-lead author and graduate student. “It’s an important area of research that this work can help motivate. Being able to separate out that piece of the puzzle can provide epidemiologists with more insights on the different toxicity levels and the impact of specific particles on human health.”
The authors view these new findings as an opportunity to expand and iterate on the current guidelines.
“Routine and global measurements of the chemical composition of PM2.5 would give policymakers information on what interventions would most effectively improve air quality in any given location,” says Jesse Kroll, a professor in the MIT departments of Civil and Environmental Engineering and Chemical Engineering. “But it would also provide us with new insights into how different chemical species in PM2.5 affect human health."
“I hope that as we learn more about the health impacts of these different particles, our work and that of the broader atmospheric chemistry community can help inform strategies to reduce the pollutants that are most harmful to human health,” adds Heald.
Share this news article on:
Related links.
- Atmospheric Chemistry and Composition Modeling Group
- Department of Civil and Environmental Engineering
- Department of Earth, Atmospheric and Planetary Sciences
- Department of Chemical Engineering
Related Topics
- Public health
- Climate change
- Chemical engineering
- Earth and atmospheric sciences
- Atmospheric chemistry
- Environment
- Computer modeling
- Civil and environmental engineering
Related Articles

Study: Indoor air cleaners fall short on removing volatile organic compounds

New approach could change how we track extreme air pollution events

Tackling air pollution in India and the developing world
Previous item Next item
More MIT News

MIT launches new Music Technology and Computation Graduate Program
Read full story →

New security protocol shields data from attackers during cloud-based computation

How social structure influences the way people share money

Mars’ missing atmosphere could be hiding in plain sight

Startup helps people fall asleep by aligning audio signals with brainwaves
Study evaluates impacts of summer heat in U.S. prison environments
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Exposure to outdoor air pollution and its human health outcomes: A scoping review
Contributed equally to this work with: Zhuanlan Sun, Demi Zhu
Roles Writing – original draft
Affiliation Department of Management Science and Engineering, School of Economics and Management, Tongji University, Shanghai, China
Roles Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Comparative Politics, School of International and Public Affairs, Shanghai Jiaotong University, Shanghai, China
- Zhuanlan Sun,

- Published: May 16, 2019
- https://doi.org/10.1371/journal.pone.0216550
- Reader Comments
Despite considerable air pollution prevention and control measures that have been put into practice in recent years, outdoor air pollution remains one of the most important risk factors for health outcomes. To identify the potential research gaps, we conducted a scoping review focused on health outcomes affected by outdoor air pollution across the broad research area. Of the 5759 potentially relevant studies, 799 were included in the final analysis. The included studies showed an increasing publication trend from 1992 to 2008, and most of the studies were conducted in Asia, Europe, and North America. Among the eight categorized health outcomes, asthma (category: respiratory diseases) and mortality (category: health records) were the most common ones. Adverse health outcomes involving respiratory diseases among children accounted for the largest group. Out of the total included studies, 95.2% reported at least one statistically positive result, and only 0.4% showed ambiguous results. Based on our study, we suggest that the time frame of the included studies, their disease definitions, and the measurement of personal exposure to outdoor air pollution should be taken into consideration in any future research. The main limitation of this study is its potential language bias, since only English publications were included. In conclusion, this scoping review provides researchers and policy decision makers with evidence taken from multiple disciplines to show the increasing prevalence of outdoor air pollution and its adverse effects on health outcomes.
Citation: Sun Z, Zhu D (2019) Exposure to outdoor air pollution and its human health outcomes: A scoping review. PLoS ONE 14(5): e0216550. https://doi.org/10.1371/journal.pone.0216550
Editor: Mathilde Body-Malapel, University of Lille, FRANCE
Received: December 15, 2018; Accepted: April 10, 2019; Published: May 16, 2019
Copyright: © 2019 Sun, Zhu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: This work received support from Major projects of the National Social Science Fund of China, Award Number: 13&ZD176, Grant recipient: Demi Zhu.
Competing interests: The authors have declared that no competing interests exist.
Introduction
In recent years, despite considerable improvements in air pollution prevention and control, outdoor air pollution has remained a major environmental health hazard to human beings. In some developing countries, the concentrations of air quality far exceed the upper limit announced in the World Health Organization guidelines [ 1 ]. Moreover, it is widely acknowledged that outdoor air pollution increases the incidence rates of multiple diseases, such as cardiovascular disease, lung cancer, respiratory symptoms, asthma, negatively affected pregnancy, and poor birth outcomes [ 2 – 6 ].
The influence of outdoor air pollution exposure and its mechanisms continue to be hotly debated [ 7 – 11 ]. Some causal inference studies have been conducted to examine these situations [ 12 ]; these have indicated that an increase in outdoor air exposure affects people’s health outcomes both directly and indirectly [ 13 ]. However, few studies in the existing literature have examined the extent, range, and nature of the influence of outdoor air pollution with regard to human health outcomes. Thus, such research gaps need to be identified, and related fields of study need to be mapped.
Systematic reviews and meta-analyses, the most commonly used traditional approach to synthesize knowledge, use quantified data from relevant published studies in order to aggregate findings on a specific topic [ 14 ]; furthermore, they formally assesses the quality of these studies to generate precise conclusions related to the focused research question [ 15 ]. In comparison, scoping review is a more narrative type of knowledge synthesis, and it focuses on a broader area [ 16 ] of the evidence pertaining to a given topic. It is often used to systematically summarize the evidence available (main sources, types, and research characteristics), and it tends to be more comprehensive and helpful to policymakers at all levels.
Scoping reviews have already been used to examine a variety of health related issues [ 17 ]. As an evidence synthesis approach that is still in the midst of development, the methodology framework for scoping reviews faces some controversy with regard to its conceptual clarification and definition [ 18 , 19 ], the necessity of quality assessment [ 20 – 22 ], and the time required for completion [ 19 , 21 , 23 ]. Comparing this approach with other knowledge synthesis methods, such as evidence gap map and rapid review, the scoping review has become increasingly influential for efficient evidence-based decision-making because it offers a very broad topic scope [ 15 ].
To our knowledge, few studies have systematically reviewed the literature in the broad field of outdoor air pollution exposure research, especially with regard to related health outcomes. To fill this gap, we conducted a comprehensive scoping review of the literature with a focus on health outcomes affected by outdoor air pollution. The purposes of this study were as follows: 1) provide a systematic overview of relevant studies; 2) identify the different types of outdoor air pollution and related health outcomes; and 3) summarize the publication characteristics and explore related research gaps.
Materials and methods
The methodology framework used in this study was initially outlined by Arksey and O’Malley [ 23 ] and further advanced by Levac et al. [ 20 ], Daudt et al. [ 21 ], and the Joanna Briggs Institute [ 24 ]. The framework was divided into six stages: identifying the research question; identifying relevant studies; study selection; charting the data; collating, summarizing and reporting the results; and consulting exercise.
Stage one: Research question identification
As recommended, we combined broader research questions with a clearly articulated scope of inquiry [ 20 ]; this included defining the concept, target population, and outcomes of interest in order to disseminate an effective search strategy. Thus, an adaptation of the “PCC” (participants, concept, context) strategy was used to guide the construction of research questions and inclusion criteria [ 24 ].
Types of participants.
There were no strict restrictions on ages, genders, ethnicity, or regions of participants. Everyone, including newborns, children, adults, pregnant women, and the elderly, suffer from health outcomes related to exposure to outdoor air pollution; hence, all groups were included in the study to ensure that the inquiry was sufficiently comprehensive.
The core concept was clearly articulated in order to guide the scope and breadth of the inquiry [ 24 ]. A list of outdoor air pollution and health outcome related terms were compiled by reviewing potential text words in the titles or abstracts of the most pertinent articles [ 25 – 33 ]; we also read the most cited literature reviews on air pollution related health outcomes. To classify the types of air pollution and health outcomes, we consulted researchers from different air pollution related disciplines. The classified results are shown in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0216550.t001
Our scoping review included studies from peer-reviewed journals. There were no restrictions in terms of the research field, time period, and geographical coverage. The intended audiences of our scoping review were researchers, physicians, and public policymakers.
Stage two: Relevant studies identification
We followed Joanna Briggs Institute’s instructions [ 24 ] to launch three-step search strategies to identify all relevant published and unpublished studies (grey literature) across the multi-disciplinary topic in an iterative way. The first step included a limited search of the entire database using keywords relevant to the topic and conducting an abstract and indexing categorizations analysis. The second step was a further search of all included databases based on the newly identified keywords and index terms. The final step was to search the reference list of the identified reports and literatures.
Electronic databases.
We conducted comprehensive literature searches by consulting with an information specialist. We searched the following three electronic databases from their inception until now: PubMed, Web of Science, and Scopus. The language of the studies included in our sample was restricted to English.
Search terms.
The search terms we used were broad enough to uncover any related literature and prevent chances of relevant information being overlooked. This process was conducted iteratively with different search item combinations to ensure that all relevant literature was captured ( S1 Table ).
The search used combinations of the following terms: 1) outdoor air pollution (ozone, sulfur dioxide, carbon monoxide, nitrogen dioxide, PM 2.5 , PM 10 , total suspended particle, suspended particulate matter, toxic air pollutant, volatile organic pollutant, nitrogen oxide) and 2) health outcomes (asthma, lung cancer, respiratory infection, respiratory disorder, diabetes, chronic respiratory disease, chronic obstructive pulmonary disease, hypertension, heart rate variability, heart attack, cardiopulmonary disease, ischemic heart disease, blood coagulation, deep vein thrombosis, stroke, morbidity, hospital admission, outpatient visit, emergency room visit, mortality, DNA methylation change, neurobehavioral function, inflammatory disease, skin disease, abortion, Alzheimer’s disease, disability, cognitive function, Parkinson’s disease).
Additional studies search.
Key, important, and top journals were read manually, reference lists and citation tracing were used to collect studies and related materials, and suggestions from specialists were considered to guarantee that the research was as comprehensive as possible.
Bibliographies Management Software (Mendeley) was used to remove duplicated literatures and manage thousands of bibliographic references that needed to be appraised to check whether they should be included in the final study selection.
Our literature retrieval generated a total of 5759 references; the majority of these (3567) were found on the Scopus electronic database, which emphasized the importance of collecting the findings on this broad topic.
Stage three: Studies selection
Our study identification picked up a large number of irrelevant studies; we needed a mechanism to include only the studies that best fit the research question. The study selection stage should be an iterative process of searching the literature, refining the search strategy, and reviewing articles for inclusion. Study inclusion and exclusion criteria were discussed by the team members at the beginning of the process, then two inter-professional researchers applied the criteria to independently review the titles and abstracts of all studies [ 21 ]. If there were any ambiguities, the full article was read to make decision about whether it should be chosen for inclusion. When disagreements on study inclusion occurred, a third specialist reviewer made the final decision. This process should be iterative to guarantee the inclusion of all relevant studies.
Inclusion and exclusion criteria.
The inclusion criteria used in our scoping study ensured that the articles were considered only if they were: 1) long-term and short-term exposure, perspective or prospective studies; 2) epidemiological time series studies; 3) meta-analysis and systematic review articles rather than the primary studies that contained the main parameters we were concerned with; 4) economic research studies using causality inference with observational data; and 5) etiology research studies on respiratory disease, cancer, and cardiovascular disease.
Articles were removed if they 1) focused exclusively on indoor air pollution exposure and 2) did not belong to peer-reviewed journals or conference papers (such as policy documents, proposals, and editorials).
Stage four: Data charting
The data extracted from the final articles were entered into a “data charting form” using the database, programmed Excel, so that the following relevant data could be recorded and charted according to the variables of interest ( Table 2 ).
https://doi.org/10.1371/journal.pone.0216550.t002
Stage five: Results collection, summarization, and report
The extracted data were categorized into topics such as people’s health types and regions of diseases caused by outdoor air exposure. Each reported topic should be provided with a clear explanation to enable future research. Finally, the scoping review results were tabulated in order to find research gaps to either enable meaningful research or obtain good pointers for policymaking.
Stage six: Consultation exercise
Our scoping review took into account the consultation phase of sharing preliminary findings with experts, all of whom are members of the Committee on Public Health and Urban Environment Management in China. This enabled us to identify additional emerging issues related to health outcomes.
The original search was conducted in May of 2018; the Web of Science, PubMed, and Scopus databases were searched, resulting in a total of 5759 potentially relevant studies. After a de-duplication of 1451 studies and the application of the inclusion criteria, 3027 studies were assessed as being irrelevant and excluded based on readings of the titles and the abstracts. In the end, 1281 studies were assessed for in-depth full-text screening. To prevent overlooking potentially relevant papers, we manually screened the top five impact factor periodicals in the database we were searching. We traced the reference lists and the cited literatures of the included studies, and then we reviewed the newly collected literatures to generate more relevant studies. Further, after preliminary consultation with experts, we included studies on two additional health outcome categories, pregnancy and children and mental disorders. Hence, 214 more potential studies were included during this process. Besides, 379 original studies of the inclusive meta-analysis and systematic review studies were removed for duplication. In total, 1116 studies were included for in-depth full-text screening analysis and 799 eligible studies were included in the end. The detailed articles selection process was shown in Fig 1 .
https://doi.org/10.1371/journal.pone.0216550.g001
The included air pollution related health outcome studies increased between 1992 and 2018, as shown in Fig 2 . Most studies were published in the last decade and more than 75% of studies (614/76.9%) were published after 2011.
The included studies increased during this period, more than 75% of studies were published after 2011.
https://doi.org/10.1371/journal.pone.0216550.g002
The general characteristics summary of all included studies are shown in Table 3 . Most studies were carried out in Asia, Europe and North America (280/35.0%, 261/32.7% and 219/27.4%, respectively). According to the category system of journal citation reports (JCR) in the Web of Science, 323/40.4% of all studies on health outcomes came from environmental science, 213/26.7% came from the field of medicine, and 24/3.0% were from economics. The top three research designs of the included studies were cohort studies, systematic reviews and meta-analyses, and time series studies (116/14.5%, 107/13.4% and 76/9.5%, respectively). Almost all included studies were published in journals (794/99.4%). The lengths of the included studies ranged from four pages [ 34 ] to over thirty-nine pages [ 35 ].
https://doi.org/10.1371/journal.pone.0216550.t003
Regions of studies
Table 4 outlines the locations in which health outcomes were affected by outdoor air pollution. The continents of Asia (277/34.7%), Europe (219/27.4%), and North America (168/21.0%) account for most of these studies. As the word cloud in Fig 3 illustrates, most of the included studies had been mainly conducted in the United States and China. About 62.8% of the studies (502) had been especially conducted in developed countries.
https://doi.org/10.1371/journal.pone.0216550.t004
Word cloud representing the country of included studies, the size of each term is in proportion to its frequency.
https://doi.org/10.1371/journal.pone.0216550.g003
Most authors (573/799) evaluated the air pollution health outcomes of their own continent, at a proportion of 71.7%.
Types of air pollution and related health outcomes
We categorized the health outcomes, by consulting with experts, into respiratory diseases, chronic diseases, cardiovascular diseases, health records, cancer, mental disorders, pregnancy and children, and other diseases ( Table 5 ). We also divided the outdoor air pollution into general air pollution gas, fine particulate matter, other hazardous substances, and a mixture of them.
https://doi.org/10.1371/journal.pone.0216550.t005
Most of the health records showed that mortality (163/286; 57.0%) was the most common health outcome related to outdoor air pollution, as is visually represented in Fig 4 . Respiratory diseases (e.g., asthma and respiratory symptoms) and cardiovascular diseases (e.g., heart disease) that resulted from exposure to outdoor air pollution were also common (69/199, 63/199 and 23/90; or 34.7%, 31.7% and 25.6%; respectively).
Word cloud representing the health outcomes of included studies, the size of each term is in proportion to its frequency.
https://doi.org/10.1371/journal.pone.0216550.g004
Types of affected groups
The population of included studies was categorized into seven subgroups: birth and infant, children, women and pregnancy, adults, elderly, all ages and not specified ( Table 6 ). The largest air pollution proportion fell under the groups of all ages and children (261/799; 32.7% and 165/799; 20.7%), health outcomes of respiratory diseases in children account for the largest groups (114/199; 57.3%).
https://doi.org/10.1371/journal.pone.0216550.t006
There were 121 research studies in the “Not Specified” group. As shown in Table 6 , the “Birth & Infant,” “Women & Pregnancy,” “Children,” and “elderly” groups occupied the subject areas of more than half of the total included studies, which means that air pollution affected these population groups more acutely. Moreover, age is a confounding factor for the prevalence of cancer and cardiovascular diseases. However, there were only 2 studies (2/38, 5.3%) on cancer and 14 studies (14/90, 15.6%) on cardiovascular diseases in the elderly group.
Summary of results
Of all included studies, 95.2% reported at least one statistically positive result, 4.4% were convincingly negative, and only 0.4% showed ambiguous results ( Table 7 ).
https://doi.org/10.1371/journal.pone.0216550.t007
There were 27 primary studies that showed no association between air pollution and disease, including cancer (n = 1), chronic diseases (n = 1), cardiovascular diseases (n = 6), health records (n = 7), pregnancy and children (n = 2), respiratory diseases (n = 6), mental disorders (n = 1), and other diseases (n = 3). Moreover, eight meta-analyses showed no evidence for any association between air pollution and disease prevalence (childhood asthma, chronic bronchitis, asthma, cardio-respiratory mortality, acute respiratory distress syndrome and acute lung injury, mental disorder, cardiovascular disease, and daily respiratory death). Three meta-analyses showed ambiguous results for mental health, venous thromboembolism, and hypertension.
Our scoping review provided an overview on the subject of outdoor air pollution and health outcomes. We adhered to the methodology outlined for publishing guidelines and used the six steps outlined by the scoping review protocol. The guiding principle ensured that our methods were transparent and free from potential bias. The strengths of the included studies are that they tend to focus on large sample sizes and broad geographical coverage. This research helped us to identify research gaps and disseminate research findings [ 23 ] to policymakers, practitioners, and consumers for further missing or potentially valuable investigations.
Principal findings
Among the included studies, we identified various health outcomes of outdoor air pollution, including respiratory diseases, chronic diseases, cardiovascular diseases, health records, cancer, mental disorders, pregnancy and children, and other diseases. Among them, asthma in respiratory diseases and mortality in health records were the most common ones. The study designs contained cohort, meta-analysis, time series, crossover, cross-sectional, and other qualitative methods. In addition, we included economically relevant studies [ 12 , 36 , 37 ] to investigate the causal inference of outdoor air pollution on health outcomes. Further, pregnancy and children, mental disorders, and other diseases are health outcomes that might have uncertain or inconsistent effects. For example, Kirrane et al. [ 38 ] reported that PM 2.5 had positive associations with Parkinson’s disease; however, some studies report that there is no statistically significant overall association between PM exposure and such diseases [ 39 ]. Overall, the majority of these studies suggested a potential positive association between outdoor air pollution and health outcomes, although several recent studies revealed no significant correlations [ 40 – 42 ].
Time frame of included studies
The time frame of included studies is one of the most important characteristics of air pollution research. Even in the same country or region, industrialization and modernization caused by air pollution is distinguished between different time periods [ 43 , 44 ]. In addition, the more the public understands environment science, the more people will take preventative measures to protect themselves. This is also influenced by time. Although air pollution should not be seen as an inevitable side effect of economic growth, time period should be considered in future studies. The publication trends with regard to air pollution related health outcome research increased sharply after 2010. In recent times, published studies have begun to pay more attention to controlling confounding factors such as socioeconomic factors and human behavior.
Population and country
More than 50% of the studies on the relationship between air pollution and health outcomes originated from high income countries. There was less research (<25%) from developing countries and poor countries [ 45 – 48 ], which may result from inadequate environmental monitoring systems and public health surveillance systems. Less cohesive policies and inadequate scientific research may be another reason. In this regard, stratified analysis by regional income will be helpful for exploring the real estimates. It is reported that the stroke incidence is largely associated with low and middle income countries rather than with high income countries [ 49 ]. More studies are urgently needed in highly populated regions, such as Eastern Asia and North and Central Africa.
It is worth noting that rural and urban differences in air pollution research have been neglected. There are only eight studies focused on the difference of spatial variability of air pollution [ 50 – 57 ]. Variation is common even across relatively small areas due to geographical, topographical, and meteorological factors. For example, an increase in PM 2.5 in Northern China was predominantly from abundant coal combustion used for heating in the winter months [ 58 ]. These differences should be considered with caution by urbanization and by region. Data analysis adjustment for spatial autocorrelation will provide a more accurate estimate of the differences in air. What’s more, in some countries such as China, migrants are not able to access healthcare within the cities; this has resulted in misleading conclusions about a “healthier” population and null based bias was introduced [ 59 ].
Other studies (including systematic reviews and economic studies) on outdoor air pollution
Our scoping review included a large number of systematic reviews and meta-analyses. Of the included 107 systematic review and meta-analyses, the most discussed topics were respiratory diseases influenced by mixed outdoor air pollution [ 60 – 62 ]. Little systematic review research focused on chronic diseases, cancer, and mental disorders, which are current research gaps and potential research directions. A large overlap remains between the primary studies included in the systematic reviews. However, some systematic reviews that focused on the same topic have conflicting results, which were mainly caused by different inclusion criteria and subgroup analyses [ 63 , 64 ]. To solve this problem, it is critical that reporting of systematic reviews should retrieve all related published systematic reviews and meta-analyses.
As for the 24 included economic studies, two kinds of health outcomes—morbidity [ 65 ] and economic cost [ 66 ]—were discussed separately using regression approaches. The economic methods were different from those used in the epidemiology; the study focused on causal inference and provided a new perspective for examining the relevant environmental health problems. Furthermore, meta-regression methodology, an economic synthesis approach, proved to be very effective for evaluating the outcomes in a comprehensive way [ 67 ].
Diagnostic criteria for diseases
The diagnostic criteria for diseases forms an important aspect of health-related outcomes. The diagnostic criteria for stroke and mental disorders might be less reliable than those for cancer, mobility, and cardiovascular diseases [ 68 ]. Few studies provided detailed disease diagnostic information on how the disease was measured. Thus, the overall effect estimation of outdoor air pollution might be overestimated. It is recommended that ICD-10 or ICD-11 classification should be adopted as the health outcome classification criterion to ensure consistency among studies in different disciplines considered in future research [ 69 ].
In spite of these broad disease definitions, studies in healthy people or individuals with chronic diseases were not conducted separately. People with chronic diseases were more susceptible to air pollution [ 70 ]. It is obvious that air pollution related population mobility might be underestimated. However, the obvious association of long-term exposure to air pollution with chronic disease related mortality has been reported by prospective cohort studies [ 71 ]. It should be translated to other diverse air pollution related effect research. The population with pre-existing diseases should be analyzed as subgroups.
Except for the overall population, subgroups of people with outdoor occupations and athletes [ 72 , 73 ], sensitive groups such as infants and children, older adults [ 74 , 75 ], and people with respiratory or cardiovascular diseases, should be analyzed separately.
Measurement of personal exposure
The measurement of personal exposure to air pollutants (e.g., measurement of errors associated with the monitoring instruments, heterogeneity in the amount of time spent outdoors, and geographic variation) was lacking in terms of accurate determination. There is a need for clear reporting of these measurements. The key criterion to determine if there is causal relationship between air pollution and negative health outcomes was that at least one aspect of these could be measured in an unbiased manner.
Pollutant dispersion factor
It is well known that the association between air pollution and stroke, and respiratory and cardiovascular disease subtype might be caused by many other factors such as temperature, humidity, season, barometric pressure, and even wind speed and rain [ 76 – 78 ]. These confounding factors related to aspects of energy, transportation, and socioeconomic status, may explain the varying effect size of the association between air pollution and diseases.
While the associations reported in epidemiological studies were significant, proving a causal relationship between the different air pollutants affected by any other factors and adverse effects has been more challenging. To avoid bias, these modifier effects should be compared with previous localized studies. In fact, how the confounding variables account for the heterogeneity should be explored by case-controlled study design or other causal interference research designs.
Study limitations
The following limitations should not be overlooked. First, scoping reviews are based on a knowledge synthesis approach that allows for the mapping of gaps in the existing literature; however, they lack quality assessment for the included studies, which may be an obstacle for precise interpretation. Some improvements have been made by adding a quality assessment [ 15 , 22 , 79 ] to increase the reliability of the findings, and other included studies control for quality by including only peer-reviewed publications [ 80 ]; however, this is not a requirement for scoping reviews. While our paper aimed to comprehensively present a broader range of global-level current published literatures related to outdoor air pollution health outcomes, we did not assess the quality of the analyzed literature. The conclusions of this scoping review were based on the existence of the selected studies rather than their intrinsic qualities.
Second, bias is an inevitable problem from the perspectives of languages, disciplines, and literatures in knowledge synthesis. We included literatures from electronic databases, key journals, and reference lists to avoid “selection bias” and then included unpublished literature to avoid “publication bias”; further, we also conscientiously sampled among the studies to ensure that there was a safeguard against “researcher bias.” We only took English language articles into account because of the cost and time involved in translating the material, which might have led to a potential language bias [ 23 ]. However, in scoping reviews, language restriction does not have the importance that it does in meta-analysis [ 81 ].
Conclusions
In all, the topic of outdoor air pollution exposure related health outcomes is discussed across multiple-disciplines. The various characteristics and contexts of different disciplines suggest different underlying mechanisms worth of the attention of researchers and policymakers. The presentation of the diversity of health outcomes and its relationship to outdoor exposure air pollution is the purpose of this scoping review for new findings in future investigations.
Supporting information
S1 table. literature search strategies..
https://doi.org/10.1371/journal.pone.0216550.s001
S2 Table. PRISMA-ScR checklist.
https://doi.org/10.1371/journal.pone.0216550.s002
Acknowledgments
The authors would like to thank Miaomiao Liu, an assistant professor in School of the Environment of Nanjing University, for her valuable advice with regard to this article.
- View Article
- PubMed/NCBI
- Google Scholar
- 24. The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI scoping reviews. Joanne Briggs Inst. 2015; 1–24.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .

Research on Health Effects from Air Pollution
Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to health and increased disease, especially in vulnerable populations. Children, the elderly, and people living in areas with high levels of air pollution are especially susceptible.
Results from these investigations are used to support the nation's air quality standards under the Clean Air Act and contribute to improvements in public health.
On this page:
Health Effects of Air Pollutants on Vulnerable Populations
Long-term and short-term effects from exposure to air pollutants.
- Multipollutant Exposures and Changes in Environmental Conditions
- Leveraging Big Data for Innovations in Health Science
Health Effects of Wildfire Smoke
Public health intervention and communications strategies, integrated science assessments for air pollutants.

Research has shown that some people are more susceptible than others to air pollutants. These groups include children, pregnant women, older adults, and individuals with pre-existing heart and lung disease. People in low socioeconomic neighborhoods and communities may be more vulnerable to air pollution because of many factors. Proximity to industrial sources of air pollution, underlying health problems, poor nutrition, stress, and other factors can contribute to increased health impacts in these communities.
There is a need for greater understanding of the factors that may influence whether a population or age group is at increased risk of health effects from air pollution. In addition, advances to analytical approaches used to study the health effects from air pollution will improve exposure estimates for healthy and at-risk groups.
The research by EPA scientists and others inform the required reviews of the primary National Ambient Air Quality Standards (NAAQS), which is done with the development of Integrated Science Assessments (ISAs). These ISAs are mandated by Congress every five years to assess the current state of the science on criteria air pollutants and determine if the standards provide adequate protection to public health.
Research is focused on addressing four areas:
- Identifying and characterizing whether there are key reproductive factors and critical stages of development that are impacted by air pollution exposures;
- Determining the role of acute and chronic sociodemographic factors in air pollution health disparities;
- Understanding how diet modifies responses to air pollution;
- Evaluating long-term lifestyle and chronic disease effects on air pollution-induced respiratory and cardiovascular responses
A multi-disciplinary team of investigators is coordinating epidemiological, human observational, and basic toxicological research to assess the effects of air pollution in at-risk populations and develop strategies to protect these populations, particularly those with pre-existing disease. The results from these products will improve risk assessments by clarifying the role of modifying factors such as psychosocial stress (e.g. noise) and diet, and determining the impact of individual susceptibility on the relationship between air pollutant exposures and health.
Related Links
- Healthy Heart Research
- Integrated Science Assessments
- Criteria Air Pollutants

People can experience exposure to varying concentrations of air pollution. Poor air quality can impact individuals for a short period of time during the day, or more frequently during a given day. Exposure to pollutants can also occur over multiple days, weeks or months due to seasonal air pollution, such as increased ozone during the summer or particulate matter from woodstoves during the winter.
The health impact of air pollution exposure depends on the duration and concentrations, and the health status of the affected populations. Studies are needed to increase knowledge of the exposure duration and the possible cumulative increase in risk.
The research is focused on three main areas:
- Short-term peak exposures, such as wildfires, traffic-related sources, or other episodic events;
- Intermittent and cumulative exposures;
- Mechanisms underlying the exposure risks
Researchers are evaluating the health responses of intermittent multiple days versus one-day air pollution exposure in controlled human exposure, animal, and in vitro models and associated cellular and molecular mechanisms. They are employing population-based models and electronic health records to assess the health effects of short-term and long-term exposures and identifying populations at greatest risk of health effects. The work is improving our understanding of the possible cumulative effects of multiple short-term peak exposures and the relationship of these exposures to longer-term exposures and risks.
Multipollutant Exposures and Changes in Environmental Conditions

EPA research is providing information to understand how individuals may respond to two or more pollutants or mixtures and how environmental conditions may impact air quality. While risk estimates for exposure to individual criteria air pollutants such as PM and ozone are well established, the acute and cumulative effects of combinations of pollutants is not well understood. In addition, research is needed to determine how changes in the environment affect both pollutant formation and subsequent responsiveness to exposures in healthy and susceptible individuals.
The research is focused on three specific questions:
- What is the role of temperature and photochemical aging on the health impact of wildfire smoke and air pollution mixtures?
- What is the effect of changing environmental conditions (i.e., temperature and humidity) on responsiveness to air pollution?
- Does prior pollutant exposure modify responsiveness to subsequent exposures?
The integrated, multi-disciplinary research includes:
- Epidemiologic analyses of environmental influences on morbidity and mortality in populations,
- Simulations of changing environmental conditions in multi-pollutant formation in atmospheric chamber studies coupled with clinical and toxicological assessments in healthy and at-risk populations,
- Evaluation of pre-exposure as a modifying effect on subsequent exposures
The results are revealing how changes in environmental conditions affect pollutant formation and subsequent health impact in at-risk populations. The research findings are informing EPA’s Integrated Science Assessments for criteria air pollutants and assisting with future regulatory decisions on the National Ambient Air Quality Standards (NAAQS).
Leveraging Big Data for Innovations in Health Science

EPA is at the cutting edge of health science, using electronic health records, novel data systems, tissue-like advanced cellular models, molecular approaches, and animal models to evaluate the health impacts of air pollution. Researchers are using these powerful new techniques to identify factors that may increase sensitivity and vulnerability to air pollution effects.
The research is building capacity for future risk assessment and regulatory analyses that go beyond traditional lines of evidence to more clearly define populations and lifestages at increased risk of health effects from air pollution.
To continue to protect public health from poor air quality, researchers must consider new epidemiological, toxicological and clinical approaches to understand the health risks of poor air quality and the biological mechanisms responsible for these risks. At the center of these new research approaches is an explosion of data availability and methodological approaches for handling large clinical and molecular datasets, also known as "big data."
While data of increasing size, depth, and complexity have accelerated research for many industries and scientific fields, big data is sometimes less recognized for the impacts it is having on environmental health studies. Increasingly, researchers are able to examine vulnerable populations with unprecedented precision and detail while also evaluating hundreds of thousands of molecular biomarkers in order to understand biological mechanisms associated with exposure.
- Development of the InTelligence And Machine LEarning (TAME) Toolkit for Introductory Data Science, Chemical-Biological Analyses, Predictive Modeling, and Database Mining for Environmental Health Research (Journal Article)

Larger and more intense wildfires are creating the potential for greater smoke production and chronic exposures in the United States, particularly in the West. Wildfires increase air pollution in surrounding areas and can affect regional air quality.
The health effects of wildfire smoke can range from eye and respiratory tract irritation to more serious disorders, including reduced lung function, exacerbation of asthma and heart failure, and premature death. Children, pregnant women, and the elderly are especially vulnerable to smoke exposure. Emissions from wildfires are known to cause increased visits to hospitals and clinics by those exposed to smoke.
It is important to more fully understand the human health effects associated with short- and long-term exposures to smoke from wildfires as well as prescribed fires, together referred to as wildland fires. EPA is conducting research to advance understanding of the health effects from different types of fires as well as combustion phases. Researchers want to know:
- What is the full extent of health effects from smoke exposure?
- Who is most at risk?
- Are there differences in health effects from different wildfire fuel types or combustion phases (burning versus flaming)?
- What strategies and approaches are most effective in protecting public health?
- What are the environmental, social and economic impacts of wildfire emissions?
- Wildland Fire Research
- Smoke-Ready Toolbox for Wildfires
- Smoke Sense Project and App

Many communities throughout the United States face challenges in providing advice to residents about how best to protect their health when they are exposed to elevated concentrations of air pollutants from motor vehicle and industrial emissions and other sources of combustion, including wildland fire smoke.
Researchers are studying intervention strategies to reduce the health impacts from exposure to air pollution as well as ways to effectively communicate these health risks. To translate the science for use in public health communication and community empowerment, EPA is collaborating with other federal agencies, such as the Centers for Disease Control and Prevention (CDC) and the National Heart, Lung, and Blood Institute (NHLBI), and state and local agencies and tribes. The objectives are to identify ways to lower air pollution exposure or mitigate the biological responses at individual, community or ecosystem levels, and ultimately evaluate whether such interventions have benefits as measured by indicators of health, well-being or economics.
Studies are evaluating the interactions between behavior and social and economic factors to more thoroughly understand how these factors may influence health and well-being outcomes, which can inform effective and consistent health risk messaging.
- Healthy Heart Toolkit and Research
- Video: Air Quality Impacts on Public Health

EPA sets National Ambient Air Quality Standards (NAAQS) for six principal criteria air pollutants —nitrogen oxides, sulfur oxides, particulate matter, carbon monoxide, ozone and lead—all of which have been shown to be harmful to public health and the environment.
The Agency’s Integrated Science Assessments (ISAs) form the scientific foundation for the review of the NAAQS standards by providing the primary (human health-based) assessments and secondary (welfare-based, e.g. ecology, visibility, materials) assessments. The ISAs are assessments of the state of the science on the criteria pollutants. They are conducted as mandated under the Clean Air Act.
- Air Research Home
- Air Monitoring & Emissions
- Air Quality Modeling
- Wildland Fires
- Health Effects from Air Pollution
- Air & Energy
- Outreach, Tools & Resources
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
New WHO Global Air Quality Guidelines aim to save millions of lives from air pollution
Air pollution is one of the biggest environmental threats to human health, alongside climate change..
New WHO Global Air Quality Guidelines (AQGs) provide clear evidence of the damage air pollution inflicts on human health, at even lower concentrations than previously understood. The guidelines recommend new air quality levels to protect the health of populations, by reducing levels of key air pollutants, some of which also contribute to climate change.
Since WHO’s last 2005 global update, there has been a marked increase of evidence that shows how air pollution affects different aspects of health. For that reason, and after a systematic review of the accumulated evidence, WHO has adjusted almost all the AQGs levels downwards, warning that exceeding the new air quality guideline levels is associated with significant risks to health. At the same time, however, adhering to them could save millions of lives.
Every year, exposure to air pollution is estimated to cause 7 million premature deaths and result in the loss of millions more healthy years of life. In children, this could include reduced lung growth and function, respiratory infections and aggravated asthma. In adults, ischaemic heart disease and stroke are the most common causes of premature death attributable to outdoor air pollution, and evidence is also emerging of other effects such as diabetes and neurodegenerative conditions. This puts the burden of disease attributable to air pollution on a par with other major global health risks such as unhealthy diet and tobacco smoking.
Air pollution is one of the biggest environmental threats to human health, alongside climate change. Improving air quality can enhance climate change mitigation efforts, while reducing emissions will in turn improve air quality. By striving to achieve these guideline levels, countries will be both protecting health as well as mitigating global climate change.
WHO’s new guidelines recommend air quality levels for 6 pollutants, where evidence has advanced the most on health effects from exposure. When action is taken on these so-called classical pollutants – particulate matter (PM), ozone (O₃), nitrogen dioxide (NO₂) sulfur dioxide (SO₂) and carbon monoxide (CO), it also has an impact on other damaging pollutants.
The health risks associated with particulate matter equal or smaller than 10 and 2.5 microns (µm) in diameter (PM₁₀ and PM₂ . ₅, respectively) are of particular public health relevance. Both PM₂ . ₅ and PM₁₀ are capable of penetrating deep into the lungs but PM₂ . ₅ can even enter the bloodstream, primarily resulting in cardiovascular and respiratory impacts, and also affecting other organs. PM is primarily generated by fuel combustion in different sectors, including transport, energy, households, industry, and from agriculture. In 2013, outdoor air pollution and particulate matter were classified as carcinogenic by WHO’s International Agency for Research on Cancer (IARC).
The guidelines also highlight good practices for the management of certain types of particulate matter (for example, black carbon/elemental carbon, ultrafine particles, particles originating from sand and dust storms) for which there is currently insufficient quantitative evidence to set air quality guideline levels. They are applicable to both outdoor and indoor environments globally, and cover all settings.
“Air pollution is a threat to health in all countries, but it hits people in low- and middle-income countries the hardest,” said WHO Director-General, Dr Tedros Adhanom Ghebreyesus. “WHO’s new Air Quality Guidelines are an evidence-based and practical tool for improving the quality of the air on which all life depends. I urge all countries and all those fighting to protect our environment to put them to use to reduce suffering and save lives.”
An unequal burden of disease
Disparities in air pollution exposure are increasing worldwide, particularly as low- and middle-income countries are experiencing growing levels of air pollution because of large-scale urbanization and economic development that has largely relied on the burning of fossil fuels.
“Annually, WHO estimates that millions of deaths are caused by the effects of air pollution, mainly from noncommunicable diseases. Clean air should be a fundamental human right and a necessary condition for healthy and productive societies. However, despite some improvements in air quality over the past three decades, millions of people continue to die prematurely, often affecting the most vulnerable and marginalized populations,” said WHO Regional Director for Europe, Dr Hans Henri P. Kluge. “We know the magnitude of the problem and we know how to solve it. These updated guidelines give policy-makers solid evidence and the necessary tool to tackle this long-term health burden.”
Global assessments of ambient air pollution alone suggest hundreds of millions of healthy life years of life lost, with the greatest attributable disease burden seen in low and middle-income countries. The more exposed to air pollution they are, the greater the health impact, particularly on individuals with chronic conditions (such as asthma, chronic obstructive pulmonary disease, and heart disease), as well as older people, children and pregnant women.
In 2019, more than 90% of the global population lived in areas where concentrations exceeded the 2005 WHO air quality guideline for long term exposure to PM₂ . ₅. Countries with strong policy-driven improvements in air quality have often seen marked reduction in air pollution, whereas declines over the past 30 years were less noticeable in regions with already good air quality.
The road to achieving recommended air quality guideline levels
The goal of the guideline is for all countries to achieve recommended air quality levels. Conscious that this will be a difficult task for many countries and regions struggling with high air pollution levels, WHO has proposed interim targets to facilitate stepwise improvement in air quality and thus gradual, but meaningful, health benefits for the population.
Almost 80% of deaths related to PM₂ . ₅ could be avoided in the world if the current air pollution levels were reduced to those proposed in the updated guideline, according to a rapid scenario analysis performed by WHO. At the same time, the achievement of interim targets would result in reducing the burden of disease, of which the greatest benefit would be observed in countries with high concentrations of fine particulates (PM₂ . ₅) and large populations.
Note to editors
Whilst not legally-binding, like all WHO guidelines, AQGs are an evidence-informed tool for policy-makers to guide legislation and policies, in order to reduce levels of air pollutants and decrease the burden of disease that results from exposure to air pollution worldwide. Their development has adhered to a rigorously defined methodology, implemented by a guideline development group. It was based on evidence obtained from six systematic reviews that considered more than 500 papers. The development of these global AQGs was overseen by a steering group led by the WHO European Centre for Environment and Health.
Media Contacts
Ceridwen Johnson
World Health Organization
James Creswick
Technical Officer (Communications) WHO Regional Office for Europe
Leticia Linn
Consultant, Communications WHO Regional Office for Europe
Andrei Muchnik
Communications Officer World Health Organization
More on air pollution
Questions and answers on the WHO Global Air Quality Guidelines
WHO global air quality guidelines. Particulate matter: (PM2.5, PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide
WHO global air quality guidelines. Particulate matter: (PM2.5, PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide: executive summary
Download our Infographics
Air Pollution: Everything You Need to Know
How smog, soot, greenhouse gases, and other top air pollutants are affecting the planet—and your health.

- Share this page block
What is air pollution?
What causes air pollution, effects of air pollution, air pollution in the united states, air pollution and environmental justice, controlling air pollution, how to help reduce air pollution, how to protect your health.
Air pollution refers to the release of pollutants into the air—pollutants that are detrimental to human health and the planet as a whole. According to the World Health Organization (WHO) , each year, indoor and outdoor air pollution is responsible for nearly seven million deaths around the globe. Ninety-nine percent of human beings currently breathe air that exceeds the WHO’s guideline limits for pollutants, with those living in low- and middle-income countries suffering the most. In the United States, the Clean Air Act , established in 1970, authorizes the U.S. Environmental Protection Agency (EPA) to safeguard public health by regulating the emissions of these harmful air pollutants.
“Most air pollution comes from energy use and production,” says John Walke , director of the Clean Air team at NRDC. Driving a car on gasoline, heating a home with oil, running a power plant on fracked gas : In each case, a fossil fuel is burned and harmful chemicals and gases are released into the air.
“We’ve made progress over the last 50 years in improving air quality in the United States, thanks to the Clean Air Act. But climate change will make it harder in the future to meet pollution standards, which are designed to protect health ,” says Walke.
Air pollution is now the world’s fourth-largest risk factor for early death. According to the 2020 State of Global Air report —which summarizes the latest scientific understanding of air pollution around the world—4.5 million deaths were linked to outdoor air pollution exposures in 2019, and another 2.2 million deaths were caused by indoor air pollution. The world’s most populous countries, China and India, continue to bear the highest burdens of disease.
“Despite improvements in reducing global average mortality rates from air pollution, this report also serves as a sobering reminder that the climate crisis threatens to worsen air pollution problems significantly,” explains Vijay Limaye , senior scientist in NRDC’s Science Office. Smog, for instance, is intensified by increased heat, forming when the weather is warmer and there’s more ultraviolet radiation. In addition, climate change increases the production of allergenic air pollutants, including mold (thanks to damp conditions caused by extreme weather and increased flooding) and pollen (due to a longer pollen season). “Climate change–fueled droughts and dry conditions are also setting the stage for dangerous wildfires,” adds Limaye. “ Wildfire smoke can linger for days and pollute the air with particulate matter hundreds of miles downwind.”
The effects of air pollution on the human body vary, depending on the type of pollutant, the length and level of exposure, and other factors, including a person’s individual health risks and the cumulative impacts of multiple pollutants or stressors.
Smog and soot
These are the two most prevalent types of air pollution. Smog (sometimes referred to as ground-level ozone) occurs when emissions from combusting fossil fuels react with sunlight. Soot—a type of particulate matter —is made up of tiny particles of chemicals, soil, smoke, dust, or allergens that are carried in the air. The sources of smog and soot are similar. “Both come from cars and trucks, factories, power plants, incinerators, engines, generally anything that combusts fossil fuels such as coal, gasoline, or natural gas,” Walke says.
Smog can irritate the eyes and throat and also damage the lungs, especially those of children, senior citizens, and people who work or exercise outdoors. It’s even worse for people who have asthma or allergies; these extra pollutants can intensify their symptoms and trigger asthma attacks. The tiniest airborne particles in soot are especially dangerous because they can penetrate the lungs and bloodstream and worsen bronchitis, lead to heart attacks, and even hasten death. In 2020, a report from Harvard’s T.H. Chan School of Public Health showed that COVID-19 mortality rates were higher in areas with more particulate matter pollution than in areas with even slightly less, showing a correlation between the virus’s deadliness and long-term exposure to air pollution.
These findings also illuminate an important environmental justice issue . Because highways and polluting facilities have historically been sited in or next to low-income neighborhoods and communities of color, the negative effects of this pollution have been disproportionately experienced by the people who live in these communities.
Hazardous air pollutants
A number of air pollutants pose severe health risks and can sometimes be fatal, even in small amounts. Almost 200 of them are regulated by law; some of the most common are mercury, lead , dioxins, and benzene. “These are also most often emitted during gas or coal combustion, incineration, or—in the case of benzene—found in gasoline,” Walke says. Benzene, classified as a carcinogen by the EPA, can cause eye, skin, and lung irritation in the short term and blood disorders in the long term. Dioxins, more typically found in food but also present in small amounts in the air, is another carcinogen that can affect the liver in the short term and harm the immune, nervous, and endocrine systems, as well as reproductive functions. Mercury attacks the central nervous system. In large amounts, lead can damage children’s brains and kidneys, and even minimal exposure can affect children’s IQ and ability to learn.
Another category of toxic compounds, polycyclic aromatic hydrocarbons (PAHs), are by-products of traffic exhaust and wildfire smoke. In large amounts, they have been linked to eye and lung irritation, blood and liver issues, and even cancer. In one study , the children of mothers exposed to PAHs during pregnancy showed slower brain-processing speeds and more pronounced symptoms of ADHD.
Greenhouse gases
While these climate pollutants don’t have the direct or immediate impacts on the human body associated with other air pollutants, like smog or hazardous chemicals, they are still harmful to our health. By trapping the earth’s heat in the atmosphere, greenhouse gases lead to warmer temperatures, which in turn lead to the hallmarks of climate change: rising sea levels, more extreme weather, heat-related deaths, and the increased transmission of infectious diseases. In 2021, carbon dioxide accounted for roughly 79 percent of the country’s total greenhouse gas emissions, and methane made up more than 11 percent. “Carbon dioxide comes from combusting fossil fuels, and methane comes from natural and industrial sources, including large amounts that are released during oil and gas drilling,” Walke says. “We emit far larger amounts of carbon dioxide, but methane is significantly more potent, so it’s also very destructive.”
Another class of greenhouse gases, hydrofluorocarbons (HFCs) , are thousands of times more powerful than carbon dioxide in their ability to trap heat. In October 2016, more than 140 countries signed the Kigali Agreement to reduce the use of these chemicals—which are found in air conditioners and refrigerators—and develop greener alternatives over time. (The United States officially signed onto the Kigali Agreement in 2022.)
Pollen and mold
Mold and allergens from trees, weeds, and grass are also carried in the air, are exacerbated by climate change, and can be hazardous to health. Though they aren’t regulated, they can be considered a form of air pollution. “When homes, schools, or businesses get water damage, mold can grow and produce allergenic airborne pollutants,” says Kim Knowlton, professor of environmental health sciences at Columbia University and a former NRDC scientist. “ Mold exposure can precipitate asthma attacks or an allergic response, and some molds can even produce toxins that would be dangerous for anyone to inhale.”
Pollen allergies are worsening because of climate change . “Lab and field studies are showing that pollen-producing plants—especially ragweed—grow larger and produce more pollen when you increase the amount of carbon dioxide that they grow in,” Knowlton says. “Climate change also extends the pollen production season, and some studies are beginning to suggest that ragweed pollen itself might be becoming a more potent allergen.” If so, more people will suffer runny noses, fevers, itchy eyes, and other symptoms. “And for people with allergies and asthma, pollen peaks can precipitate asthma attacks, which are far more serious and can be life-threatening.”
More than one in three U.S. residents—120 million people—live in counties with unhealthy levels of air pollution, according to the 2023 State of the Air report by the American Lung Association (ALA). Since the annual report was first published, in 2000, its findings have shown how the Clean Air Act has been able to reduce harmful emissions from transportation, power plants, and manufacturing.
Recent findings, however, reflect how climate change–fueled wildfires and extreme heat are adding to the challenges of protecting public health. The latest report—which focuses on ozone, year-round particle pollution, and short-term particle pollution—also finds that people of color are 61 percent more likely than white people to live in a county with a failing grade in at least one of those categories, and three times more likely to live in a county that fails in all three.
In rankings for each of the three pollution categories covered by the ALA report, California cities occupy the top three slots (i.e., were highest in pollution), despite progress that the Golden State has made in reducing air pollution emissions in the past half century. At the other end of the spectrum, these cities consistently rank among the country’s best for air quality: Burlington, Vermont; Honolulu; and Wilmington, North Carolina.
No one wants to live next door to an incinerator, oil refinery, port, toxic waste dump, or other polluting site. Yet millions of people around the world do, and this puts them at a much higher risk for respiratory disease, cardiovascular disease, neurological damage, cancer, and death. In the United States, people of color are 1.5 times more likely than whites to live in areas with poor air quality, according to the ALA.
Historically, racist zoning policies and discriminatory lending practices known as redlining have combined to keep polluting industries and car-choked highways away from white neighborhoods and have turned communities of color—especially low-income and working-class communities of color—into sacrifice zones, where residents are forced to breathe dirty air and suffer the many health problems associated with it. In addition to the increased health risks that come from living in such places, the polluted air can economically harm residents in the form of missed workdays and higher medical costs.
Environmental racism isn't limited to cities and industrial areas. Outdoor laborers, including the estimated three million migrant and seasonal farmworkers in the United States, are among the most vulnerable to air pollution—and they’re also among the least equipped, politically, to pressure employers and lawmakers to affirm their right to breathe clean air.
Recently, cumulative impact mapping , which uses data on environmental conditions and demographics, has been able to show how some communities are overburdened with layers of issues, like high levels of poverty, unemployment, and pollution. Tools like the Environmental Justice Screening Method and the EPA’s EJScreen provide evidence of what many environmental justice communities have been explaining for decades: that we need land use and public health reforms to ensure that vulnerable areas are not overburdened and that the people who need resources the most are receiving them.
In the United States, the Clean Air Act has been a crucial tool for reducing air pollution since its passage in 1970, although fossil fuel interests aided by industry-friendly lawmakers have frequently attempted to weaken its many protections. Ensuring that this bedrock environmental law remains intact and properly enforced will always be key to maintaining and improving our air quality.
But the best, most effective way to control air pollution is to speed up our transition to cleaner fuels and industrial processes. By switching over to renewable energy sources (such as wind and solar power), maximizing fuel efficiency in our vehicles, and replacing more and more of our gasoline-powered cars and trucks with electric versions, we'll be limiting air pollution at its source while also curbing the global warming that heightens so many of its worst health impacts.
And what about the economic costs of controlling air pollution? According to a report on the Clean Air Act commissioned by NRDC, the annual benefits of cleaner air are up to 32 times greater than the cost of clean air regulations. Those benefits include up to 370,000 avoided premature deaths, 189,000 fewer hospital admissions for cardiac and respiratory illnesses, and net economic benefits of up to $3.8 trillion for the U.S. economy every year.
“The less gasoline we burn, the better we’re doing to reduce air pollution and the harmful effects of climate change,” Walke explains. “Make good choices about transportation. When you can, ride a bike, walk, or take public transportation. For driving, choose a car that gets better miles per gallon of gas or buy an electric car .” You can also investigate your power provider options—you may be able to request that your electricity be supplied by wind or solar. Buying your food locally cuts down on the fossil fuels burned in trucking or flying food in from across the world. And most important: “Support leaders who push for clean air and water and responsible steps on climate change,” Walke says.
- “When you see in the news or hear on the weather report that pollution levels are high, it may be useful to limit the time when children go outside or you go for a jog,” Walke says. Generally, ozone levels tend to be lower in the morning.
- If you exercise outside, stay as far as you can from heavily trafficked roads. Then shower and wash your clothes to remove fine particles.
- The air may look clear, but that doesn’t mean it’s pollution free. Utilize tools like the EPA’s air pollution monitor, AirNow , to get the latest conditions. If the air quality is bad, stay inside with the windows closed.
- If you live or work in an area that’s prone to wildfires, stay away from the harmful smoke as much as you’re able. Consider keeping a small stock of masks to wear when conditions are poor. The most ideal masks for smoke particles will be labelled “NIOSH” (which stands for National Institute for Occupational Safety and Health) and have either “N95” or “P100” printed on it.
- If you’re using an air conditioner while outdoor pollution conditions are bad, use the recirculating setting to limit the amount of polluted air that gets inside.
This story was originally published on November 1, 2016, and has been updated with new information and links.
This NRDC.org story is available for online republication by news media outlets or nonprofits under these conditions: The writer(s) must be credited with a byline; you must note prominently that the story was originally published by NRDC.org and link to the original; the story cannot be edited (beyond simple things such as grammar); you can’t resell the story in any form or grant republishing rights to other outlets; you can’t republish our material wholesale or automatically—you need to select stories individually; you can’t republish the photos or graphics on our site without specific permission; you should drop us a note to let us know when you’ve used one of our stories.
Related Stories

When Customers and Investors Demand Corporate Sustainability

The Particulars of PM 2.5

What Are the Effects of Climate Change?
When you sign up, you’ll become a member of NRDC’s Activist Network. We will keep you informed with the latest alerts and progress reports.
- Name This field is for validation purposes and should be left unchanged.
- Climate Change
- Policy & Economics
- Biodiversity
- Conservation
Get focused newsletters especially designed to be concise and easy to digest
- ESSENTIAL BRIEFING 3 times weekly
- TOP STORY ROUNDUP Once a week
- MONTHLY OVERVIEW Once a month
- Enter your email *
- Email This field is for validation purposes and should be left unchanged.
New Research Brings Fresh Methodological Perspective on Air Pollution and Mental Health

Air pollution’s effects on physical health have been widely acknowledged, with countless studies linking poor air quality to respiratory and cardiovascular diseases. However, the relationship between air pollution and mental health has been less explored. A new study dives into this emerging field, offering fresh insights into how air pollution could impact our mental well-being.
Air pollution has long been known as a silent killer, responsible for millions of premature deaths each year. The effects of air pollution on physical health, particularly respiratory and cardiovascular health, are well-known. However, a new study emphasizes that the damage extends beyond the lungs and heart and extends to the mind. Researchers are beginning to uncover that exposure to particulate matter (PM) in the air could be linked to a host of mental health issues, including anxiety , depression , and stress .
The study’s authors set out to explore how researchers have historically studied this connection by seeking to find the most preferred methodologies. Their work provides a comprehensive overview of the methods used to investigate air pollution’s potential mental health effects, focusing on adults living in urban, suburban, and rural areas.
The study argues that better insights into how air quality affects mental health could lead to improved public health strategies and air quality management, ultimately enhancing well-being on a broader scale.
Mental health is increasingly recognised as a critical component of overall well-being . With mental health disorders becoming a leading cause of disability worldwide , understanding all potential risk factors – including environmental ones – has never been more critical.
How We Study the Air We Breathe
The study’s central aim was to review the methods used by researchers to link outdoor particulate matter (PM) with mental health outcomes. The authors scoured through literature published between 2010 and 2024, honing in on studies that analyzed the relationship between PM and symptoms of depression, anxiety, and stress in adults. Notably, the research excluded vulnerable populations such as children, the elderly, and pregnant women to focus more precisely on the general adult population to potentially introduce a standardized methodology approach that could apply to future research focusing on various cohorts.

Among the 3,889 papers analyzed initially, only 29 were taken into consideration, as they met the study’s stringent inclusion criteria, which included gathering studies on ambient air pollution and focusing on PM only. These studies covered various countries and employed a range of quantitative methodologies to assess air quality and its potential impacts on mental health.
One of the most intriguing findings of this scoping review is the geographic distribution of the studies. Most research has been conducted in Asia, particularly China, where air pollution, primarily caused by industrial activity, is a significant concern. The country has consequently increased airborne pollutants in places near Japan, South Korea, and Taiwan, as well as in places as far away as California in the US due to airborne pollutant travel. Europe also features prominently, while studies in North America and Australia are less common. A notable absence of South American and African studies highlights a critical gap in the global research landscape.
The finding of geographic concentration could be due to the severe air pollution in regions like China, where the effects on mental health might be more pronounced or easier to study. Although China has implemented strong air quality regulations and research , it still struggles with elevated air pollution levels and adhering to the World Health Organization’s recommended limit values for air pollutants. This calls for more research in underrepresented areas to understand how air pollution impacts mental health worldwide.
| Fine particulate matter, µg/m | Annual: 5 24-hour: 15 |
| Ozone, µg/m | 8-hour: 100 |
| Nitrogen dioxide, µg/m | Annual: 25 24-hour: 40 |
What We Know: Key Findings From the Reviewed Studies
Most studies reviewed showed a significant negative impact of air pollution on mental health. Specifically, higher levels of particulate matter were consistently associated with increased symptoms of depression, anxiety, and stress. Of the 29 studies, 27 found a clear link between poor air quality and mental health issues, demonstrating a solid consensus in the literature.
However, two studies did not find a significant correlation, suggesting that while the evidence is strong, it is inconclusive. The new study highlights the need for more research to confirm these findings and to explore the underlying mechanisms that could explain how air pollution affects the brain.
How Researchers Are Measuring Mental Health and Air Quality
The methodologies used to study the relationship between air pollution and mental health vary widely. Most of the reviewed studies relied on quantitative methods, using standardized psychological scales like the Patient Health Questionnaire (PHQ) to measure symptoms of depression and anxiety. Other studies relied on medical records to gather data on mental health outcomes, while a few employed innovative tools like portable air quality sensors to get real-time exposure data.
The review found that stationary air quality monitoring stations and land-use regression models were the most common methods for assessing air pollution levels. These tools provide robust data on long-term exposure to particulate matter, allowing researchers to make more accurate connections between air quality and mental health.
Gaps in the Current Research
Besides providing valuable insights, the review also highlights significant gaps in the existing research. Most notably, there is a lack of studies focusing on the general adult population, as much of the existing research has concentrated on vulnerable groups like children and the elderly. Additionally, there is a need for more longitudinal studies that track mental health outcomes over time, as most current research relies on cross-sectional data, which only provides a snapshot of the situation and the need for studies mainly focusing on qualitative or mixed-method approaches.
Qualitative research can offer a deeper understanding of health phenomena and a comprehensive picture, especially from an individual perspective . At the same time, a mixed-methods approach could enhance the accuracy and reliability of mental health evaluations.

The authors also call for more research to evaluate mental health outcomes concerning other pollutants. Other pollutants, such as nitrogen dioxide or volatile organic gasses, warrant consideration in future research. Their potential neurotoxic effects could contribute to a broader understanding of how air pollutants impact the nervous system and mental health. Moreover, studies were lacking in controlling potential confounders, such as meteorological effects , which could influence the observed associations between air pollution and mental health.
Underrepresented regions, particularly in South America and Africa, remain largely unexplored when it comes to the effects of air pollution on mental health. These regions face unique environmental challenges and socio-economic conditions that could influence the relationship between air pollution and mental health differently compared to more industrialized areas.
You might also like: Research Gap: The Geographical Bias of Environmental Data
Moving Forward: A Call to Action
The findings of this scoping review underscore the importance of expanding our understanding of how air pollution affects mental health. Future research should fill the gaps identified in this review , particularly by focusing on the general adult population and conducting more longitudinal studies.
Additionally, integrating qualitative approaches could provide more prosperous, nuanced insights into how individuals perceive and experience the mental health impacts of air pollution. By broadening the scope of research, we can develop more effective public health strategies that address the full range of air pollution’s impacts on well-being.
While evidence on the potential link between air pollution and mental health is growing, much remains to be understood. The authors of the review call for more comprehensive and geographically diverse research to fully uncover the extent of air pollution’s impact on mental well-being. As we continue to grapple with the challenges of air pollution, this research highlights the urgent need to consider the physical and psychological health implications of the air we breathe. By addressing these gaps, we can work towards a future in which cleaner air means healthier lungs and minds.
This story is funded by readers like you
Our non-profit newsroom provides climate coverage free of charge and advertising. Your one-off or monthly donations play a crucial role in supporting our operations, expanding our reach, and maintaining our editorial independence.
About EO | Mission Statement | Impact & Reach | Write for us
About the Author

Kristina Leontjevaite

Fast Fashion and Its Environmental Impact

10 Companies Called Out For Greenwashing

10 Concerning Fast Fashion Waste Statistics
Hand-picked stories weekly or monthly. We promise, no spam!
Boost this article By donating us $100, $50 or subscribe to Boosting $10/month – we can get this article and others in front of tens of thousands of specially targeted readers. This targeted Boosting – helps us to reach wider audiences – aiming to convince the unconvinced, to inform the uninformed, to enlighten the dogmatic.
Renowned expert on water-to-air pollution to speak at College of Science J. Mark Sowers Distinguished Lecture Series
23 Sep 2024
- Share on Facebook
- Share on Twitter
- Copy address link to clipboard
Kimberly Prather of UC San Diego's Scripps Institute of Oceanography is the latest speaker in the J. Mark Sowers Distinguished Lecture Series. Photo courtesy of Kimberly Prather.

The Virginia Tech College of Science’s J. Mark Sowers Distinguished Lecture Series will host a talk on Thursday, Sept. 26, by Kimberly Prather, a member of the National Academy of Sciences and distinguished professor at the University of California San Diego’s Scripps Institute of Oceanography.
Prather, of the Department of Chemistry and Biochemistry, has researched how water pollutants — previously believed to remain in the water — can turn into aerosols and affect air quality, climate, and health. Once airborne, Prather said, the pollutants can travel great distances and affect ecosystems over wide areas.
“With a large portion of the global population living near and contributing to polluted waterways, understanding these impacts is vital,” Prather said, “as increasing water pollution worldwide poses growing threats to public health and air quality.”
Prather’s lecture is titled:“From Water to Air: How Pollution Impacts Air Quality and Health in Coastal Regions.” Her talk will be 7:30 p.m. in Assembly Hall at Holtzman Alumni Center. The lecture is free and open to the public.
Prather’s talk that evening will cap a day of discussion on the Blacksburg campus about the health of the coastal environment. During the day, the Seale Coastal Zone Observatory will conduct a symposium and workshop on Coastal Studies: Environmental Microplastics Fate and Effects. Prather and Michael F. Hochella Jr., University Distinguished Professor Emeritus at Virginia Tech, will deliver the keynote addresses.
Prather’s Sowers talk will highlight key findings from over a decade of research by the National Science Foundation's Center for Aerosol Impacts on Chemistry of the Environment, which developed an “ocean-in-the-lab” approach to study how pollutants are released into the atmosphere. This led to the Scripps Ocean-Atmosphere Research Simulator, a facility that simulates waves, winds, temperature, and biological activity to examine sea spray production and gas transfer processes at the air-sea interface.
Building on these lab studies, current research examines how pollution from the Tijuana River and the coastal ocean influences air quality and health. Flowing across the U.S.-Mexico border into the Pacific Ocean near southern San Diego, the Tijuana River serves as a critical case study for understanding how pollutants transfer from water to air, affecting coastal communities and underscoring environmental justice concerns.
The J. Mark Sowers Distinguished Lecture Series in the College of Science at Virginia Tech is a forum for the exchange of new and innovative ideas in scientific fields. The series began in February 2017.
It has attracted national and world-renowned scholars, including a laser physicist, a nanoscientist, an astrophysicist, an applied mathematician, the director of the NASA Astrobiology Institute, and a statistician who specializes in machine learning. Discussions have delved into brain sciences, speech and hearing development, black holes, and more. Generously supported by Mark and Debi Sowers, this series provides opportunities for the university community and general public to interact with and learn from eminent scholars and industry experts.
Sowers is a Richmond-based businessman and developer and longtime supporter of the College of Science . He sponsors the series to share with others his fascination with the sciences.
540-231-6468
- Air Pollution
- Biochemistry
- Climate Change
- Coastal Research
- College of Science
- Environmental Health and Safety
- Philanthropy
Related Content

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- eBioMedicine
- v.93; 2023 Jul
- PMC10363432

Gaps and future directions in research on health effects of air pollution
Ruzmyn vilcassim.
a Department of Environmental Health Sciences, The University of Alabama at Birmingham, School of Public Health, USA
George D. Thurston
b Departments of Medicine and Population Health, New York University School of Medicine, USA
Despite progress in many countries, air pollution, and especially fine particulate matter air pollution (PM 2.5 ) remains a global health threat: over 6 million premature cardiovascular and respiratory deaths/yr. have been attributed to household and outdoor air pollution. In this viewpoint, we identify present gaps in air pollution monitoring and regulation, and how they could be strengthened in future mitigation policies to more optimally reduce health impacts. We conclude that there is a need to move beyond simply regulating PM 2.5 particulate matter mass concentrations at central site stations. A greater emphasis is needed on: new portable and affordable technologies to measure personal exposures to particle mass; the consideration of a submicron (PM 1 ) mass air quality standard; and further evaluations of effects by particle composition and source. We emphasize the need to enable further studies on exposure–health relationships in underserved populations that are disproportionately impacted by air pollution, but not sufficiently represented in current studies.
Introduction
Since the early establishment of air quality regulations in the United Kingdom in 1956 and the 1970 Clean Air Act in the United States, followed by similar governmental legislations across Europe and the rest of the world, air pollution levels have decreased considerably in most major cities in high-income countries that used to be primary hubs of industrialization and poor air quality not so long ago. Six ‘Criteria’ or ‘classical’ air pollutants were targeted by the United States Environmental Protection Agency (US EPA) and the World Health Organization (WHO): Ground-level ozone (O 3 ), particulate matter (PM), carbon monoxide (CO), lead, sulfur dioxide (SO 2 ) and nitrogen dioxide (NO 2 ). Standards and guidelines were imposed for each pollutant 1 , 2 initiating mitigatory measures. However, controlling air pollution has been more challenging globally, and levels of air pollutants have worsened in most large cities in low and low-middle income countries, 3 at times leading to historic air pollution episodes in cities such as New Delhi, Beijing, and Karachi. 4 , 5 In addition, as levels have declined in high income countries, new evidence has documented severe adverse health effects still occur even at their now lowered exposure levels. 6 , 7 Concentrations previously considered ‘healthy’ may now exceed the newer more stringent guidelines by the WHO, and frequent short-term excursions are observed even in usually ‘low-pollution’ cities. Thus, air pollution remains a major global environmental concern impacting human health, particularly among vulnerable groups and socioeconomically disadvantaged communities. 8 , 9 The Lancet Commission's 2019 report and the WHO have estimated that some 6.7 million premature deaths can be attributed to the combined impact of household and outdoor air pollution, primarily from increased mortality from cardiovascular and respiratory diseases. 10
Over the past half century, exposure scientists, epidemiologists, and researchers of various related disciplines have made significant contributions in developing methods for monitoring and controlling airborne pollutants and investigating the harmful effects of exposure to air pollution. However, the chemistry of air pollutants, their behavior in the atmosphere/environment, and their interactions with biological systems are complex and, despite major strides in research, many unknowns persist. In 2010, an international specialty conference sponsored by the American Association for Aerosol Research (AAAR) titled “ Air Pollution and Health: Bridging the Gap from Sources to Health Outcomes ” 11 identified key needs to improve our understanding of air pollution related adverse effects: 1) a greater focus on multipollutant science that includes studies on mixtures and pollutant sources, 2) a better understanding of biological mechanism and associations of various health effects with sub-components of PM (e.g., submicron particles, elemental carbon, trace elements, and source-specific mixtures); 3) a further understanding of susceptibility of populations - including the role of genetics/epigenetics, the influence of socioeconomic and other confounding factors, and; 4) the addition of new technologies, such as ‘microsensors’, hybrid air quality modeling, and remote (e.g., satellite) sensing data. 11 While there have been significant improvements in addressing some of these concerns, many gaps identified at that time still persist.
Of the various air pollutants, greater importance has been attributed to the mass concentration of particulate matter (particularly PM with aerodynamic diameters smaller than 10 μm and 2.5 μm; PM 10 and PM 2.5 ), due to studies showing stronger links between fine PM concentration and adverse health effects. 12 While, even to-date, the mass concentration of PM is used as the standard and main exposure metric in many studies, the AAAR conference attendees raised concerns that mass concentration alone does not appear to be a metric sufficient to fully and effectively evaluate the health effects of PM exposure: the size, source, and composition of PM and other physical properties also need to be considered in evaluating health effects. More recently, Nicolaou and Chekley (2021) 13 discussed deficiencies in air quality monitoring including, research on the long-term effects of exposure, lack of knowledge in relative toxicities from different sources and the joint and independent effects of multipollutant exposures, the impacts of ultrafine particulate matter, and importantly, the need for more effort in research in low-and-middle-income countries (LMICs), where exposures are highest, but data are sparse. In addition, attention has been drawn to gaps in our understanding of air pollution control and health, particularly on diseases spread by airborne pathogens. 14 Thus, most knowledge gaps discussed in the past still persist, although insights into some have advanced significantly in recent years, such as studies on epigenetic factors associated with air pollution exposure, 15 , 16 as well as analyses of source mixtures and metals more strongly associated with health outcomes. 17 , 18 In addition, improved understanding of the biological mechanisms regarding how air pollutants affect various organ systems, including cardiovascular, neurological, developmental, and metabolic systems, provide vital insights for other aspects of research including identifying susceptibility and possible treatments. For example, recent research has pointed to oxidative stress from fine PM containing both transition metals and acidic sulfates, such as emitted by fossil fuel combustion, as a likely important health impact causal pathway. 19
Therefore, despite a long history of air pollution research, there is still much to learn about the interactions between air pollutants and human health systems, and the external modifying factors influencing this relationship. New challenges have emerged, in addition to the pre-existing issues and gaps in knowledge. In this viewpoint, we identify critical gaps in air pollution research/knowledge, and discuss future directions and their potential impact on air pollution related health risks along the following key themes: (1) Air pollution monitoring methods and technological limitations e.g. air pollution source and composition, number concentration vs. mass concentration, central vs. personal monitoring; (2) Exposure assessment uncertainties impacting health outcomes assessed and, (3) Regulatory standards and policies.
Gaps in monitoring methods and technological limitations
Pm mass, size, composition, and source.
While the U.S. EPA recognized the key role of fine particulate matter in the health effects of particles when it changed the U.S. ambient air quality standard from PM 10 to PM 2.5 in 1997, 20 further progress has been lagging in its regulation to better monitor and focus regulation on those fine particles that are most toxic, which varies within PM 2.5 depending on size, composition, and source. The growing evidence that the most toxic particles are among the sub-micron size (e.g., nanoparticles), and from sources emitting the most toxic mix of constituents (e.g. fossil fuel combustion), is yet to be addressed in regulations, or in most PM air pollution studies. 21 While some have called for the conduct of site-specific epidemiological studies of PM 2.5 health effects in every locality to address the variation in PM 2.5 toxicity per unit mass 22 , the development and application of source sector-specific and composition-specific health effect estimates (e.g., for those with the highest risk per μg/m 3 ) would more efficiently allow the derivation of more locally appropriate site-specific health effect coefficients, based on local measurements of PM 2.5 source and composition, sidestepping the need for multiple epidemiological studies in each locality. Thus, better quantifying source and composition-based air pollution associated health impacts needs to begin with more detailed particulate matter monitoring when evaluating air pollution levels over space and time.
In most countries and cities, air pollution concentrations are obtained via central fixed reference-grade ambient monitors. In the U.S., the EPA has established a large network of central ambient monitors, mainly to measure and meet federal regulatory NAAQ standards, which are based on either hourly, daily and/or annual averages of overall mass concentration. In addition, the U.S. EPA has established a more limited Chemical Speciation Network (CSN) that are useful in evaluating variations in PM 2.5 composition, as well as useful for the estimation of source-specific exposure levels at those sites and at intervening locales using land use regression methods (e.g., see Rahman and Thurston, 2021). 23 Such data have proved useful in discriminating the varying health effects of different PM 2.5 components, but more such composition-based analyses of PM 2.5 samples and their health effects at more sites around the world are needed to enable more location-specific health effects estimation, enabling more health benefit optimized PM 2.5 mitigation policies. The expansion and maintenance of a worldwide CSN will be financially and technically challenging, added by the complexity of chemical compositions of various PM components. However, the data generated from such methods are key to connect epidemiologic findings with toxicological findings, as demonstrated in the NPACT study in the USA. 18 , 24 The studies conducted under the NPACT initiative were key in identifying source components of PM which have greater potential to cause harm, as well as to identify the challenges and complexities that need to be addressed to understand the mechanisms of individual component toxicities.
Since particulate matter derived from sources most often associated with the adverse health effects of PM 2.5 (e.g., fossil fuel combustion particles) are found in the sub-micron part of PM 2.5 mass, we also recommend another, simpler, approach to focus mitigation on the most toxic particle sources: switch from monitoring and regulating PM 2.5 to PM 1 (particles less than 1 μm in aerodynamic diameter) mass. This is consistent with the past progression in particle mass regulation from Total Suspended Particulate Matter (TSP), to inhalable particulate matter (PM 10 ) to fine particulate matter (PM 2.5 ). While this concept has been in discussion among air pollution scientists in recent years, perhaps the main challenge for implementation of a PM 1 standard was the lack of evidence of associated health benefits in the past. PM 1 is not monitored in the U.S. and many other major cities, limiting the number of studies that investigate associations between PM 1 levels and health outcomes. However, in recent years there has been a growing body of epidemiology results finding stronger health associations with PM 1 mass than with PM 2.5 . For example, Yang et al. (2020) recently found that “Associations with lower lung function were consistently larger for PM 1 than for PM 2.5 . 25 Guo and colleagues (2022) evaluated the varying associations of the incidence rate of female lung cancer with PM 1 , PM 2.5 , and PM 10 in 436 Chinese cancer registries and demonstrated that the association with the incidence rate of female lung cancer was stronger for PM 1 than for PM 2.5 or PM 10 . 26 Similarly Hu et al. concluded that their mortality studies found greater PM 1 effects per μg/m 3 , and that “To effectively reduce the adverse health effects of PMs, more attention should be paid to fine and very fine particles”. 27 Clearly, further air pollution monitoring of PM 1 , and epidemiological studies comparing PM 2.5 vs. PM 1 associations with adverse health are needed in order to confirm the case for PM 1 based air pollution control and regulations.
Monitoring of personal exposures
While central monitors provide a very useful estimate of a region's typical pollution levels, they are of limited use in providing estimates of personal-level exposures.
- • First, the number of residents represented by a central monitor can vary significantly within a country and between countries. In Europe and North America, the estimates are about one monitor per 100,000–600,000 residents, while in contrast, across sub-Saharan Africa one ground-level monitor represents about 15.9 million residents. 28 , 29 , 30
- • Second, central site monitors do not represent concentrations in varying microenvironments and occupational settings, which may be higher. For example, it has been found that street level NO 2 exposures in a city can be significantly higher than measured at a regulation air monitoring site located just a few stories above. 31
- • Third, when the interest is to study the health effects of smaller targeted populations, including vulnerable communities that may live in areas that do not have central monitors, they provide little information on personal exposure levels in populations that may be more strongly linked to health outcomes.
However, it is important to note that, despite these limitations of stationary monitoring, consistent associations have still been found in epidemiological studies over large populations using central monitoring data in different geographical regions. More focused exposures are needed to consider more sensitive subpopulations.
Advanced modeling of higher spatial resolution exposures using central monitor data as inputs have provided more spatially detailed estimates, such as via Land Use Regression (LUR) models, and satellite estimates of surface PM concentrations. 23 , 32 However, LUR and air quality models require extensive monitoring, meteorological data, and built environment information, 33 , 34 , and may not be broadly applicable to other locations. Similarly, satellite estimates of PM, while more spatially comprehensive, may have errors in the range of 22–85% if they are not cross-validated by ground level monitoring data, and are also impacted by other atmospheric conditions and particles in the atmosphere. 28 Due to such limitations, accurately estimating air pollution exposures for epidemiological studies still remains a challenge, contributing to variations in the estimations of health effects per amount of exposure, particularly in LMICs and rural areas in high-income countries, where central monitor coverage is more sparse.
This brings us to a more accurate approach for the estimation of individual level exposures to air pollutants-personal monitoring. Personal monitor sampling at breathing level provides the most accurate time-integrated exposures and variations of an individual's exposure. 35 For example, van Nunen et al. (2021) successfully employed 24-h personal monitoring of PM 2.5 , ultrafine particles, and soot concentrations to study their associations with blood pressure and lung function changes. 36 Xie et al. (2021) simultaneously obtained PM measurements from personal monitors and regulatory monitors to study exposures in individuals with asthma, and demonstrated that the portable monitors were better able to capture personalized air quality information compared to the traditional method. 37 However, despite these advantages, the wide use of personal monitors for exposure studies is limited for several reasons. Personal monitors and methods that have been validated and are of research grade have been expensive and require initial training to use, particularly for monitoring of gases and volatile organic compounds (VOCs). Examples for PM personal monitoring methods and devices include gravimetric analysis using portable pumps and filters, as well as light scattering-based nephelometric devices, which can cost in the range of $7000 - $8000 per unit. Therefore, monitoring exposure concentrations of a group/population has been limited by the number and cost of research-grade personal monitors available. Thus, although personal monitoring can provide more accurate estimates of individual and sensitive subpopulation exposures, these limitations have prevented them from significantly advancing the field of air pollution and health studies, as compared to the contribution from studies that have used central-site monitoring data.
In recent years, however, the goal of higher spatial and time resolution individual level air pollution monitoring has been made more attainable by the introduction and rapid advancement of low-cost sensors . Low-cost sensors (LCS) are expected to be an important development in the future direction of more democratized, high resolution, and inter-connected air (and health) monitoring, generating ‘big data’ for complex, but more inclusive, research. In addition to being inexpensive, mobile, and light weight, currently available LCS are smartphone compatible, which has greatly increased their appeal among concerned citizens and environmental non-profits, allowing monitoring among those who could not previously afford the traditionally more expensive personal monitoring equipment. LCS are also typically linked via GPS, and are used for crowdsourcing and identifying air pollution ‘hotspots’ in cities. 38 Recognizing this, the U.S. EPA has developed a comprehensive program to test and validate currently available low-cost air monitoring devices against reference grade and/or more advanced instruments, which is a major step in testing their capabilities for research. 39 , 40 A significant body of research has now been done to test and use LCS for personal exposure monitoring, demonstrating their potential for use in research, with proper quality control. 38 , 39 , 41 , 42 Importantly, their advantages make low-cost sensors a strong candidate for studies in LMIC, where resources for environmental monitoring are more scarce.
Despite the numerous advantages of low-cost air monitoring sensors, their accuracy may be limited as measurements can be biased by variations in the ambient environment, inter-instrument variability, limitations in the range of concentrations that can be measured, and concentration plateauing due to signal saturation above certain levels - typically above 100 μg/m 3 . 41 , 43 They have also been found to underperform in lower pollution settings, demonstrating poor agreement with more advance instruments below 40 μg/m 3 . 44 Therefore, they are most accurate and have high agreement with reference instruments only within a particular range. 42 , 43 Sensor ‘aging’ drift is also a concern. 41 In very high concentration situation LCS may also become saturated, and fail to accurately assess extreme concentrations. Therefore, scientists and the U.S. EPA have recommended periodic calibration of low-cost devices with more advanced or reference instruments to achieve data quality and accuracy. 39 , 43 , 45 , 46 In addition, prior to use in studies, they require continuous development and evaluation of calibration protocols and algorithms, which, if not done, can lead to uncertainties in obtaining reliable and timely air quality data. 42 Indeed, monitoring data quality has been found to improve LCS performance significantly after calibration. 46 Another challenge in LCSs is the lack of a physical size ‘cut-point’ that are designed into advanced instruments. Sensors estimate particle size using an internal algorithm, which at times have been found to be different from reference instruments. 41 However, overall, LCS present a great potential to be a powerful tool for augmenting central site air quality monitoring data with higher resolution, particularly for research in communities in LMIC and other areas that are unable to afford central site reference monitors.
Other developments in methods and technologies for personal monitoring that have seen progress in recent years and have future potential include, low-cost wearable sensors to measure health biometrics, 47 , 48 and non-invasive health biomarker analysis methods, such as breath biopsies. 49 , 50 These methods, combined with low-cost air monitoring devices, could be used to generate high resolution exposure-health metrics for scientists and medical professionals in studying and mitigating the health impacts of air pollution.
Exposure assessment uncertainties and exposure misclassification due to movement between environments with varying conditions
Advancements in monitoring instrument technologies, statistical and modeling methods, and high-resolution geographical mapping have improved our ability to better estimate exposure concentrations of populations in regions of interest, such as in communities living close to a powerplant, or children exposed to vehicle emissions when they live near highways. Recent research indicates that epidemiological effect estimates of PM 2.5 health effects are robust to the choice of PM 2.5 exposure assessment spatial resolution. 51 , 52 , 53 However, individuals move between ‘microenvironments’ with varying sources and concentrations, and failing to incorporate these variations may still lead to exposure misclassification and/or exposure estimation errors. Exposure estimation errors may be exacerbated among those living outside an urban core, or when time is spent in microenvironments with higher than average air pollution within the urban core. 54 More epidemiological studies that incorporate study participant mobility into exposure assessments are needed, which may now be more practical, given the improvements and cost reductions in personal particulate matter monitoring equipment, and the common availability of cell phones for data storage and transmission.
We particularly note two venues of air pollution related health exposures that impact a large number of individuals, but have lacked sufficient attention and need further exposure - health effects investigations. They are: (a) when traveling to polluted cities abroad (particularly international travel) and, (b) when using major transit systems, especially in underground subway systems.
Air pollution health risks when travelling
Until the coronavirus disease (COVID-19) pandemic, international tourist arrivals had been steadily increasing with approximately 1.4 billion worldwide arrivals in 2019. 55 , 56 After a significant drop in 2020 and 2021, recent estimates show an increasing trend, and international tourism climbed to nearly 60% of pre-pandemic levels in January–July 2022. 56 During travel, a large population of individuals may be exposed to air pollution concentrations and compositions that significantly vary from their home city/country, especially when they travel to popular destinations in Asia, Africa and South America. Megacities in these regions have poor air quality which are known to exceed local and WHO guidelines by several levels of magnitude. 4 , 5 , 57 However, although billions of individuals travel internationally, there is very limited research addressing the impact of air pollution on travelers’ health. 58
Travelers may experience a large differential in ambient exposure concentrations and composition within a short time of air travel, increasing their risk of air pollution related injury compared to residents who are more likely to be adapted to local conditions and knowledge. Although limited in number, existing studies have indicated that exposure to elevated levels of PM 2.5 in cities abroad can be associated with adverse cardiopulmonary health impacts, including a reduction in lung function, increase in respiratory symptoms and, and impacting quality of life. 58 , 59 , 60 Importantly, most study participants recovered from symptoms after returning to home cities. Other studies provide evidence of systemic pro-oxidative and proinflammatory effects associated with travel-related exposure to air pollution, where the elevated levels of biomarkers were interestingly reversed after the participants returned to their home city. 61 In this study, exposure to Polycyclic Aromatic Hydrocarbons (PAHs) in cities traveled to altered oxidative metabolism, which can be attributable to ambient air pollution exposure.
In addition to air pollutant exposure related health risks, travelers may be unpredictably impacted significantly by climate-related events, which are expected to particularly affect vulnerable urban areas in South Asia, East Asia and the Pacific. 62 Rising global temperatures can increase the frequency of ‘extreme events’ such as floods, heatwaves, dust storms and wildfires, and increases in air or water pollution, thereby elevating health risks, and causing population displacement in affected regions. Thus, global warming is expected to contribute to human mobility, leading to increased migration and travel to regions that are perceived to be ‘safer’. 63 While studies on migrant health are emerging, there is a need for more studies linking previous and ‘new’ exposures of migrant populations to cardiovascular and respiratory health outcomes. 58 , 63
Despite these concerns faced by travelers and migrants, insufficient studies have further explored short and long-term health outcomes associated with visiting or temporarily migrating to polluted cities for work, safety, education, leisure etc., especially among vulnerable groups such as older, pregnant, and other susceptible travelers. 58 Adding to the difficulty of conducting such studies is the need to adjust for many confounders, such as stress, temperature changes, changes in diet and water intake, alterations in sleep and sleep patterns, effects of changing altitude, and infectious/transmissible diseases. Studies on physiological outcomes and biomarkers that can detect early cardiovascular effects due to air pollution exposure during international travel will be important to warn elderly and susceptible travelers of risks of traveling to polluted destination cities, prior to travel. Given that cities are increasingly connected via travel, their residents and visitors present dynamic interdependent systems in concert with variable air pollution profiles. Therefore, we suggest that future epidemiological studies that explore ambient PM associated all-cause, cardiovascular, and respiratory mortality not consider populations in individual cities as a static entity, but also strive to consider travel related exposures as a potentially significant component of disease risk when evaluating such outcomes. 64
Air pollution health risks in subways
Underground subway/metro systems move large numbers of people daily, and further growth in such systems are expected. 65 , 66 Although commuters spend a relatively shorter time on subway platforms, daily exposures to peak levels may significantly impact health. However, despite several studies documenting very high levels of PM exposure in underground systems, especially in North America, Europe, 65 , 67 , 68 , 69 , 70 we are unaware of studies that have yet comprehensively evaluated the health risks of inhalation of high levels of varying compositions in this unique environment. Subway PM 2.5 levels have shown to be elevated several fold over ambient levels even in busy cities, and contain higher proportions of iron and other metals, such as manganese and chromium. 65 , 68 High elemental carbon levels have also been reported in subways that utilize diesel-powered maintenance trains. 70 Except for some studies indicating that exposure to subway particles causes inflammation in lung epithelial cells and oxidative stress in exposed workers, 71 , 72 the health implications of repeated relatively brief, but very high, pollution exposure levels in subways are largely unknown. Further complicating the issue is the ambiguity of classifying the subway environment for regulatory purposes. Should outdoor ambient standards apply, and if so who has the authority to regulate pollution levels in subways? Or is it considered an ‘indoor’ environment? These legal questions remain unanswered, limiting our ability to evaluate the possible mitigatory options. Pollution mitigation approaches, such as improved ventilation in subway platforms and cars, and the use of electric/battery powered maintenance equipment for system maintenance, are suggested, and may also reduce virus transmission risks at the same time. 73 , 74 Further research on subway air quality is needed, especially as a large population of commuters around the world is expected to increasingly rely on these systems in the future.
Regulatory standards and policies impacting health
The establishment of ambient air quality standards around the world, particularly in North America and Europe, has greatly improved air quality in many regions compared to levels before they were established, and prompted improvements in air monitoring, technological advancements in emissions control technology, and more environmental friendly practices in industry. 75 , 76 , 77 In the U.S., these gains in air quality reduction benefits were made even as the economy has grown. 77 Legislation in Europe led to the rapid growth in monitoring stations, and progress was made towards improving air quality over time, despite some challenges such as rising O 3 levels in many European cities 76 In recent years, cities such as Beijing, which had extremely poor air quality in the past, has achieved sizable and steady declines in ambient air pollution levels due to stricter control measures on emissions, and particularly on coal burning. 78 Such significant reductions in PM 2.5 and PM 10 concentrations in 74 key cities in China (between 2013 and 2016) were shown to be associated with substantial reductions in mortality and years of life lost. 79 Thus, air quality regulations and action plans have overall reduced air pollutant levels and improved the lives of affected populations. However, there is still much to do on improving standards and policies, particularly considering the emerging knowledge on the complexity of particulate air pollutants and recent studies demonstrating inequalities in air pollution exposure and health disparities among historically disadvantaged and vulnerable (due to economic and environmental disasters) populations.
Recent research indicates that there is no known threshold of PM and other pollutants’ health effects (e.g., see US EPA, 2019 80 ), while reductions will likely become more challenging to implement as regulatory PM 2.5 mass concentration limits decrease. As a result, the focus on mass without consideration of variations in composition toxicity has the potential drawback that the fine mass constituents that contribute the most mass may become the focus of controls, even if they are not the most toxic constituents. For example, some have recently recommended focusing on controlling gaseous ammonia releases in order to lower PM 2.5 because it reacts with ambient sulfuric and nitric acid to form particulate matter, 81 but that step would lead to more acidic (less neutralized), and likely much more toxic, particulate matter that remains in the air, likely leading to increased toxicity per unit mass. 82 Therefore, it would likely be more health efficient to consider focus additional PM regulation on the most toxic constituents of PM 2.5 , or on the submicron subcomponent, of the mass PM 1 . As discussed above, this concept has been in discussion for many years, 83 but now may well be the time for its implementation.
The issue of varying PM 2.5 composition and toxicity also has implications to standard and Air Quality Index (AQI) interpretation. In contrast to the setting of a single AQI for individual gaseous pollutants, such as ozone, which is the same compound everywhere, the setting of a single world-wide AQI for particulate matter is less defensible, because PM 2.5 varies widely in its size distribution, composition, and dominant source, and likely in its toxicity to humans per μg/m 3 , from place to place. Thus, the above discussed need for the assessment of PM 2.5 exposures and health impacts as a function of size, composition, and source is directly relevant. Such studies would be useful for the setting of locality-specific PM 2.5 AQI values, For example, a recent study of pollution in Dhaka, Bangladesh found that the hospital admissions and mortality impacts of fossil-fuel combustion PM 2.5 has a much larger impact per unit mass than biomass related PM 2.5 in Dhaka. 84 Since biomass burning dominates the PM 2.5 mass in Dhaka, it may be that the overall health impacts of PM 2.5 are less per μg/m 3 than in the developed world cities where the WHO guideline studies were primarily conducted, and so it may well be that a higher AQI guideline would be appropriate in Bangladesh than in the US or Europe. Similarly, windblown sand is a large component of the PM 2.5 in the Middle East, unlike where PM 2.5 epidemiological studies have been conducted. Thus, it stands to reason that PM 2.5 AQI adjustments need to be made, depending on the region and particularly the primary sources of air pollution in that state or nation.
Environmental justice considerations make clear that the environmental health protection improvements suggested here for regulations and policies must most pressingly be applied to address those most affected by air pollution. Growing evidence has established that the burden of air pollution is not equally shared, and socioeconomically disadvantaged populations and certain racial and ethnic groups often face higher exposure to pollutants and greater responses from air pollution. 8 , 85 , 86 , 87 Thus, future research, education and air pollution control policies should consider their impact on groups most affected, and make an effort to mitigate inequities during the planning and implementation stages. For example, Wang Y et al. (2022) have shown that national inequalities in air pollution exposure can be eliminated with fewer emission reductions if those reductions target the most heavily burdened locations, rather than implementing across the board national standards ( Fig. 1 ). 88

PM 2.5 exposure-disparity and concentration-reduction curves . Each panel compares three approaches to emission reduction: location (green line), sector (blue line), and NAAQS-like (i.e., employing a concentration standard; here, 6 μg/m 3 ; orange line). An “equal reduction” approach, where all emissions are reduced proportionately, would be a straight line (black dotted line). The location approach (green line) can eliminate national disparities with modest total emission reductions. Fig. 1 was obtained from 88 with permission from the corresponding author.
The exposome and precision environmental health in air pollution research
Recent scientific discussions on the future of the field of environmental health have highlighted the importance of integrating knowledge from various related disciplines. Focus has been drawn to utilizing ‘exposomics’ which is based on the concept of the ‘exposome’-the totality of all exposures in an individual's life course. 89 Although the exposome is not a new concept, the realization that average exposures alone cannot explain disease spread or occurrence has highlighted the importance of considering the variations and complexities of the pollutants, and their interactions with individual and population characteristics over space and time. Thus, the concept is gaining increasing applications in environmental health and toxicology studies. Early prediction and avoidance of diseases has gained greater importance, combined with a push towards more precise individualized treatments for exposure associated diseases. 90
Precision environmental health, predictive and translational toxicology, social justice, and health disparities have been identified as key areas for future development of environmental health, as well as climate change and innovative computational methods for data analysis. For example, an expert panel from the National Academies sponsored by the National Institutes of Environmental Health Sciences (NIEHS) has identified areas that the biomedical community can use to integrate environmental health science into broader studies of human health. 91 Such integration of exposure data, ‘omics’ data, and personal health information will greatly improve our ability to predict air pollution related diseases (i.e. using predictively toxicology approaches) and implement more targeted early prevention strategies. However, for precision medicine to be effectively integrated with exposomics and to be utilized for predicting and preventing air pollution related diseases, the focus has to be expanded from genetic or molecular studies alone to also incorporate environmental factors that determine disease progression. Despite the available technologies, researchers have expressed concern that environmental or exposure related issues are rarely considered in current precision medicine programs. 90 Nevertheless, there is huge potential in integrating exposomics and precision medicine methods in future environmental health research, especially when combined with personal wearable monitors, advanced analytical methods, and modern artificial intelligence capabilities.
While acknowledging that the field of air pollution and associated health effects is robust and ever growing, and that scientists throughout the years have greatly contributed to the understanding and betterment of the science, we have identified key gaps and future directions especially needing attention in current and future studies and policies (as summarized in Table 1 ). Future directions will be influenced by technological developments and more advanced methods of particulate matter air quality measurement, modeling, analysis, and regulation, such as focusing future additional regulation on the most health threatening particles, such as PM 1 . On the other hand, other air pollutants, such as volatile organic compounds, nanoparticles, emissions from new technologies and industrial processes, emissions from e-waste disposal and burning also need attention and further investigation as to how more efficiently to mitigate their risks. Occupational exposures, medical exposures, and immune responses to ‘new’ and more toxic pollutants are other areas of research (among many others) that would also warrant attention and new methodologies for assessment.
Table 1
Summary of gaps and future directions in air pollution research and mitigation.
| Gaps/limitations identified | Current status | Suggestions/future directions |
|---|---|---|
| mass concentration determines standards. | ||
HICs, High-Income Countries; LMICs, Low- and Middle-Income Countries; PM, particulate matter; AQIs, Air Quality Indices.
Thus, the present and future of environmental health and air pollution research present many challenges, such as changing pollution source mixes and characteristics over space and time, but also new opportunities, as technology opens new exposure measurement possibilities. Strong international cooperation is needed between countries/communities with resources and those that do not, for more extensive and advanced exposure data collection and dissemination, research knowledge, and resource sharing, so that these new methods and technologies become accessible in LMICs and burdened communities, as well. In this way, there is the potential to achieve a world in which scientific collaborations, using more globally accessible methods-such as remote and low-cost sensors, open source data platforms, and capacity building programs, can greatly influence and mitigate air pollution related health risks, enabling better informed, fair, and more equitable environmental health solutions for all.
Contributors
Both authors (RV and GDT) contributed to the conceptualization, preparation of the original draft, and editing of the manuscript. Both authors read and approved the final version of this manuscript.
Data sharing statement
Not applicable.
Declaration of interests
The authors declare no completing interests.
Acknowledgements
This work was not funded by any specific funding agency. RV is partially supported by a JPB Environmental Health Fellowship award granted by The JPB Foundation and administered through the Harvard T.H. Chan School of Public Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of any funding agency.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 25 September 2024
Soil and water pollution and cardiovascular disease
- Thomas Münzel ORCID: orcid.org/0000-0001-5503-4150 1 , 2 ,
- Omar Hahad ORCID: orcid.org/0000-0001-7823-7671 1 , 2 ,
- Jos Lelieveld 3 ,
- Michael Aschner ORCID: orcid.org/0000-0002-2619-1656 4 ,
- Mark J. Nieuwenhuijsen 5 ,
- Philip J. Landrigan 6 , 7 &
- Andreas Daiber ORCID: orcid.org/0000-0002-2769-0094 1 , 2
Nature Reviews Cardiology ( 2024 ) Cite this article
91 Accesses
51 Altmetric
Metrics details
- Cardiovascular diseases
- Chemical biology
Healthy, uncontaminated soils and clean water support all life on Earth and are essential for human health. Chemical pollution of soil, water, air and food is a major environmental threat, leading to an estimated 9 million premature deaths worldwide. The Global Burden of Disease study estimated that pollution was responsible for 5.5 million deaths related to cardiovascular disease (CVD) in 2019. Robust evidence has linked multiple pollutants, including heavy metals, pesticides, dioxins and toxic synthetic chemicals, with increased risk of CVD, and some reports suggest an association between microplastic and nanoplastic particles and CVD. Pollutants in soil diminish its capacity to produce food, leading to crop impurities, malnutrition and disease, and they can seep into rivers, worsening water pollution. Deforestation, wildfires and climate change exacerbate pollution by triggering soil erosion and releasing sequestered pollutants into the air and water. Despite their varied chemical makeup, pollutants induce CVD through common pathophysiological mechanisms involving oxidative stress and inflammation. In this Review, we provide an overview of the relationship between soil and water pollution and human health and pathology, and discuss the prevalence of soil and water pollutants and how they contribute to adverse health effects, focusing on CVD.
Illnesses related to chemical pollution of the soil, water and air are responsible for an estimated 9 million premature deaths annually, which equates to 16% of all global deaths; half of these deaths are of cardiovascular origin.
Degradation of the soil threatens the health of at least 3.2 billion people (40% of the global population), whereas >2 billion people live in water-stressed countries (25% of the global population).
Eco-disruptive causes of soil and water pollution include deforestation, climate change, airborne dust, over-fertilization and unhealthy city designs.
Pollution by heavy metals, pesticides, and microplastics and nanoplastics causes cardiovascular damage by interacting with protein-bound thiols, inducing oxidative stress and inflammation, and impairing circadian rhythms.
Exposure to chemicals (such as heavy metals, solvents, dioxins and pesticides) at workplaces, through consumer products or indirectly via environmental contamination contributes to endothelial dysfunction and cardiovascular disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
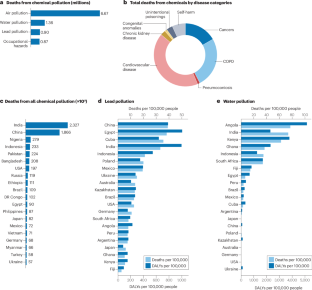
Similar content being viewed by others
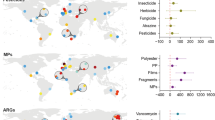
Soil contamination in nearby natural areas mirrors that in urban greenspaces worldwide

Human health risk assessment of heavy metals in residential soil—Houston, Texas
Study on the risk of soil heavy metal pollution in typical developed cities in eastern China
Fuller, R. et al. Pollution and health: a progress update. Lancet Planet Health 6 , e535–e547 (2022).
Article PubMed Google Scholar
Landrigan, P. J. et al. The Lancet Commission on Pollution and Health. Lancet 391 , 462–512 (2018).
Munzel, T., Hahad, O., Daiber, A. & Landrigan, P. J. Soil and water pollution and human health: what should cardiologists worry about? Cardiovasc. Res. 119 , 440–449 (2023).
GBD 2015 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388 , 1603–1658 (2016).
Article Google Scholar
Institute for Health Metrics and Evaluation. Global health data exchange tool. Global Health Data Exchange http://ghdx.healthdata.org/gbd-results-tool (2023).
Lelieveld, J. et al. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur. Heart J. 40 , 1590–1596 (2019).
Article CAS PubMed PubMed Central Google Scholar
Lelieveld, J. et al. Air pollution deaths attributable to fossil fuels: observational and modelling study. BMJ 383 , e077784 (2023).
Article PubMed PubMed Central Google Scholar
World Health Organization. The public health impact of chemicals: knowns and unknowns – data addendum for 2019. WHO https://www.who.int/publications/i/item/WHO-HEP-ECH-EHD-21.01 (2021).
World Health Organization. Global action plan for the prevention and control of non-communicable diseases 2013–2020. WHO https://www.who.int/publications/i/item/9789241506236 (2013).
United Nations Environment Program. Global assessment of soil pollution. UNEP https://www.unep.org/resources/report/global-assessment-soil-pollution (2021).
United Nations Environment Program. Soil pollution a risk to our health and food security. UNEP https://www.unep.org/news-and-stories/story/soil-pollution-risk-our-health-and-food-security (2020).
Mielke, H. W. & Reagan, P. L. Soil is an important pathway of human lead exposure. Environ. Health Perspect. 106 , 217–229 (1998).
CAS PubMed PubMed Central Google Scholar
European Envrionment Agency. Water Pollution and Health. EEA https://www.eea.europa.eu/publications/zero-pollution/health/water-pollution (2022).
United Nations. Water. summary progress update 2021: SDG 6 – Water and sanitation for all. UN-Water http://www.unwater.org/sites/default/files/app/uploads/2021/12/SDG-6-Summary-Progress-Update-2021_Version-July-2021a.pdf (2021).
Global Allliance on Health and Pollution. Pollution and health metrics. GAHP https://gahp.net/wp-content/uploads/2019/12/PollutionandHealthMetrics-final-12_18_2019.pdf (2019).
World Health Organization. The public health impact of chemicals: knowns and unknowns. WHO http://www.who.int/publications/i/item/WHO-FWC-PHE-EPE-16.01-eng (2016).
World Health Organization. Food safety. WHO http://www.who.int/news-room/fact-sheets/detail/food-safety (2022).
European Commission. The European Human Biomonitoring Initiative. HBM4EU https://www.hbm4eu.eu/ (2016).
Centers for Disease Control and Prevention. National biomonitoring program. CDC https://www.cdc.gov/biomonitoring/index.html (2018).
Persson, L. et al. Outside the safe operating space of the planetary boundary for novel entities. Environ. Sci. Technol. 56 , 1510–1521 (2022).
United Nations Environment Program. Global chemicals outlook II – from legacies to innovative solutions: Implementing the 2030 Agenda for Sustainable Development (Part I). UNEP https://www.unep.org/topics/chemicals-and-pollution-action/chemicals-management/global-chemicals-outlook (2019).
Maertens, A., Golden, E. & Hartung, T. Avoiding regrettable substitutions: green toxicology for sustainable chemistry. ACS Sustain. Chem. Eng. 9 , 7749–7758 (2021).
Peters, A., Nawrot, T. S. & Baccarelli, A. A. Hallmarks of environmental insults. Cell 184 , 1455–1468 (2021).
La Merrill, M. A. et al. Consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification. Nat. Rev. Endocrinol. 16 , 45–57 (2020).
Cosselman, K. E., Navas-Acien, A. & Kaufman, J. D. Environmental factors in cardiovascular disease. Nat. Rev. Cardiol. 12 , 627–642 (2015).
Article CAS PubMed Google Scholar
Liu, Z., Lu, Y., Zhong, K., Wang, C. & Xu, X. The associations between endocrine disrupting chemicals and markers of inflammation and immune responses: a systematic review and meta-analysis. Ecotoxicol. Environ. Saf. 234 , 113382 (2022).
Chen, J. C. et al. Associations of per- and polyfluoroalkyl substances, polychlorinated biphenyls, organochlorine pesticides, and polybrominated diphenyl ethers with oxidative stress markers: a systematic review and meta-analysis. Environ. Res. 239 , 117308 (2023).
Daiber, A. et al. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 174 , 1591–1619 (2017).
Wenzel, P., Kossmann, S., Munzel, T. & Daiber, A. Redox regulation of cardiovascular inflammation – immunomodulatory function of mitochondrial and Nox-derived reactive oxygen and nitrogen species. Free Radic. Biol. Med. 109 , 48–60 (2017).
Vogel, C. F. A., Van Winkle, L. S., Esser, C. & Haarmann-Stemmann, T. The aryl hydrocarbon receptor as a target of environmental stressors – implications for pollution mediated stress and inflammatory responses. Redox Biol. 34 , 101530 (2020).
Martinez-Pinna, J. et al. Endocrine disruptors in plastics alter β-cell physiology and increase the risk of diabetes mellitus. Am. J. Physiol. Endocrinol. Metab. 324 , E488–E505 (2023).
Sule, R. O., Condon, L. & Gomes, A. V. A common feature of pesticides: oxidative stress – the role of oxidative stress in pesticide-induced toxicity. Oxid. Med. Cell Longev. 2022 , 5563759 (2022).
Rasin, P. & Sreekanth, A. Cadmium exposure and cardiovascular diseases. Chem. Res. Toxicol. 36 , 1441–1443 (2023).
Singh, N., Kumar, A., Gupta, V. K. & Sharma, B. Biochemical and molecular bases of lead-induced toxicity in mammalian systems and possible mitigations. Chem. Res. Toxicol. 31 , 1009–1021 (2018).
Hu, H., Chen, Y., Jing, L., Zhai, C. & Shen, L. The link between ferroptosis and cardiovascular diseases: a novel target for treatment. Front. Cardiovasc. Med. 8 , 710963 (2021).
Farina, M., Aschner, M. & Rocha, J. B. Oxidative stress in MeHg-induced neurotoxicity. Toxicol. Appl. Pharmacol. 256 , 405–417 (2011).
Kempuraj, D. et al. Mercury induces inflammatory mediator release from human mast cells. J. Neuroinflammation 7 , 20 (2010).
Ellinsworth, D. C. Arsenic, reactive oxygen, and endothelial dysfunction. J. Pharmacol. Exp. Ther. 353 , 458–464 (2015).
Jomova, K. & Valko, M. Advances in metal-induced oxidative stress and human disease. Toxicology 283 , 65–87 (2011).
Gaetke, L. M. & Chow, C. K. Copper toxicity, oxidative stress, and antioxidant nutrients. Toxicology 189 , 147–163 (2003).
Kang, Y. J. Copper and homocysteine in cardiovascular diseases. Pharmacol. Ther. 129 , 321–331 (2011).
Yang, S. et al. Copper homeostasis and cuproptosis in atherosclerosis: metabolism, mechanisms and potential therapeutic strategies. Cell Death Discov. 10 , 25 (2024).
Dai, H., Wang, L., Li, L., Huang, Z. & Ye, L. Metallothionein 1: a new spotlight on inflammatory diseases. Front. Immunol. 12 , 739918 (2021).
Paniagua, L., Diaz-Cueto, L., Huerta-Reyes, M. & Arechavaleta-Velasco, F. Cadmium exposure induces interleukin-6 production via ROS-dependent activation of the ERK1/2 but independent of JNK signaling pathway in human placental JEG-3 trophoblast cells. Reprod. Toxicol. 89 , 28–34 (2019).
Zheng, X., Zhang, K., Zhao, Y. & Fent, K. Environmental chemicals affect circadian rhythms: an underexplored effect influencing health and fitness in animals and humans. Environ. Int. 149 , 106159 (2021).
Li, H. et al. Influence of mental stress and environmental toxins on circadian clocks: implications for redox regulation of the heart and cardioprotection. Br. J. Pharmacol. 177 , 5393–5412 (2020).
Lim, F. L., Currie, R. A., Orphanides, G. & Moggs, J. G. Emerging evidence for the interrelationship of xenobiotic exposure and circadian rhythms: a review. Xenobiotica 36 , 1140–1151 (2006).
Parmalee, N. L. & Aschner, M. Metals and circadian rhythms. Adv. Neurotoxicol. 1 , 119–130 (2017).
Lafuente, A. The hypothalamic-pituitary-gonadal axis is target of cadmium toxicity. An update of recent studies and potential therapeutic approaches. Food Chem. Toxicol. 59 , 395–404 (2013).
Agency for Toxic Substances and Disease Registry. Interaction profile for: benzene, toluene, ethylbenzene, and xylenes (BTEX) (US Department of Health and Human Services, 2004). https://www.atsdr.cdc.gov/interactionprofiles/ip-btex/ip05.pdf .
Drwal, E., Rak, A. & Gregoraszczuk, E. L. Review: Polycyclic aromatic hydrocarbons (PAHs) – action on placental function and health risks in future life of newborns. Toxicology 411 , 133–142 (2019).
Institute for Health and Consumer Protection. Summary risk assessment report: Phenol. EUR 22522 EN/1 (Publications Office of the European Union, 2006). https://echa.europa.eu/documents/10162/3e04f30d-9953-4824-ba04-defa32a130fa .
Galbraith, D., Gross, S. A. & Paustenbach, D. Benzene and human health: a historical review and appraisal of associations with various diseases. Crit. Rev. Toxicol. 40 , 1–46 (2010).
Wang, Y. L., Lee, Y. H., Chiu, I. J., Lin, Y. F. & Chiu, H. W. Potent impact of plastic nanomaterials and micromaterials on the food chain and human health. Int. J. Mol. Sci. 21 , 1727 (2020).
Jamieson, A. J., Malkocs, T., Piertney, S. B., Fujii, T. & Zhang, Z. Bioaccumulation of persistent organic pollutants in the deepest ocean fauna. Nat. Ecol. Evol. 1 , 51 (2017).
Landrigan, P. J. & Goldman, L. R. Children’s vulnerability to toxic chemicals: a challenge and opportunity to strengthen health and environmental policy. Health Aff. 30 , 842–850 (2011).
Lind, L. & Lind, P. M. Can persistent organic pollutants and plastic-associated chemicals cause cardiovascular disease? J. Intern. Med. 271 , 537–553 (2012).
Dunder, L. et al. Plasma levels of per- and polyfluoroalkyl substances (PFAS) and cardiovascular disease – results from two independent population-based cohorts and a meta-analysis. Environ. Int. 181 , 108250 (2023).
Honda-Kohmo, K., Hutcheson, R., Innes, K. E. & Conway, B. N. Perfluoroalkyl substances are inversely associated with coronary heart disease in adults with diabetes. J. Diabetes Complications 33 , 407–412 (2019).
Chowdhury, R. et al. Environmental toxic metal contaminants and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 362 , k3310 (2018).
Meneguzzi, A., Fava, C., Castelli, M. & Minuz, P. Exposure to perfluoroalkyl chemicals and cardiovascular disease: experimental and epidemiological evidence. Front. Endocrinol. 12 , 706352 (2021).
Zhao, L. et al. The associations between organophosphate pesticides (OPs) and respiratory disease, diabetes mellitus, and cardiovascular disease: a review and meta-analysis of observational studies. Toxics 11 , 741 (2023).
Fawell, J. & Nieuwenhuijsen, M. J. Contaminants in drinking water. Br. Med. Bull. 68 , 199–208 (2003).
Jarup, L. Hazards of heavy metal contamination. Br. Med. Bull. 68 , 167–182 (2003).
Chowdhury, R. et al. Reducing NCDs globally: the under-recognised role of environmental risk factors. Lancet 392 , 212 (2018).
National Research Council. Toxicological Effects of Methylmercury (National Academy Press, 2000). https://nap.nationalacademies.org/catalog/9899/toxicological-effects-of-methylmercury .
Lancereaux, E. Nephrite et arthrite saturnine: coincidences de ces affections; parallele avec la nephrite et l’arthrite gouttesses. Trans. Int. Med. Congr. 2 , 193–202 (1881).
Google Scholar
Schwartz, J. Lead, blood pressure, and cardiovascular disease in men. Arch. Environ. Health 50 , 31–37 (1995).
Navas-Acien, A., Guallar, E., Silbergeld, E. K. & Rothenberg, S. J. Lead exposure and cardiovascular disease – a systematic review. Environ. Health Perspect. 115 , 472–482 (2007).
Schober, S. E., Mirel, L. B., Graubard, B. I., Brody, D. J. & Flegal, K. M. Blood lead levels and death from all causes, cardiovascular disease, and cancer: results from the NHANES III mortality study. Environ. Health Perspect. 114 , 1538–1541 (2006).
Lanphear, B. P., Rauch, S., Auinger, P., Allen, R. W. & Hornung, R. W. Low-level lead exposure and mortality in US adults: a population-based cohort study. Lancet Public Health 3 , e177–e184 (2018).
Larsen, B. & Sanchez-Triana, E. Global health burden and cost of lead exposure in children and adults: a health impact and economic modelling analysis. Lancet Planet Health 7 , e831–e840 (2023).
Zhu, K. et al. Associations of exposure to lead and cadmium with risk of all-cause and cardiovascular disease mortality among patients with type 2 diabetes. Environ. Sci. Pollut. Res. Int. 29 , 76805–76815 (2022).
Xing, X. et al. Association of selenium and cadmium with heart failure and mortality based on the National Health and Nutrition Examination Survey. J. Hum. Nutr. Diet. 36 , 1496–1506 (2023).
Tellez-Plaza, M., Jones, M. R., Dominguez-Lucas, A., Guallar, E. & Navas-Acien, A. Cadmium exposure and clinical cardiovascular disease: a systematic review. Curr. Atheroscler. Rep. 15 , 356 (2013).
Duan, W. et al. Levels of a mixture of heavy metals in blood and urine and all-cause, cardiovascular disease and cancer mortality: a population-based cohort study. Environ. Pollut. 263 , 114630 (2020).
Lim, K. M. et al. Low-level mercury can enhance procoagulant activity of erythrocytes: a new contributing factor for mercury-related thrombotic disease. Environ. Health Perspect. 118 , 928–935 (2010).
Morin, Y. & Daniel, P. Quebec beer-drinkers’ cardiomyopathy: etiological considerations. Can. Med. Assoc. J. 97 , 926–928 (1967).
Perez, A. L. & Tang, W. H. Contribution of environmental toxins in the pathogenesis of idiopathic cardiomyopathies. Curr. Treat. Options Cardiovasc. Med. 17 , 381 (2015).
Stea, F., Bianchi, F., Cori, L. & Sicari, R. Cardiovascular effects of arsenic: clinical and epidemiological findings. Environ. Sci. Pollut. Res. Int. 21 , 244–251 (2014).
Moon, K., Guallar, E. & Navas-Acien, A. Arsenic exposure and cardiovascular disease: an updated systematic review. Curr. Atheroscler. Rep. 14 , 542–555 (2012).
Tseng, W. P. Black foot disease in Taiwan: a 30-year follow-up study. Angiology 40 , 547–558 (1989).
Kinsman, G. D., Howard, A. N., Stone, D. L. & Mullins, P. A. Studies in copper status and atherosclerosis. Biochem. Soc. Trans. 18 , 1186–1188 (1990).
United Nations Environment Programme. The Stockholm Convention on Persistent Organic Pollutants, http://chm.pops.int/TheConvention/Overview/TextoftheConvention/tabid/2232/Default.aspx (2019).
Agency for Toxic Substances and Disease Registry. Toxicological profile for chlorinated dibenzo-p-dioxins (CDDs) (ATSDR, 1998).
Consonni, D. et al. Mortality in a population exposed to dioxin after the Seveso, Italy, accident in 1976: 25 years of follow-up. Am. J. Epidemiol. 167 , 847–858 (2008).
Lee, D. H. et al. A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: results from the National Health and Examination Survey 1999-2002. Diabetes Care 29 , 1638–1644 (2006).
Lim, J. S., Lee, D. H. & Jacobs, D. R. Jr Association of brominated flame retardants with diabetes and metabolic syndrome in the U.S. population, 2003-2004. Diabetes Care 31 , 1802–1807 (2008).
Lang, I. A. et al. Association of urinary bisphenol A concentration with medical disorders and laboratory abnormalities in adults. JAMA 300 , 1303–1310 (2008).
Moon, S. et al. Effects of bisphenol A on cardiovascular disease: an epidemiological study using National Health and Nutrition Examination Survey 2003-2016 and meta-analysis. Sci. Total Environ. 763 , 142941 (2021).
Wang, R. et al. The bisphenol F and bisphenol S and cardiovascular disease: results from NHANES 2013–2016. Environ. Sci. Eur. 34 , 4 (2022).
Article CAS Google Scholar
Chen, Z., He, J. & Shi, W. Association between urinary environmental phenols and the prevalence of cardiovascular diseases in US adults. Environ. Sci. Pollut. Res. Int. 29 , 42947–42954 (2022).
Moreno-Gómez-Toledano, R. Relationship between emergent BPA-substitutes and renal and cardiovascular diseases in adult population. Environ. Pollut. 313 , 120106 (2022).
Lu, Y., Chen, S., Jin, H., Tang, L. & Xia, M. Associations of bisphenol F and S, as substitutes for bisphenol A, with cardiovascular disease in American adults. J. Appl. Toxicol. 43 , 500–507 (2023).
Bar-Meir, E. et al. Guidelines for treating cardiac manifestations of organophosphates poisoning with special emphasis on long QT and Torsades De Pointes. Crit. Rev. Toxicol. 37 , 279–285 (2007).
Humblet, O., Birnbaum, L., Rimm, E., Mittleman, M. A. & Hauser, R. Dioxins and cardiovascular disease mortality. Environ. Health Perspect. 116 , 1443–1448 (2008).
Gustavsson, P. & Hogstedt, C. A cohort study of Swedish capacitor manufacturing workers exposed to polychlorinated biphenyls (PCBs). Am. J. Ind. Med. 32 , 234–239 (1997).
OECD. Global plastics outlook. OECDiLibrary http://www.oecd-ilibrary.org/environment/global-plastics-outlook_aa1edf33-en (2022).
European Environment Agency. Microplastics from textiles: towards a circular economy for textiles in Europe. EEA http://www.eea.europa.eu/publications/microplastics-from-textiles-towards-a (2022).
Wright, S. L., Thompson, R. C. & Galloway, T. S. The physical impacts of microplastics on marine organisms: a review. Environ. Pollut. 178 , 483–492 (2013).
Yong, C. Q. Y., Valiyaveettil, S. & Tang, B. L. Toxicity of microplastics and nanoplastics in mammalian systems. Int. J. Environ. Res. Public Health 17 , 1509 (2020).
Oh, N. & Park, J. H. Endocytosis and exocytosis of nanoparticles in mammalian cells. Int. J. Nanomed. 9 , 51–63 (2014).
Zhang, S., Gao, H. & Bao, G. Physical principles of nanoparticle cellular endocytosis. ACS Nano 9 , 8655–8671 (2015).
Gong, T., Liu, L., Jiang, W. & Zhou, R. DAMP-sensing receptors in sterile inflammation and inflammatory diseases. Nat. Rev. Immunol. 20 , 95–112 (2020).
Jeong, J. & Choi, J. Adverse outcome pathways potentially related to hazard identification of microplastics based on toxicity mechanisms. Chemosphere 231 , 249–255 (2019).
Horstmann, H., Ng, C. P., Tang, B. L. & Hong, W. Ultrastructural characterization of endoplasmic reticulum–Golgi transport containers (EGTC). J. Cell Sci. 115 , 4263–4273 (2002).
Treyer, A., Pujato, M., Pechuan, X. & Musch, A. Iterative sorting of apical and basolateral cargo in Madin-Darby canine kidney cells. Mol. Biol. Cell 27 , 2259–2271 (2016).
Lim, S. L. et al. Targeted metabolomics reveals differential biological effects of nanoplastics and nanoZnO in human lung cells. Nanotoxicology 13 , 1117–1132 (2019).
Cordani, M. & Somoza, A. Targeting autophagy using metallic nanoparticles: a promising strategy for cancer treatment. Cell Mol. Life Sci. 76 , 1215–1242 (2019).
Besseling, E., Wang, B., Lurling, M. & Koelmans, A. A. Nanoplastic affects growth of S. obliquus and reproduction of D. magna . Environ. Sci. Technol. 48 , 12336–12343 (2014).
Liu, Z. et al. Age-dependent survival, stress defense, and AMPK in Daphnia pulex after short-term exposure to a polystyrene nanoplastic. Aquat. Toxicol. 204 , 1–8 (2018).
Greven, A. C. et al. Polycarbonate and polystyrene nanoplastic particles act as stressors to the innate immune system of fathead minnow ( Pimephales promelas ). Environ. Toxicol. Chem. 35 , 3093–3100 (2016).
Foley, C. J., Feiner, Z. S., Malinich, T. D. & Hook, T. O. A meta-analysis of the effects of exposure to microplastics on fish and aquatic invertebrates. Sci. Total Environ. 631-632 , 550–559 (2018).
Bucci, K., Tulio, M. & Rochman, C. M. What is known and unknown about the effects of plastic pollution: a meta-analysis and systematic review. Ecol. Appl. 30 , e02044 (2019).
De-la-Torre, G. E. Microplastics: an emerging threat to food security and human health. J. Food Sci. Technol. 57 , 1601–1608 (2020).
Shiwakoti, S. et al. Effects of polystyrene nanoplastics on endothelium senescence and its underlying mechanism. Environ. Int. 164 , 107248 (2022).
Zhao, J. et al. Polystyrene bead ingestion promotes adiposity and cardiometabolic disease in mice. Ecotoxicol. Environ. Saf. 232 , 113239 (2022).
Wei, J. et al. The impact of polystyrene microplastics on cardiomyocytes pyroptosis through NLRP3/caspase-1 signaling pathway and oxidative stress in Wistar rats. Environ. Toxicol. 36 , 935–944 (2021).
Li, Z. et al. Polystyrene microplastics cause cardiac fibrosis by activating Wnt/β-catenin signaling pathway and promoting cardiomyocyte apoptosis in rats. Environ. Pollut. 265 , 115025 (2020).
Wang, X. et al. Nanoplastic-induced vascular endothelial injury and coagulation dysfunction in mice. Sci. Total Environ. 865 , 161271 (2023).
Zhu, X. et al. Micro- and nanoplastics: a new cardiovascular risk factor? Environ. Int. 171 , 107662 (2023).
Ali, N. et al. The potential impacts of micro-and-nano plastics on various organ systems in humans. EBioMedicine 99 , 104901 (2023).
Marfella, R. et al. Microplastics and nanoplastics in atheromas and cardiovascular events. N. Engl. J. Med. 390 , 900–910 (2024).
Beuchle, R., Achard, F., Bourgoin, C., Vancutsem, C. Deforestation and forest degradation in the Amazon – updated status and trends for the year 2021 (Publications Office of the European Union, 2022).
Veldkamp, E., Schmidt, M., Powers, J. S. & Corre, M. D. Deforestation and reforestation impacts on soils in the tropics. Nat. Rev. Earth Environ. 1 , 590–605 (2020).
United Nations. The global forest goals report 2021. UN https://www.un.org/esa/forests/wp-content/uploads/2021/08/Global-Forest-Goals-Report-2021.pdf (2021).
Johnston, F. H. et al. Estimated global mortality attributable to smoke from landscape fires. Environ. Health Perspect. 120 , 695–701 (2012).
Artiola, J. F., Walworth, J. L., Musil, S. A. & Crimmins, M. A. in Environmental and Pollution Science 3rd edn (eds Brusseau, M. L., Pepper, I. L. & Gerba, C. P.) 219–235 (Academic Press, 2019).
US Environmental Protection Agency. Air quality and climate change research. EPA http://www.epa.gov/air-research/air-quality-and-climate-change-research#:~:Text=Emissions%20of%20pollutants%20into%20the,cooling%20effects%20on%20the%20climate (2024).
UN Report: Global Assessment of Soil Pollution. Chapter 4. Environmental, Health and Socio-economic Impacts of Soil Pollution. 4.4 Socio-economic impacts of soil pollution. FAO http://www.fao.org/3/cb4894en/online/src/html/chapter-04-4.html (2017).
European Environment Agency. Soil moisture deficit, EEA http://www.eea.europa.eu/en/analysis/indicators/soil-moisture-deficit (2021).
US Environmental Protection Agency. Climate change indicators: permafrost. EPA https://www.epa.gov/climate-indicators/climate-change-indicators-permafrost#:~:Text=Additionally%2C%20organic%20matter%20 (2021).
United Nations. Water – at the center of the climate crisis. UN https://www.un.org/en/climatechange/science/climate-issues/water (2021).
Liu, J. et al. Emission control priority of PM 2.5 -bound heavy metals in different seasons: a comprehensive analysis from health risk perspective. Sci. Total Environ. 644 , 20–30 (2018).
Prospero, J. M., Ginoux, P., Torres, O., Nicholson, S. E. & Gill, T. E. Environmental characterization of global sources of atmospheric soil dust identified with the Nimbus 7 Total Ozone Mapping Spectrometer (TOMS) absorbing aerosol product. Rev. Geophys. 40 , 2-1–2-31 (2002).
Chen, W., Meng, H., Song, H. & Zheng, H. Progress in dust modelling, global dust budgets, and soil organic carbon dynamics. Land 11 , 176 (2022).
Kok, J. F. S. et al. Mineral dust aerosol impacts on global climate and climate change. Nat. Rev. Earth Environ. 4 , 71–86 (2023).
Giannadaki, D., Pozzer, A. & Lelieveld, J. Modeled global effects of airborne desert dust on air quality and premature mortality. Atmos. Chem. Phys. 14 , 957–968 (2014).
Kotsyfakis, M., Zarogiannis, S. G. & Patelarou, E. The health impact of Saharan dust exposure. Int. J. Occup. Med. Environ. Health 32 , 749–760 (2019).
Gomez, A. R. et al. The projected future degradation in air quality is caused by more abundant natural aerosols in a warmer world. Commun. Earth Environ. 4 , 22 (2023).
Achakulwisut, P. et al. Effects of increasing aridity on ambient dust and public health in the U.S. Southwest under climate change. Geohealth 3 , 127–144 (2019).
Fussell, J. C. & Kelly, F. J. Mechanisms underlying the health effects of desert sand dust. Environ. Int. 157 , 106790 (2021).
Miller, M. R. Oxidative stress and the cardiovascular effects of air pollution. Free Radic. Biol. Med. 151 , 69–87 (2020).
Lwin, K. S. et al. Effects of desert dust and sandstorms on human health: a scoping review. Geohealth 7 , e2022GH000728 (2023).
Yu, Z. et al. Simulating the impact of long-range-transported Asian mineral dust on the formation of sulfate and nitrate during the KORUS-AQ Campaign. ACS Earth Space Chem. 4 , 1039–1049 (2020).
Karydis, V. A., Tsimpidi, A. P., Pozzer, A., Astitha, M. & Lelieveld, J. Effects of mineral dust on global atmospheric nitrate concentrations. Atmos. Chem. Phys. 16 , 1491–1509 (2016).
Ho, K. F. et al. Contributions of local pollution emissions to particle bioreactivity in downwind cities in China during Asian dust periods. Environ. Pollut. 245 , 675–683 (2019).
Lovett, C., Sowlat, M. H., Saliba, N. A., Shihadeh, A. L. & Sioutas, C. Oxidative potential of ambient particulate matter in Beirut during Saharan and Arabian dust events. Atmos. Environ. 188 , 34–42 (2018).
Chirizzi, D. et al. Influence of Saharan dust outbreaks and carbon content on oxidative potential of water-soluble fractions of PM 2.5 and PM 10 . Atmos. Environ. 163 , 1–8 (2017).
Yang, A., Tan, Q., Rajapakshe, C., Chin, M. & Yu, H. Global premature mortality by dust and pollution PM 2.5 estimated from aerosol reanalysis of the modern-era retrospective analysis for research and applications, version 2. Sec. Atmos. Clim. 10 , 975755 (2022).
Kojima, S. et al. Asian dust exposure triggers acute myocardial infarction. Eur. Heart J. 38 , 3202–3208 (2017).
Galloway, J. N. et al. Transformation of the nitrogen cycle: recent trends, questions, and potential solutions. Science 320 , 889–892 (2008).
Fowler, D. et al. The global nitrogen cycle in the twenty-first century. Philos. Trans. R. Soc. Lond. B Biol. Sci. 368 , 20130164 (2013).
Kicińska, A., Radoslaw, P. & Izquierdo-Diaz, M. Changes in soil pH and mobility of heavy metals in contaminated soils. Eur. J. Soil Sci. 73 , e13203 (2022).
Zhang, X., Ward, B. B. & Sigman, D. M. Global nitrogen cycle: critical enzymes, organisms, and processes for nitrogen budgets and dynamics. Chem. Rev. 120 , 5308–5351 (2020).
McDuffie, E. E. et al. Source sector and fuel contributions to ambient PM 2.5 and attributable mortality across multiple spatial scales. Nat. Commun. 12 , 3594 (2021).
Lelieveld, J., Evans, J. S., Fnais, M., Giannadaki, D. & Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 525 , 367–371 (2015).
Lelieveld, J. et al. Effects of fossil fuel and total anthropogenic emission removal on public health and climate. Proc. Natl Acad. Sci. USA 116 , 7192–7197 (2019).
Gumanova, N. G., Deev, A. D., Zhang, W., Kots, A. Y. & Shalnova, S. A. Serum nitrite and nitrate levels, NOx, can predict cardiovascular mortality in the elderly in a 3-year follow-up study. Biofactors 43 , 82–89 (2017).
Gumanova, N. G., Deev, A. D., Kots, A. Y. & Shalnova, S. A. Elevated levels of serum nitrite and nitrate, NOx, are associated with increased total and cardiovascular mortality in an 8-year follow-up study. Eur. J. Clin. Invest. 49 , e13061 (2019).
Bahadoran, Z., Mirmiran, P., Tahmasebinejad, Z., Azizi, F. & Ghasemi, A. Serum nitric oxide metabolites and hard clinical endpoints: a population-based prospective study. Scand. Cardiovasc. J. 53 , 176–182 (2019).
Wang, M. et al. Exposure to PM 2.5 and its five constituents is associated with the incidence of type 2 diabetes mellitus: a prospective cohort study in northwest China. Environ. Geochem. Health 46 , 34 (2024).
United Nations. World population prospects 2019: highlights. UN http://population.un.org/wpp/Publications/Files/wpp2019_10KeyFindings.pdf (2019).
Dye, C. Health and urban living. Science 319 , 766–769 (2008).
Ezzati, M. et al. Cities for global health. BMJ 363 , k3794 (2018).
Bikis, A. Urban air pollution and greenness in relation to public health. J. Environ. Public Health 2023 , 8516622 (2023).
European Environment Agency. Air pollution still too high across Europe. EEA http://www.eea.europa.eu/highlights/air-pollution-still-too-high (2018).
Hunter, R. F. et al. Advancing urban green and blue space contributions to public health. Lancet Public Health 8 , e735–e742 (2023).
Munzel, T. et al. Heart healthy cities: genetics loads the gun but the environment pulls the trigger. Eur. Heart J. 42 , 2422–2438 (2021).
Baumgartner, J., Brauer, M. & Ezzati, M. The role of cities in reducing the cardiovascular impacts of environmental pollution in low- and middle-income countries. BMC Med. 18 , 39 (2020).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health 6 , e1077–e1086 (2018).
Munzel, T., Sorensen, M. & Daiber, A. Transportation noise pollution and cardiovascular disease. Nat. Rev. Cardiol. 18 , 619–636 (2021).
Nieuwenhuijsen, M. J. New urban models for more sustainable, liveable and healthier cities post Covid19; reducing air pollution, noise and heat island effects and increasing green space and physical activity. Environ. Int. 157 , 106850 (2021).
Zota, A. R., Singla, V., Adamkiewicz, G., Mitro, S. D. & Dodson, R. E. Reducing chemical exposures at home: opportunities for action. J. Epidemiol. Community Health 71 , 937–940 (2017).
Hahad, O. et al. Noise and air pollution as risk factors for hypertension: part II – pathophysiologic insight. Hypertension 80 , 1384–1392 (2023).
European Commission. Zero Pollution Action Plan: towards zero pollution for air, water and soil. https://environment.ec.europa.eu/strategy/zero-pollution-action-plan_en# (2021).
European Environment Agency. Soil. EEA http://www.eea.europa.eu/en/topics/in-depth/soil# (2023).
European Environment Agency. Progress in the management of contaminated sites in Europe. EEA http://www.eea.europa.eu/en/analysis/indicators/progress-in-the-management-of (2022).
Goldsborough, E.III, Gopal, M., McEvoy, J. W., Blumenthal, R. S. & Jacobsen, A. P. Pollution and cardiovascular health: a contemporary review of morbidity and implications for planetary health. Am. Heart J. 25 , 100231 (2023).
Tsoi, M. F., Lo, C. W. H., Cheung, T. T. & Cheung, B. M. Y. Blood lead level and risk of hypertension in the United States National Health and Nutrition Examination Survey 1999-2016. Sci. Rep. 11 , 3010 (2021).
Cook, M. K., Zhang, J. & Wei, Y. Blood lead levels and risk of deaths from cardiovascular disease. Am. J. Cardiol. 173 , 132–138 (2022).
Lee, M. S., Park, S. K., Hu, H. & Lee, S. Cadmium exposure and cardiovascular disease in the 2005 Korea National Health and Nutrition Examination Survey. Environ. Res. 111 , 171–176 (2011).
Tellez-Plaza, M. et al. Cadmium exposure and incident cardiovascular disease. Epidemiology 24 , 421–429 (2013).
Li, Z. et al. Association between exposure to cadmium and risk of all-cause and cause-specific mortality in the general US adults: a prospective cohort study. Chemosphere 307 , 136060 (2022).
Tellez-Plaza, M. et al. Cadmium exposure and all-cause and cardiovascular mortality in the U.S. general population. Environ. Health Perspect. 120 , 1017–1022 (2012).
Nigra, A. E., Moon, K. A., Jones, M. R., Sanchez, T. R. & Navas-Acien, A. Urinary arsenic and heart disease mortality in NHANES 2003-2014. Environ. Res. 200 , 111387 (2021).
Sun, Y. et al. Association of seafood consumption and mercury exposure with cardiovascular and all-cause mortality among US adults. JAMA Netw. Open 4 , e2136367 (2021).
Isiozor, N. M. et al. Serum copper and the risk of cardiovascular disease death in Finnish men. Nutr. Metab. Cardiovasc. Dis. 33 , 151–157 (2023).
Shankar, A., Teppala, S. & Sabanayagam, C. Bisphenol A and peripheral arterial disease: results from the NHANES. Environ. Health Perspect. 120 , 1297–1300 (2012).
Sturgeon, S. R., Flynn, D., Kaiser, A. B. & Reeves, K. W. Urinary levels of phthalate metabolites and cardiovascular disease mortality (NHANES, 1999-2008). Int. J. Hyg. Environ. Health 219 , 876–882 (2016).
Bao, W. et al. Association between bisphenol A exposure and risk of all-cause and cause-specific mortality in US adults. JAMA Netw. Open 3 , e2011620 (2020).
Cai, S. et al. Relationship between urinary bisphenol A levels and cardiovascular diseases in the U.S. adult population, 2003-2014. Ecotoxicol. Environ. Saf. 192 , 110300 (2020).
Chen, M. et al. Relationship between bisphenol A and the cardiovascular disease metabolic risk factors in American adults: a population-based study. Chemosphere 324 , 138289 (2023).
Chen, S. et al. Association of urinary bisphenol A with cardiovascular and all-cause mortality: National Health and Nutrition Examination Survey (NHANES) 2003-2016. Environ. Sci. Pollut. Res. Int. 30 , 51217–51227 (2023).
Shankar, A., Xiao, J. & Ducatman, A. Perfluorooctanoic acid and cardiovascular disease in US adults. Arch. Intern. Med. 172 , 1397–1403 (2012).
Huang, M. et al. Serum polyfluoroalkyl chemicals are associated with risk of cardiovascular diseases in national US population. Environ. Int. 119 , 37–46 (2018).
Simpson, C., Winquist, A., Lally, C. & Steenland, K. Relation between perfluorooctanoic acid exposure and strokes in a large cohort living near a chemical plant. Environ. Res. 127 , 22–28 (2013).
Xue, Q. et al. Association between pyrethroid exposure and cardiovascular disease: a national population-based cross-sectional study in the US. Environ. Int. 153 , 106545 (2021).
Bao, W., Liu, B., Simonsen, D. W. & Lehmler, H. J. Association between exposure to pyrethroid insecticides and risk of all-cause and cause-specific mortality in the general US adult population. JAMA Intern. Med. 180 , 367–374 (2020).
Chang, J. W. et al. Predicting the risk of cardiovascular disease in people exposed to moderate to high levels of dioxin. J. Hazard Mater. 198 , 317–322 (2011).
Ha, M. H., Lee, D. H. & Jacobs, D. R. Association between serum concentrations of persistent organic pollutants and self-reported cardiovascular disease prevalence: results from the National Health and Nutrition Examination Survey, 1999-2002. Environ. Health Perspect. 115 , 1204–1209 (2007).
Lin, Y. S. et al. Environmental exposure to dioxin-like compounds and the mortality risk in the U.S. population. Int. J. Hyg. Environ. Health 215 , 541–546 (2012).
Global Alliance on Health and Pollution. Pollution and Health Metrics. GAHP https://gahp.net/wp-content/uploads/2019/12/PollutionandHealthMetrics-final-12_18_2019.pdf (2019).
Tang, F. H. M., Lenzen, M., McBratney, A. & Maggi, F. Risk of pesticide pollution at the global scale. Nat. Geosci. 14 , 206–210 (2021).
Amini, M. et al. Statistical modeling of global geogenic arsenic contamination in groundwater. Environ. Sci. Technol. 42 , 3669–3675 (2008).
Pure Earth. Lead country statistics. https://leadpollution.org/ (2019).
Steenhuisen, F. & Wilson, S. J. Development and application of an updated geospatial distribution model for gridding 2015 global mercury emissions. Atmos. Environ. 211 , 138–150 (2019).
Lebreton, L. Where mismanaged plastic waste is generated and possible paths of change. The Ocean Cleanup https://theoceancleanup.com/updates/where-mismanaged-plastic-waste-is-generated-and-possible-paths-of-change/ (2019).
Global Water Intelligence. Agencies plead for global action on water pollution. https://www.globalwaterintel.com/news/2019/34/agencies-plead-for-global-action-on-water-pollution (2019).
FAO & UNEP. Global Assessment of Soil Pollution Ch. 4. Environmental, health and socio-economic impacts of soil pollution. 4.3 Soil pollution and risk to human health. https://openknowledge.fao.org/server/api/core/bitstreams/fe5df8d6-6b19-4def-bdc6-62886d824574/content/src/html/chapter-04-3.html (2021).
Campanale, C., Massarelli, C., Savino, I., Locaputo, V. & Uricchio, V. F. A detailed review study on potential effects of microplastics and additives of concern on human health. Int. J. Environ. Res. Public Health 17 , 1212 (2020).
Carré, F. et al. in Global Soil Security (eds Field, D. J., Morgan, C.L.S. & McBratney, A. B.) 275–295 (Springer, 2017).
Filippini, T., Wise, L. A. & Vinceti, M. Cadmium exposure and risk of diabetes and prediabetes: a systematic review and dose-response meta-analysis. Environ. Int. 158 , 106920 (2022).
Rahimi Kakavandi, N. et al. An updated systematic review and dose-response meta-analysis on the relation between exposure to arsenic and risk of type 2 diabetes. Toxicol. Lett. 384 , 115–127 (2023).
Hu, X. F., Lowe, M. & Chan, H. M. Mercury exposure, cardiovascular disease, and mortality: a systematic review and dose-response meta-analysis. Environ. Res. 193 , 110538 (2021).
Guo, Y., Lv, Y., Liu, X. & Wang, G. Association between heavy metal mercury in body fluids and tissues and diabetes mellitus: a systematic review and meta-analysis. Ann. Transl. Med. 11 , 114 (2023).
Vena, J. et al. Exposure to dioxin and nonneoplastic mortality in the expanded IARC international cohort study of phenoxy herbicide and chlorophenol production workers and sprayers. Environ. Health Perspect. 106 , 645–653 (1998).
Song, Y. et al. Endocrine-disrupting chemicals, risk of type 2 diabetes, and diabetes-related metabolic traits: a systematic review and meta-analysis. J. Diabetes 8 , 516–532 (2016).
Mattsson, K. et al. Levels of perfluoroalkyl substances and risk of coronary heart disease: findings from a population-based longitudinal study. Environ. Res. 142 , 148–154 (2015).
Schillemans, T. et al. Per- and polyfluoroalkyl substances and risk of myocardial infarction and stroke: a nested case-control study in Sweden. Environ. Health Perspect. 130 , 37007 (2022).
Winquist, A. & Steenland, K. Modeled PFOA exposure and coronary artery disease, hypertension, and high cholesterol in community and worker cohorts. Environ. Health Perspect. 122 , 1299–1305 (2014).
Gui, S. Y. et al. Association between per- and polyfluoroalkyl substances exposure and risk of diabetes: a systematic review and meta-analysis. J. Expo. Sci. Environ. Epidemiol. 33 , 40–55 (2023).
Fu, X., Xu, J., Zhang, R. & Yu, J. The association between environmental endocrine disruptors and cardiovascular diseases: a systematic review and meta-analysis. Environ. Res. 187 , 109464 (2020).
Zhang, H. et al. Phthalate exposure and risk of diabetes mellitus: implications from a systematic review and meta-analysis. Environ. Res. 204 , 112109 (2022).
Zeng, G., Zhang, Q., Wang, X. & Wu, K. H. Low-level plasticizer exposure and all-cause and cardiovascular disease mortality in the general population. Environ. Health 21 , 32 (2022).
Su, T. C., Hwang, J. J., Sun, C. W. & Wang, S. L. Urinary phthalate metabolites, coronary heart disease, and atherothrombotic markers. Ecotoxicol. Environ. Saf. 173 , 37–44 (2019).
Melzer, D. et al. Urinary bisphenol A concentration and risk of future coronary artery disease in apparently healthy men and women. Circulation 125 , 1482–1490 (2012).
Hwang, S., Lim, J. E., Choi, Y. & Jee, S. H. Bisphenol A exposure and type 2 diabetes mellitus risk: a meta-analysis. BMC Endocr. Disord. 18 , 81 (2018).
Download references
Acknowledgements
T.M. is the principal investigator of the German Center for Cardiovascular Research (DZHK), Partner Site Rhine-Main, Mainz, Germany. O.H. and A.D. received funding from the DZHK. O.H. and A.D. have received vascular biology research grants from the Foundation Heart of Mainz. M.A. was supported by grants from the National Institute of Environmental Health Sciences (R01ES07331 and R01ES10563). All the authors were supported by the environmental network EXPOHEALTH, funded by the state of Rhineland-Palatinate, Germany.
Author information
Authors and affiliations.
University Medical Center Mainz, Department of Cardiology, Johannes Gutenberg University Mainz, Mainz, Germany
Thomas Münzel, Omar Hahad & Andreas Daiber
German Center for Cardiovascular Research (DZHK), Partner Site Rhine-Main, Mainz, Germany
Atmospheric Chemistry Department, Max Planck Institute for Chemistry, Mainz, Germany
Jos Lelieveld
Department of Molecular Pharmacology, Albert Einstein College of Medicine, Bronx, NY, USA
Michael Aschner
Center for Research in Environmental Epidemiology (CREAL), Barcelona, Spain
Mark J. Nieuwenhuijsen
Global Observatory on Planetary Health, Boston College, Boston, MA, USA
Philip J. Landrigan
Centre Scientifique de Monaco, Monaco, Monaco
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Correspondence to Thomas Münzel .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Cardiology thanks Mark Miller, Annette Peters and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Münzel, T., Hahad, O., Lelieveld, J. et al. Soil and water pollution and cardiovascular disease. Nat Rev Cardiol (2024). https://doi.org/10.1038/s41569-024-01068-0
Download citation
Accepted : 30 July 2024
Published : 25 September 2024
DOI : https://doi.org/10.1038/s41569-024-01068-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
COMMENTS
Air pollution is determined as the presence of pollutants in the air in large quantities for long periods. Air pollutants are dispersed particles, hydrocarbons, CO, CO 2, ... At this point, international cooperation in terms of research, development, administration policy, monitoring, and politics is vital for effective pollution control. ...
Air pollution is high on the global agenda and is widely recognised as a threat to both public health and economic progress. The World Health Organization (WHO) estimates that 4.2 million deaths ...
Abstract. Air pollution is a pressing global environmental challenge with far-reaching consequences for human health and well-being. This research paper presents an extensive examination of air ...
Air pollution has wide-ranging and profound impacts on human health and well-being. Poor air quality has been shown to be responsible for over 4 million deaths each year from outdoor pollutants, 2 ...
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders (3), leading to infant mortality or chronic disease in adult age (6). National reports have mentioned the increased risk of morbidity and mortality (1).
The Lancet Commission on pollution and health reported that pollution was responsible for 9 million premature deaths in 2015, making it the world's largest environmental risk factor for disease and premature death. We have now updated this estimate using data from the Global Burden of Diseases, Injuriaes, and Risk Factors Study 2019. We find that pollution remains responsible for approximately ...
Air pollution is a cause of disease for millions around the world and now more than ever urgent action is required to tackle the burden of its impacts. Doing so will not only improve both life ...
Two large bodies of evidence in air pollution research support a rethinking of current practices in evaluating the health effects of air pollution for prevention and policy: In September 2021, the World Health Organization (WHO) substantially reinforced its Air Quality Guidelines for clean air by reducing the recommended annual levels of PM 2.5 from 10 μg/m 3 to 5 μg/m 3 and those of NO 2 ...
The roles of air pollution and climate change in individual-level patient care are increasingly recognized. While air pollution has contributed to morbidity and mortality before these cases, the past 2 years brought the first cases in which individual deaths were officially linked with air pollution: in the death of a 9-year-old girl who suffered from asthma in the United Kingdom in whom ...
Public Health. Particle-based ambient air pollution causes more than 4 million premature deaths each year globally, according to the World Health Organization. The tiniest particles—2.5 microns ...
Despite progress in many countries, air pollution, and especially fine particulate matter air pollution (PM2.5) remains a global health threat: over 6 million premature cardiovascular and respiratory deaths/yr. have been attributed to household and outdoor air pollution. In this viewpoint, we identify present gaps in air pollution monitoring and regulation, and how they could be strengthened ...
MIT researchers demonstrate that over 50 percent of the world's population would still be exposed to PM2.5 concentrations that exceed new air quality guidelines due to the large natural sources of particulate matter — dust, sea salt, and organics from vegetation — that still exist in the atmosphere when anthropogenic emissions are removed from the air.
Despite considerable air pollution prevention and control measures that have been put into practice in recent years, outdoor air pollution remains one of the most important risk factors for health outcomes. To identify the potential research gaps, we conducted a scoping review focused on health outcomes affected by outdoor air pollution across the broad research area. Of the 5759 potentially ...
Air pollution is becoming a major health problem that affects millions of people worldwide. In support of this observation, the World Health Organization estimates that every year, 2.4 million people die because of the effects of air pollution on health. ... Research Report. New York: Columbia University Center for Climate Systems Research and ...
Air pollution contributes to the global burden of disease, with ambient exposure to fine particulate matter of diameters smaller than 2.5 μm (PM 2.5) being identified as the fifth-ranking risk ...
Public concern about plastic in the ocean recently ranked higher than concern about climate change in both Australia and the US (149, 150); while Europeans and Australians regarded plastic pollution as the biggest marine related threat to human health, followed by chemical/oil pollution ; and 88% of citizens across 28 European countries ...
Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to health and increased disease, especially in ...
Русский. Español. New WHO Global Air Quality Guidelines (AQGs) provide clear evidence of the damage air pollution inflicts on human health, at even lower concentrations than previously understood. The guidelines recommend new air quality levels to protect the health of populations, by reducing levels of key air pollutants, some of which ...
A number of air pollutants pose severe health risks and can sometimes be fatal, even in small amounts. Almost 200 of them are regulated by law; some of the most common are mercury, lead, dioxins ...
Most research has been conducted in Asia, particularly China, where air pollution, primarily caused by industrial activity, is a significant concern. The country has consequently increased airborne pollutants in places near Japan, South Korea, and Taiwan, as well as in places as far away as California in the US due to airborne pollutant travel.
Air pollution reduction and climate co-benefits in China's industries. Energy intensity improvement, scale structure adjustment and electrification measures in major industrial sectors can ...
The Air Pollution Policy package assumes for all energy-related emission sources the most effective technical pollution control measures that are currently applied in the world. ... Economic Valuation and Cost of Air Pollution Handbook of Research on Energy and Environmental Finance 4.0, 10.4018/978-1-7998-8210-7.ch011, (278-300)
Based on previous research, human exposure to air pollution may cause oral cancer [35], [36]. However, the results of the association between indoor air pollution and PM 2.5 exposure and oral cancer are inconsistent, which may be caused by diverse study populations, exposure sources, races or ethnicities, nationality, and study designs ...
The Virginia Tech College of Science's J. Mark Sowers Distinguished Lecture Series will host a talk on Thursday, Sept. 26, by Kimberly Prather, a member of the National Academy of Sciences and distinguished professor at the University of California San Diego's Scripps Institute of Oceanography. Prather, of the Department of Chemistry and Biochemistry, has researched how water pollutants ...
Globally, more than 6.5 million people die each year due to air pollution. Exposure to polluted air can inflame cells and increase the risk of chronic diseases, including respiratory illness or cancer.Sensitive groups—such as people with heart or lung disease, asthma, children, and older adults—can be particularly susceptible to poor air quality. ...
The Global Burden of Diseases Study estimates that ambient (outdoor) air pollution of particulate matter and ozone is responsible for nearly 6.7 million premature deaths worldwide in 2019. And the ...
Summary. Despite progress in many countries, air pollution, and especially fine particulate matter air pollution (PM 2.5) remains a global health threat: over 6 million premature cardiovascular and respiratory deaths/yr. have been attributed to household and outdoor air pollution. In this viewpoint, we identify present gaps in air pollution ...
Most air pollution research has focused on assessing the urban landscape effects of pollutants in megacities, little is known about their associations in small- to mid-sized cities. Considering ...
Pollution of soil, water and air is an escalating health hazard worldwide 1.The Lancet Commission on Pollution and Health identified pollution as the leading global environmental cause of disease ...