
Utilization Review Nurse Resume Example for 2024: Free Downloadable Templates
Craft an exceptional Utilization Review Nurse Resume with our online builder. Explore expert example templates tailored for various levels and specialties. Captivate employers with a refined, professional Resume. Secure your ideal job today!
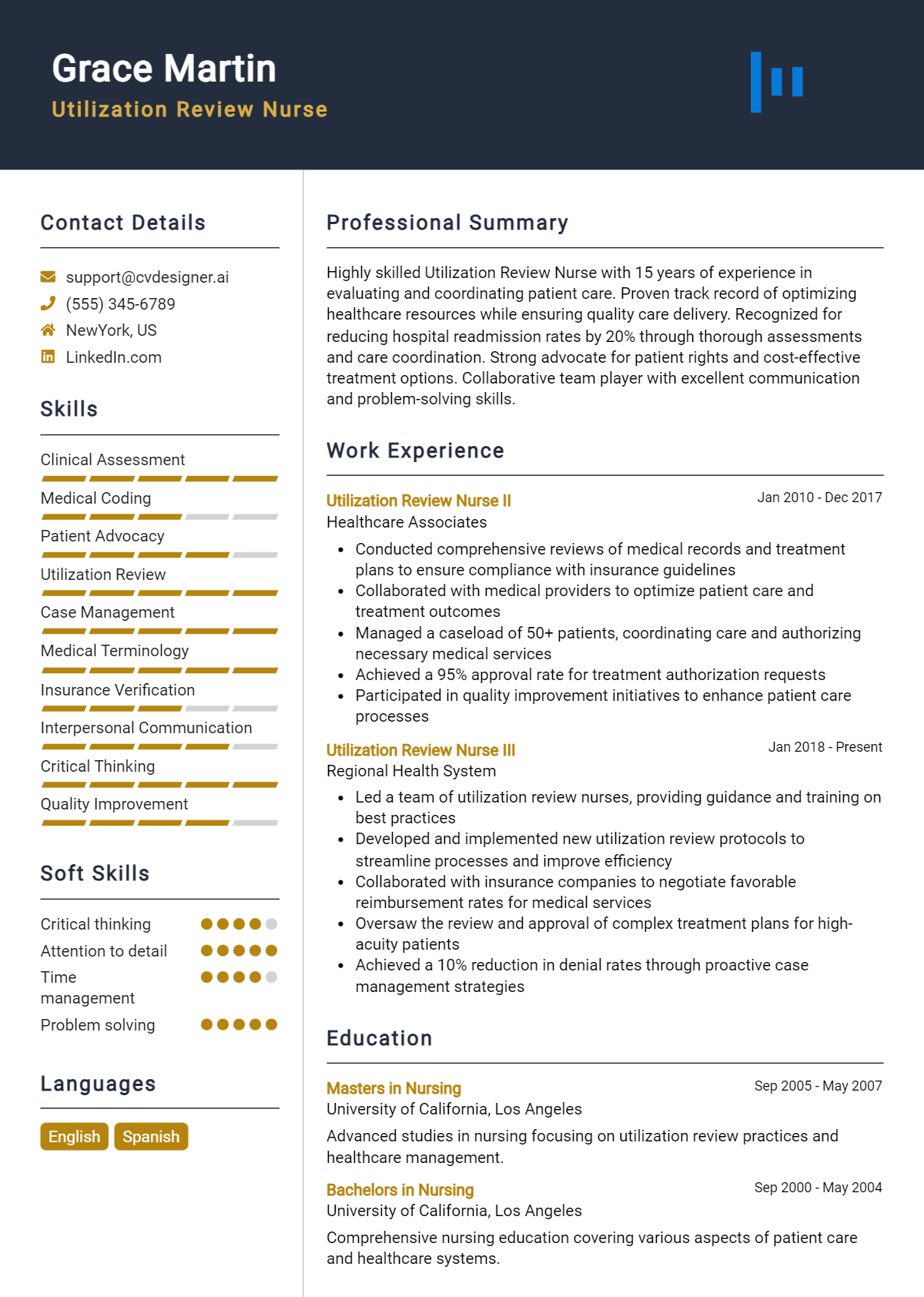
Table of Contents
As the healthcare industry continues to evolve, the role of a Utilization Review Nurse has become increasingly critical in ensuring that patients receive appropriate care while managing costs effectively. This position involves assessing the necessity and efficiency of healthcare services, making it essential for professionals in this field to showcase their expertise and experience through a compelling resume. A well-crafted resume not only highlights your qualifications but also sets you apart in a competitive job market. In this guide, we will walk you through the nuances of writing a standout Utilization Review Nurse resume, providing you with the tools necessary to capture the attention of hiring managers and secure your next position.
Throughout this article, we will cover key points essential for crafting an impactful resume tailored for Utilization Review Nurses. You will learn about the specific responsibilities and skills that should be highlighted, and the best formats to use for maximum effect. We will also discuss common mistakes to avoid that can hinder your chances of landing an interview. Additionally, you’ll find resume examples catering to various levels of experience, along with valuable tips on effective resume writing techniques. Finally, we will guide you in selecting the right resume templates to ensure that your application stands out in the best possible way. Whether you're a seasoned professional or just starting in this field, this comprehensive guide is designed to help you succeed in your job search.
Key Responsibilities and Skills for a Utilization Review Nurse
Utilization Review Nurses play a critical role in the healthcare system by assessing patient care and ensuring that services provided are necessary and appropriate. Their key responsibilities include:
- Conducting evaluations of patient records and treatment plans to determine medical necessity and appropriateness of care.
- Collaborating with healthcare providers, insurance companies, and patients to facilitate effective communication regarding treatment options and coverage.
- Monitoring and analyzing utilization patterns to identify areas for improvement in patient care and resource management.
- Ensuring compliance with healthcare regulations, policies, and standards during the review process.
- Preparing detailed reports and documentation related to utilization review findings and recommendations.
To excel in this role, a Utilization Review Nurse must possess a set of essential skills, including:
- Strong analytical skills to assess patient data and treatment plans effectively.
- Excellent communication skills for liaising with healthcare teams, patients, and insurers.
- Knowledge of healthcare regulations, coding, and billing practices.
- Critical thinking abilities to make informed decisions regarding the necessity of care.
- Proficiency in electronic health records (EHR) systems and utilization review software.
Highlighting these skills effectively in the resume skills section is crucial for showcasing your qualifications to potential employers. Tailoring these responsibilities and skills to match the specific job description will demonstrate your understanding of the role and your suitability for the position. Additionally, consider how these skills can be relevant in crafting a strong CV that reflects your expertise and achievements in utilization review nursing.
Best Resume Format and Structure for a Utilization Review Nurse
When crafting a resume for a Utilization Review Nurse position, it’s essential to choose a format that effectively highlights your qualifications and experience. Here’s a detailed guide on the best resume format and structure to help you stand out:
Contact Information Place your contact information at the top of your resume. This should include:
- Phone Number
- Professional Email Address
- LinkedIn Profile (optional)
- Location (City, State)
Professional Summary Following your contact information, include a concise professional summary. This section should be 2-3 sentences long and summarize your experience, skills, and what you bring to the Utilization Review role. Focus on your nursing background, familiarity with utilization review processes, and any notable achievements.
Work Experience This is one of the critical sections of your resume. List your work experience in reverse chronological order. For each position, include:
- Company Name
- Dates of Employment (Month/Year to Month/Year)
- Bullet points that outline your responsibilities and achievements. Use action verbs and quantify your accomplishments whenever possible. Highlight experiences related to patient care, collaboration with multidisciplinary teams, and any specific utilization review tasks you performed.
Education In this section, provide details of your educational background. Include:
- Degree(s) Earned (e.g., Bachelor of Science in Nursing)
- University/College Name
- Graduation Date (Month/Year)
- Additional relevant coursework or honors can be included if applicable.
Skills Create a section to list your relevant skills. Tailor this to include both hard and soft skills that are pertinent to a Utilization Review Nurse, such as:
- Knowledge of healthcare regulations and compliance
- Proficient in electronic health record (EHR) systems
- Strong analytical and critical thinking abilities
- Effective communication and interpersonal skills
- Ability to work collaboratively with healthcare teams
Certifications List any relevant certifications that enhance your qualifications. This may include:
- Registered Nurse (RN) License
- Certified Case Manager (CCM)
- Utilization Review Certification (URAC)
- Other relevant certifications (if applicable)
Additional Tips
- Choose the Right Format: A chronological resume format is often best for showcasing your work history and progression in the nursing field. However, if you are changing careers or have gaps in your employment, consider a functional or combination format.
- Tailor Your Content: Customize your resume for each job application by using keywords from the job description. This not only helps in passing applicant tracking systems but also shows your alignment with the specific role.
- Keep It Concise: Aim for a one-page resume, especially if you have less than 10 years of experience. If you have extensive experience, you can extend to two pages but ensure every entry is relevant.
The format you choose for your resume can complement your cover letter format as well. A clean, professional design for both documents creates a cohesive application package. Ensure that both your resume and cover letter share similar fonts, colors, and styling to present a unified professional image. Use your cover letter to elaborate on your experiences mentioned in the resume, providing context and demonstrating your enthusiasm for the Utilization Review Nurse position.
By following this structured approach, you will create an impactful resume that effectively communicates your qualifications and readiness for a Utilization Review Nurse role.
Writing Tips and Best Practices for a Utilization Review Nurse Resume
When crafting a resume as a Utilization Review Nurse, it's essential to showcase your clinical expertise, analytical skills, and knowledge of healthcare regulations in a clear and professional format. Start by tailoring your resume to the specific job you're applying for, emphasizing relevant experience and skills that align with the job description. Incorporate strong action verbs to convey your responsibilities and achievements effectively. Additionally, quantifying your accomplishments can provide potential employers with a clearer picture of your capabilities and contributions. Remember to use industry-specific keywords that reflect the terminology and nuances of the Utilization Review field. For a polished presentation, refer to resume writing tips that can elevate your document's professionalism. Finally, consider how these best practices can also enhance your cover letter by making it more compelling and aligned with the job requirements.
- Use action verbs like "analyzed," "managed," "coordinated," and "evaluated" to start bullet points and demonstrate your active role in previous positions.
- Quantify your achievements, such as the percentage of claims approved or the number of patient evaluations conducted, to provide measurable impact.
- Incorporate relevant industry-specific keywords such as "utilization review," "clinical guidelines," "case management," and "healthcare compliance" to pass through applicant tracking systems.
- Highlight your familiarity with medical coding and billing processes, as this is often crucial in utilization review roles.
- Tailor your skills section to reflect both hard skills (like data analysis) and soft skills (like communication and collaboration) that are essential for the role.
- Keep your resume concise, ideally one page, focusing on the most relevant experiences from your nursing career.
- Ensure the format is clean and easy to read, with consistent fonts and spacing to create a professional appearance.
- Proofread your resume multiple times to eliminate any grammatical errors or typos, as attention to detail is vital in the healthcare field.

Common Mistakes to Avoid in a Utilization Review Nurse Resume
Crafting a compelling resume as a Utilization Review Nurse is crucial for standing out in a competitive job market. However, many candidates make common mistakes that can undermine their chances of landing an interview. Awareness of these pitfalls can significantly enhance the effectiveness of your resume. Here are some key mistakes to avoid:
- Overloading your resume with excessive information, making it cluttered and hard to read.
- Using generic descriptions that fail to highlight specific skills and achievements relevant to utilization review.
- Neglecting to tailor your resume for the specific job you are applying for, which can make it appear less relevant.
- Failing to quantify accomplishments, such as the number of reviews completed or improvements in patient care metrics.
- Ignoring the importance of clear formatting, which can lead to a lack of professionalism.
- Including outdated certifications or failing to mention current relevant credentials.
- Misstating your job titles or responsibilities, which can be easily verified by potential employers.
- Using passive language instead of strong action verbs, which can make your contributions seem less impactful.
- Overlooking the importance of proofreading for typos and grammatical errors that can detract from your professionalism.
- Not including keywords from the job description that can help your resume get past applicant tracking systems.
To further enhance your job application, consider reviewing the common mistakes to avoid in a resume . Additionally, pay attention to common cover letter mistakes that should also be avoided to ensure a cohesive and compelling application package.
Sample Utilization Review Nurse Resumes
A well-crafted resume is essential for showcasing your qualifications as a Utilization Review Nurse. Whether you're an experienced professional, an entry-level candidate, or transitioning from a different career, having a tailored resume can significantly impact your job search. Below are three sample resumes to guide you in creating your own.
Experienced Utilization Review Nurse
Jane Doe, RN, BSN 123 Health St. City, State, Zip (123) 456-7890 [email protected]
Professional Summary Dedicated and detail-oriented Utilization Review Nurse with over 8 years of experience in healthcare. Proven track record of conducting thorough patient assessments, reviewing medical records, and ensuring compliance with healthcare policies. Expertise in collaborating with healthcare teams to optimize patient care while managing costs.
Core Competencies
- Utilization Review
- Patient Advocacy
- Healthcare Policy Compliance
- Medical Record Review
- Interdisciplinary Collaboration
- Quality Assurance
Professional Experience Utilization Review Nurse ABC Health Services, City, State March 2018 – Present
- Conduct comprehensive reviews of patient care plans to ensure compliance with insurance policies and regulations.
- Collaborate with physicians and healthcare providers to develop cost-effective treatment plans.
- Implement quality assurance measures that improved patient outcomes by 15% over two years.
- Train and mentor junior nurses on best practices in utilization review and documentation.
Staff Nurse XYZ Hospital, City, State June 2015 – March 2018
- Provided direct patient care in a fast-paced environment, managing a caseload of 10 patients daily.
- Assisted in developing patient discharge plans and coordinated with community resources for post-hospital care.
- Participated in patient education initiatives, enhancing patient understanding of treatment options.
Education Bachelor of Science in Nursing (BSN) University of State, City, State Graduated: May 2015
Certifications
- Registered Nurse (RN)
Entry-Level Utilization Review Nurse
John Smith, RN 456 Care Ave. City, State, Zip (987) 654-3210 [email protected]
Professional Summary Motivated and compassionate recent nursing graduate with a solid foundation in patient care and a keen interest in utilization review. Eager to leverage clinical skills and knowledge of healthcare regulations to ensure optimal patient outcomes and resource utilization.
- Patient Assessment
- Medical Terminology
- Clinical Documentation
- Critical Thinking
- Team Collaboration
- Time Management
Professional Experience Nursing Intern LMN Medical Center, City, State January 2023 – May 2023
- Assisted nursing staff in assessing patients and developing care plans under supervision.
- Participated in interdisciplinary team meetings to discuss patient care strategies.
- Conducted patient education sessions on medication adherence and discharge instructions.
Volunteer Nurse Health Outreach Program, City, State June 2022 – August 2022
- Provided nursing care and support for underserved populations during community health initiatives.
- Collected health data and assisted in the documentation of patient information.
Education Bachelor of Science in Nursing (BSN) University of State, City, State Graduated: May 2023
Career Changer to Utilization Review Nurse
Emily Johnson 789 Wellness Blvd. City, State, Zip (321) 654-9870 [email protected]
Professional Summary Results-driven healthcare professional transitioning to a Utilization Review Nurse role with a background in healthcare administration and a passion for patient advocacy. Strong analytical skills and experience in managing healthcare processes, seeking to ensure efficient resource utilization and high-quality patient care.
- Healthcare Administration
- Data Analysis
- Cost Management
- Policy Development
- Communication Skills
- Project Management
Professional Experience Healthcare Administrator PQR Hospital, City, State June 2019 – Present
- Managed operational processes, improving efficiency by 20% through streamlined workflows.
- Developed and implemented policies to enhance patient care and compliance with regulatory standards.
- Collaborated with clinical teams to analyze patient data and identify areas for improvement.
Administrative Assistant GHI Medical Group, City, State August 2016 – May 2019
- Supported the healthcare team with patient scheduling, insurance verification, and data entry.
- Assisted in the coordination of patient care services and ensured adherence to organizational policies.
Education Master of Health Administration (MHA) University of State, City, State Graduated: May 2019
- Certified Healthcare Administrative Professional (cHAP)
For further inspiration, explore more resume templates . Additionally, corresponding cover letter examples can help you create a complete job application package.
Checklist for a Utilization Review Nurse Resume
- Proofread for Typos and Errors: Carefully review your resume for any spelling, grammar, or punctuation mistakes. Consider reading it aloud or asking a friend to review it for a fresh perspective.
- Check for Consistency: Ensure that your formatting is uniform throughout the document. This includes font size, bullet points, and spacing. Consistency enhances readability.
- Tailor to the Job Description: Customize your resume for each application by incorporating relevant keywords and phrases from the job description. This shows that you are a good fit for the specific role.
- Highlight Relevant Experience: Focus on your experience related to utilization review, including specific achievements, metrics, and responsibilities that align with the job requirements.
- Include Relevant Certifications: Make sure to list any nursing licenses, certifications, or training that are pertinent to utilization review, such as Certified Utilization Review Nurse (CURN).
- Quantify Achievements: Whenever possible, use numbers to quantify your achievements (e.g., "Reviewed and approved 200+ patient cases monthly, achieving a 95% accuracy rate").
- Professional Summary: Write a compelling professional summary that encapsulates your skills, experience, and what you bring to the role. This should be tailored to highlight your strengths in utilization review.
- Contact Information: Ensure your contact information is correct and up to date, including your phone number, email address, and LinkedIn profile if applicable.
- Use an AI Resume Builder: Consider using an AI resume builder to ensure that all elements are well-organized and visually appealing, making it easier for recruiters to read.
- Adapt for CV or Cover Letter: Remember that a similar checklist can be followed for creating a CV or cover letter , ensuring consistency and professionalism across all your application materials.
Key Takeaways for a Utilization Review Nurse Resume Guide
As you embark on the journey to create an impactful Utilization Review Nurse resume, remember that the examples and tips provided are your stepping stones to success. By tailoring your resume to highlight your clinical expertise, analytical skills, and understanding of healthcare policies, you’ll be well-equipped to stand out in a competitive job market. To further enhance your application, consider downloading a tailored resume template from resume templates or a professional cover letter template from cover letter templates . For a more personalized approach, explore our best resume maker to craft a resume that reflects your unique qualifications. Additionally, following similar guidelines will assist you in creating a compelling CV and an engaging cover letter . Take these next steps to ensure your application stands out and showcases your strengths as a Utilization Review Nurse.
Build your Resume in minutes
Use an AI-powered resume builder and have your resume done in 5 minutes. Just select your template and our software will guide you through the process.
Make a cv in minutes
Pick your template, fill in a few details, and our builder will do the rest.
