

Research Horizons: 6 Best Research Opportunities for Medical Students in Kenya
- Post author: kenyamedexams
- Post published: December 8, 2023
- Post category: Uncategorized
Research Opportunities : Research is the cornerstone of medical advancement, a crucial avenue for expanding knowledge and improving healthcare outcomes. In Kenya, a burgeoning hub of medical education, the landscape is ripe with opportunities for aspiring medical students to engage in impactful research initiatives. These opportunities not only enrich the educational experience but also contribute significantly to the country’s healthcare system. In this exploration of research horizons, we shed light on the myriad avenues available to medical students in Kenya, fostering a culture of inquiry and innovation.
Exploring the Landscape of Research Opportunities

Building Bridges: Collaboration in Research
Collaboration is a linchpin in the world of research, and medical students in Kenya have the opportunity to build bridges between academia and healthcare practice. Partnering with experienced researchers, clinicians, and public health professionals, students can access a wealth of knowledge and resources. Through interdisciplinary collaboration, medical students can contribute to holistic solutions for healthcare challenges. This interconnected approach fosters an environment where different perspectives converge, leading to innovative breakthroughs. Moreover, collaborative projects often extend beyond national borders, providing students with a global perspective on healthcare challenges and solutions.
The Role of Technology in Medical Research
In the contemporary landscape, technology plays a pivotal role in medical research. Embracing cutting-edge tools and methodologies, medical students in Kenya can spearhead research projects that leverage the power of artificial intelligence, data analytics, and telemedicine. Whether it’s streamlining patient data for better diagnostics or utilizing mobile health applications for community outreach, technology opens new vistas for research. This intersection of medicine and technology not only enhances the efficiency of healthcare delivery but also equips students with skills that are increasingly relevant in the evolving field of medicine.
Challenges and Opportunities in Rural Healthcare Research
While urban centers often take the spotlight in medical research, rural healthcare presents a unique arena for exploration. Medical students in Kenya have the chance to investigate the challenges and opportunities specific to rural communities. From understanding the impact of geographical barriers on healthcare access to exploring innovative solutions for telemedicine in remote areas, rural healthcare research addresses critical gaps in the medical landscape. By immersing themselves in the rural context, students can contribute to the development of tailored interventions that address the distinct healthcare needs of these underserved populations.
Ethical Considerations in Medical Research
As stewards of public health, medical students must navigate the complex terrain of ethical considerations in their research endeavors. Kenya, like any other country, requires a rigorous adherence to ethical standards to ensure the welfare of research participants and the integrity of the findings. Whether it’s obtaining informed consent, safeguarding confidentiality, or addressing cultural sensitivities, ethical considerations are paramount. Engaging in research provides medical students with an opportunity to grapple with these ethical challenges firsthand, instilling a sense of responsibility and integrity that will guide them throughout their careers.
Fostering a Culture of Inquiry: Research in Medical Education
Beyond the confines of specific research projects, the integration of research into medical education itself is a transformative force. Medical students in Kenya have the chance to be part of institutions that prioritize a culture of inquiry. Incorporating research into the curriculum empowers students to develop critical thinking skills, cultivate a questioning mindset, and appreciate the iterative nature of scientific inquiry. By emphasizing the importance of research in medical education, Kenya lays the foundation for a generation of healthcare professionals who are not just practitioners but also contributors to the evolving body of medical knowledge.
Conclusion: Nurturing the Seeds of Research for a Healthier Tomorrow
In conclusion, the landscape of research opportunities for medical students in Kenya is expansive and filled with promise. As the country grapples with diverse healthcare challenges, the role of medical students in shaping the future of healthcare through research cannot be overstated. Whether through collaborative efforts, leveraging technology, addressing rural healthcare disparities, navigating ethical considerations, or integrating research into education, the potential for impact is immense. By seizing these opportunities, medical students in Kenya not only enhance their own educational journey but contribute significantly to the advancement of healthcare in the nation and beyond. As they embark on this research odyssey, they are not merely students; they are architects of a healthier tomorrow.
Please Share This Share this content
- Opens in a new window
You Might Also Like

Residency Tips: 6 Best ways to Navigate the Path After Medical School for Kenyan Graduates

Striking the Balance: 6 Top Guides for Medical Students on Best Ways of Balancing Academics and Extracurriculars in Kenya

Healthcare Technology in Kenya: Exploring 6 Best Advances in Medical Innovations

- Address St. Mary’s Mission Hospital, Lang'ata, Nairobi, Kenya
- any question: +254 720999920
- Appointment
Pioneering Clinical Trials and Healthcare Research in Kenya
At CliniQuest Research Site, we are dedicated to improving the future of healthcare through groundbreaking clinical trials and in-depth healthcare research in Kenya. Our state-of-the-art facility is committed to developing innovative solutions that address the unique health challenges faced by Kenyans. Join us as we transform the medical landscape and enhance patient care nationwide.

Dr. Karen Kiranka
Happy patients.
Our Mission
Our mission is to conduct high-quality clinical trials and healthcare research that contribute significantly to global medical knowledge while focusing on the specific needs of the Kenyan population.
We aim to bridge the gap between cutting-edge medical innovations and the people who need them most, ensuring that advancements in healthcare are accessible and relevant to our communities.
Join us on a journey of discovery and progress, where each clinical trial brings us closer to a healthier future for all Kenyans.
- About CliniQuest Resaerch
Comprehensive Clinical Trial Services at CliniQuest Research, Kenya
CliniQuest Research offers a comprehensive suite of services designed to facilitate cutting-edge clinical trials and healthcare research in Kenya. Our expertise spans various therapeutic areas, and we are dedicated to providing high-quality, ethical research services that contribute to global health advancements. Explore our core services below:

Clinical Trial Management
Consulting services.

Custom Research Solutions

Data Management and Biostatistics
Laboratory services.

Patient Recruitment and Retention
Pharmacovigilance, regulatory affairs and compliance.

Training and Education
Why choose cliniquest research.
Elevating Healthcare Through Ethical Innovation and Collaboration
Unmatched Expertise in Local and Global Health Dynamics
At CliniQuest Research site, we blend deep local insights with global health expertise, positioning us uniquely to tackle the health challenges prevalent in Kenya and beyond. Our team comprises renowned specialists and researchers who bring a wealth of knowledge and experience to every clinical trial, ensuring that our studies are both globally relevant and locally impactful.
Patient-Centric Research Approach
Our commitment to the safety, dignity, and well-being of our participants stands at the core of our operations. CliniQuest Research adopts a patient-centric approach, ensuring that every clinical trial is conducted with the highest ethical standards, respect, and transparency. We prioritize informed consent and continuous communication, making participants active partners in our research journey.
Strategic Partnerships for Comprehensive Solutions
Collaboration is key to our success. CliniQuest Research has forged strong alliances with international healthcare leaders, local institutions, and community organizations. These partnerships allow us to leverage collective expertise, resources, and insights, ensuring that our research findings are translated into practical and sustainable healthcare solutions for the communities we serve.
Innovative Research for Tangible Impact
Innovation drives us forward. We are committed to exploring new frontiers in medical research, employing state-of-the-art technologies and methodologies in our clinical trials. Our work is aimed at not only advancing scientific knowledge but also developing real-world solutions that address the unmet health needs of our population.
Commitment to Empowerment through Education
Knowledge is power. CliniQuest Research believes in the importance of empowering individuals, healthcare providers, and the wider community with up-to-date information about medical research and healthcare advancements. Through educational programs, workshops, and public engagement initiatives, we strive to build a well-informed and health-literate society.
Our Promise of Integrity and Excellence
Integrity and excellence are the cornerstones of our work. At CliniQuest Research, we are dedicated to conducting our trials and research activities with the utmost honesty, accuracy, and professionalism. Our promise is to uphold the highest standards of quality and reliability in every aspect of our work, from initial research design to the dissemination of findings.

What are our Therapeutic Areas
CliniQuest Research Site stands out as a beacon of progress in healthcare research at the intersection of innovation and compassion.
Developing vaccines with cutting-edge science to protect against infectious diseases and improve global health.
Targeting sickle cell disease with novel therapies and comprehensive care for improved patient outcomes.

Pioneering diabetes care through breakthrough treatments and comprehensive management strategies for better health

Neglected diseases
Addressing neglected diseases with dedicated research to bring hope and solutions to underserved populations.

Infectious Diseases
Innovating to combat infectious diseases, enhancing global health through groundbreaking research and collaborative efforts.

Diagnostic devices
Revolutionizing patient care with state-of-the-art diagnostic devices for early detection and intervention.
Reproductive health
Advancing reproductive health through research-driven solutions and accessible care for all individuals.

Antimicrobial resistance
Combating antimicrobial resistance with innovative research to develop effective treatments and stewardship strategies.
Bioequivalence and Bioavailability
Ensuring medication safety and efficacy with rigorous bioequivalence and bioavailability studies for better treatments.
Successful Stories
Discover the wide array of clinical trials conducted at CliniQuest Research, ranging from infectious diseases to chronic condition management, from cancer treatments to vaccines, and from cardiology to neurology. Our trials are meticulously designed and executed to meet the highest international standards, ensuring reliable results that can make a real difference in the lives of patients.
Utilization of dried blood spot specimens can expedite nationwide surveillance of HIV drug resistance in resource-limited settings
The Effects on Tuberculosis Treatment Adherence from Utilising Community Health Workers: A Comparison of Selected Rural and Urban Settings in Kenya
Effect of the levonorgestrel intrauterine device on genital HIV-1 RNA shedding among HIV-1–infected women not taking antiretroviral therapy in Nairobi, Kenya
Join Our Research
We invite you to participate in our clinical trials and become part of a movement that’s shaping the future of healthcare in Kenya. Whether you’re a potential trial participant, a healthcare provider, or a researcher, your involvement is vital to our success. By contributing to our studies, you’re playing a role in the development of new treatments and the improvement of health outcomes for generations to come.

24 / 7 HOURS SERVICE
Make an Appoinment
Select Department Clinical Trial Management Patient Recruitment And Retention Laboratory Services Data Management And Biostatistics Pharmacovigilance Regulatory Affairs And Compliance Custom Research Solutions Training And Education Counseling
Choose Doctor by Name Dr. Christina Mwachari Dr. Karin Kiranka Dr. John Heshmat Dr. Videlis Nduba
Our Latest News

Upholding Ethical Standards in Clinical Trials: CliniQuest Research Site’s Commitment in Kenya
In the quest for medical advancements, ethical integrity forms the backbone of credible clinical research. At CliniQuest Research, we’re pioneering ethical clinical trials in Kenya, setting new standards for patient safety and research integrity. Our commitment goes beyond regulatory compliance,…

Navigating Clinical Trial Management in Kenya: Challenges and Triumphs
Diving into the heart of Kenya’s healthcare research landscape, CliniQuest Research stands at the forefront, navigating the intricate world of clinical trial management. Faced with unique challenges from regulatory hurdles to infrastructure constraints, we’re crafting innovative solutions that are transforming…

Empowering Healthcare Innovations: CliniQuest Research Site’s Approach to Patient Recruitment
In the quest to revolutionize healthcare through clinical trials, CliniQuest Research is redefining patient recruitment in Kenya. Through innovative strategies and a deep understanding of the local community, we are breaking down barriers and engaging participants in meaningful ways. This…


+254 709 983000/ +254 709 983676
- Our History
- Our Policies
- Partnerships and Collaborators
MAJOR RESEARCH THEMES
Research platforms, scientific departments, policy briefs, publications.
- Capacity Strengthening
- Data Access

The Programme
- Major Research Themes
- Research Platforms
- Scientific Departments
Quick Links
- Procurement

The KEMRI Wellcome Trust Research Programme is a
world-renowned health research unit of excellence. The programme was formed in 1989 when the Kenya Medical Research Institute formed a partnership with the Wellcome Trust and the University of Oxford. The Programme has grown from a small group of 12 to a state of the art facility hosting over 100 research scientists and 700 support staff working across Kenya, Uganda and the region. We have over the years excelled in use of novel ideas working with local community’s to achieve better health for Africa while also developing African scientific leaders.
Executive Director KWTRP
A mixed methods study examining the impact of primary health care financing transitions on facility functioning and service delivery in Kenya: a study protocol - 2024
Examining the development and utilisation of community-based health information systems (cbhis) in africa: a scoping review - 2024, the impact of covid-19 on people with epilepsy: global results from the coronavirus and epilepsy study - 2024.
- Adopting the EEEC Framework to optimize critical provision in Kenya
- Final copy Summary of research findings by The CHAIN Network and KEMRI-Wellcome Trust
- Improving case detection of tuberculosis in hospitalised Kenyan children
- Using ‘Magnet Theatre’ to engage public audiences with health research in coastal Kenya

Revolutionizing Care: Advancements in Sickle Cell Disease Research

KWTRP exhibits at the Kenya National Research Festival 2024
Dissemination Workshop for the Kenya Multi-site Integrated Serosurveillance (KEMIS) Project

KWTRP 2023 Annual Report
World- Leading COVID-19 Vacciine Research

Frequently Asked Questions .
The KEMRI Wellcome Trust Research Programme (KWTRP) is based within the KEMRI Centre for Geographic Medical Research – (Coast). Our core activities are funded by the Wellcome Trust.
KEMRI stands for Kenya Medical Research Institute and is a government institution, under the Ministry of Health, (MOH). It was established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and Innovation Act 2013. The 1979 Act established KEMRI as a National body responsible for carrying out health research in Kenya. There are 12 KEMRI research centres in Kenya. Eight are in Nairobi while the other centres are in Kilifi, Kisumu, Kericho and Busia. The centre in Kilifi is called the Centre for Geographic Medicine Research, Coast (CGMR-C) and also known us the KEMRI-Wellcome Trust Research Programme (KWTRP) due to the funding received from the Wellcome Trust see more
Conducting high quality research requires resources, including equipment, vehicles, drugs and highly qualified staff. As such, KEMRI Kilifi works with several international organisations that fund most of the ongoing research projects. In Kilifi, the main funding partner is a charitable UK-based organisation called Wellcome Trust. This is why the research programme in Kilifi is called the KEMRI-Wellcome Trust Research Programme.
The first large research project at KEMRI Kilifi in 1989 looked at the problem of malaria. In Kenya, malaria is very common in the Coast, Nyanza, Rift Valley and Western parts of Kenya. From these possible sites, Kilifi was chosen because KEMRI already had some experience of running smaller research projects with the Wellcome Trust at Kilifi County Hospital (former Kilifi District Hospital), in addition to having a stable population i.e. minimal movement in and out of Kilifi was important to the studies.
Currently, KWTRP has 3 main hubs in Kilifi, Nairobi and Mbale, but also works in collaborations with researchers in Harar in Ethiopia and Bagamoyo in Tanzania. In Kilifi the Programme conducts research in Kilifi County Hospital and nearby health facilities, such as Pingilikani, Ngerenya, Junju, Ganze Health Centre, Bamba sub county hospital, Dida, Madamani dispensaries, Mtwapa among others. The programme also hosts a comprehensive Health demographic surveillance system where KWTRP staff visit people in their homes and collects population-based data which is then used to support research work. The Programme has also established a clinical surveillance network with 17 hospitals across Kenya. This network collects routine hospital admission data that is used for decision making and for researchers. The hospital in the network include Coast General Hospital in Mombasa, Mbagathi, Machakos, Pumwani Hospitals in Nairobi etc. KEMRI Kilifi also works in other parts of Kenya and in other countries in Africa such as Mbale, Uganda.
Need directly help! Please feel free to contact us
Our Subsites

Our Gallery

Articles on Kenyan health
Displaying all articles.

Suffering in silence: how Kenyan women live with profound childbirth injuries
Kathomi Gatwiri , Southern Cross University

Why Kenya isn’t winning the war against malaria in some counties
Eunice Anyango Owino , University of Nairobi

Why shared toilets in informal settlements may pose a serious health risk
Sheillah Simiyu , Great Lakes University of Kisumu

Why Kenya needs policies to tackle dengue and chikungunya viruses

Kenya is paying a heavy human and financial cost for unsafe abortions
Estelle Monique Sidze , African Population and Health Research Center

The Kenyan doctors’ strike is over, but there’s a lot of unfinished business
Moses Masika , University of Nairobi

Kenyans and Ugandans need to change their ways to arrest lifestyle diseases
Catherine Kyobutungi , African Population and Health Research Center

Better maternity leave laws are needed to protect African mothers
Elizabeth Kimani-Murage , Brown University

Why Nairobi must spread the right food message in an unhealthy environment
Samuel Oti , University of the Witwatersrand

Lessons other countries can learn from Kenya’s ambitious nutrition plan
Elizabeth Kimani-Murage , African Population and Health Research Center
Related Topics
- Exclusive breastfeeding
- Global perspectives
- Maternal health
- Non-communicable diseases
- Public health
- World Health Organization (WHO)
Top contributors
Medical Entomologist at the School of Biological Sciences, University of Nairobi
Senior Research Scientist, African Population and Health Research Center
Tutorial Fellow, School of Medicine, University of Nairobi, University of Nairobi
Associate professor, Southern Cross University
Executive Director, African Population and Health Research Center
Research scientist, African Population and Health Research Center
Millennium Promise Fellow and Senior Research Officer, African Population and Health Research Center
Lecturer, Great Lakes University of Kisumu
Policy Outreach Manager , African Population and Health Research Center
- X (Twitter)
- Unfollow topic Follow topic
- Telephone: +254 020 2132279
- Email: [email protected]
- Office Address: Upper Hill - Lower Duplex Suite 19
Health Research Kenya - Our business is to protect you
Our business is to protect you, health, research and information technology.
The Health and Workforce Training & Research Kenya (HETARK) is a Non-Governmental Organization registered and operating in Kenya since 2008, focused on health systems strengthening projects in Africa.
Our vision is to transform health service delivery by promoting health research and information technology innovations, while our mission is to implement sustainable interventions that strengthen health systems in Africa.
KNOW ABOUT THE COMPANY
OUR SERVICES

Digital Solutions
We deliver business applications and comprehensive web solutions for social impact & Research Technologies

Survey & Data Collection
Comprehensive data gathered from a target audience about a specific topic to conduct research.

Design & Implementation
Our policy development approach is customer-centric and tailored to the clients’ needs.

Capacity Building
We obtain and retain the skills, knowledge and other resources needed to do our jobs competently.
WHY CHOOSE HETARK
Our vision is to transform health service delivery by promoting health research and information technology innovations.
Our mission is to implement sustainable interventions that strengthen health systems in Africa.
This site uses cookies to collect activity data and personalize content. By continuing to navigate this site, you agree to allow us to collect information using cookies. Learn more about how we care for your data in our privacy notice .
Kenya launches first policy aligning research investment with national priorities
October 7, 2019 by Douglas Waudo
A potential game-changer for health research in Kenya—the government has launched a new policy framework to guide alignment of research priorities with the country’s health challenges.

Kenyan Cabinet Secretary for Health Sicily K. Kariuki (left) visits with PATH staff at the Kenya Health Forum 2019. She holds the Research for Health Priorities and Research for Health Policy documents, which she later launched. Photo: PATH/Douglas Waudo.
Although a number of Kenyan policies address research and development for health—both directly and indirectly—the country had previously lacked an overarching national policy framework to effectively coordinate, prioritize, promote, and regulate the conduct of research for health activities. Health research was scattered across various institutions without a clear framework for coordination. But during the Kenya Health Forum in August 2019, Cabinet Secretary for Health Sicily Kariuki changed that when she launched the Research for Health Policy Framework and the accompanying Research for Health Priorities.

The Research for Health Policy Framework is Kenya's first all-inclusive policy governing investment and coordination of health research. Photo: PATH/Douglas Waudo.
The launch marks a turning point in Kenya’s efforts for health research agenda setting. The Research for Health Policy Framework is the country’s first all-inclusive policy and will provide much-needed prioritization for investment, integration, and coordination of health research.
“PATH commends the government for its commitment to seeing the policy through to completion, and has been grateful for the opportunity to partner with the Ministry of Health over the past two and a half years to complete this important policy,” said Rosemarie Muganda, PATH’s regional director for advocacy and public policy.
The policy reflects a number of priorities that PATH has advocated for in Kenya, including increased investment in health research and development, evidence-informed policy change and implementation, and a streamlined regulatory system as an essential part of achieving UHC.
The policy is vital to Kenya’s progress toward global and national goals—particularly its commitment to achieving universal health coverage (UHC) in the next five years, which President Uhuru Kenyatta has committed to achieving before leaving office under his “Big Four Agenda.”
The policy reflects a number of priorities that PATH has advocated for in Kenya , including increased investment in health research and development, evidence-informed policy change and implementation, and a streamlined regulatory system as an essential part of achieving UHC. The policy also outlines key priorities and structures for health research agenda setting, as well as directs the government to support testing on the scale-up of innovations to inform policies that address barriers to access.

Kenyan Cabinet Secretary for Health, Sicily K. Kariuki, launches the Research for Health Policy at the Kenya Health Forum 2019. Photo: PATH/Douglas Waudo.
The policy will nurture innovation for the benefit of Kenyans. It will also clarify the roles and functions of national and county health sectors as they deliver an effective research-for-health ecosystem, and will define norms and standards for health research. To make sure it is implemented effectively, the policy also provides guidance for sustainable financing and monitoring and evaluation of its impact.
“For UHC to succeed in Kenya, we must invest in all the health building blocks. Key amongst them are human resources and health products and technologies.”
PATH advocates will continue to monitor the Research for Health Policy Framework and the Research for Health Priorities to ensure they are fully implemented, delivering on their potential to bring a new era of health research and development in Kenya. Through partnership, evidence generation, and accountability measures, PATH is committed to elevate this common message and to ensure that health research and development is prioritized as a means of growing Kenya’s economy and improving quality of life for all its people.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Trop Med Hyg
- v.107(4 Suppl); 2022 Oct

Enhancing Malaria Research, Surveillance, and Control in Endemic Areas of Kenya and Ethiopia
John i. githure.
1 Tom Mboya University College, Homa Bay, Kenya;
Delenasaw Yewhalaw
2 Department of Medical Laboratory Sciences, Institute of Health, Jimma University, Jimma, Ethiopia;
3 Tropical and Infectious Diseases Research Center, Jimma University, Jimma, Ethiopia;
Harrysone Atieli
4 School of Public Health and Community Development, Maseno University, Kisumu, Kenya;
Elizabeth Hemming-Schroeder
5 Center for Global Health & Diseases, Case Western Reserve University, Cleveland, Ohio;
Ming-Chieh Lee
6 Program in Public Health, University of California at Irvine, Irvine, California;
Xiaoming Wang
Daibin zhong, christopher l. king, arlene dent, wolfgang richard mukabana.
7 Department of Biology, University of Nairobi, Nairobi, Kenya;
Teshome Degefa
8 Center for Hydrometeorology and Remote Sensing, Department of Civil and Environmental Engineering, University of California at Irvine, Irvine, California;
Andrew K. Githeko
9 Centre for Global Health Research, Kenya Medical Research Institute, Kisumu, Kenya;
Gordon Okomo
10 Ministry of Health, Homa Bay County, Homa Bay, Kenya;
Lilyana Dayo
11 Ministry of Health, Kisumu County, Kisumu, Kenya;
Kora Tushune
12 Department of Health Management and Policy, Faculty of Public Health, Jimma University, Jimma, Ethiopia;
Charles O. Omondi
Hiwot s. taffese.
13 National Malaria Program, Federal Ministry of Health, Addis Ababa, Ethiopia
James W. Kazura
Malaria control programs in Africa encounter daunting challenges that hinder progressive steps toward elimination of the disease. These challenges include widespread insecticide resistance in mosquito vectors, increasing outdoor malaria transmission, lack of vector surveillance and control tools suitable for outdoor biting vectors, weakness in malaria surveillance, and an inadequate number of skilled healthcare personnel. Ecological and epidemiological changes induced by environmental modifications resulting from water resource development projects pose additional barriers to malaria control. Cognizant of these challenges, our International Center of Excellence for Malaria Research (ICEMR) works in close collaboration with relevant government ministries and agencies to align its research efforts with the objectives and strategies of the national malaria control and elimination programs for the benefit of local communities. Our overall goal is to assess the impact of water resource development projects, shifting agricultural practices, and vector interventions on Plasmodium falciparum and P. vivax malaria in Kenya and Ethiopia. From 2017 to date, the ICEMR has advanced knowledge of malaria epidemiology, transmission, immunology, and pathogenesis, and developed tools to enhance vector surveillance and control, improved clinical malaria surveillance and diagnostic methods, and strengthened the capacity of local healthcare providers. Research findings from the ICEMR will inform health policy and strategic planning by ministries of health in their quest to sustain malaria control and achieve elimination goals.
INTRODUCTION
Malaria remains a significant public health concern in Kenya and Ethiopia. Three-quarters of the 48 million residents of Kenya and 52% of the 103 million residents of Ethiopia are at risk of malaria. 1 , 2 Despite major progress in malaria control in the past two decades, malaria burden remains high in these two countries. For example, in 2020, there were an estimated 2.7 million and 4.2 million malaria cases in Kenya and Ethiopia, respectively. 3 Malaria control strategies in both countries are deployed according to risk stratification based on routinely collected malaria case data from health facilities or from entomological surveillance. 1 , 2 For example, Kenya is stratified into four epidemiological zones on the basis of malaria endemicity: Lake and Coastal endemic zones, where transmission is high throughout the year; seasonal transmission zones in arid and semiarid areas in Northern and Southeastern parts of the country, where there is a short period of intense transmission during the rainy season; malaria epidemic-prone areas of Western highlands; and a low-risk area in the central Kenyan highlands. 2 Indoor residual spraying (IRS) of insecticides and intermittent presumptive treatment in pregnancy (IPTp) are added to the standard vector control intervention, long-lasting insecticidal-treated nets (LLINs). 4 Similarly, Ethiopia is stratified into five broad strata according to annual parasite incidence: malaria-free, very low, low, moderate, and high transmission. Vector control methods are adjusted according to malaria risk strata. 5
Kenya’s 2019–2023 Malaria Strategy aims to reduce the incidence and deaths due to malaria by 75% of 2016 levels by 2023 and to establish systems for malaria elimination in selected low-transmission counties. 2 The 2020–2025 Ethiopian National Malaria Strategic Plan aims to reduce malaria morbidity and mortality by 50% from the 2020 baseline, achieve zero indigenous malaria cases in districts with low incidence, and eliminate malaria in the country by 2030. 5 Achieving these ambitious goals must overcome many challenges. For example, insecticide resistance and outdoor malaria transmission are widely reported across Kenya and Ethiopia. 6 – 8 Human-induced environmental modifications, such as deforestation, urbanization, and water resource development projects further alter vector ecology, malaria transmission dynamics, and disease risk. 9 – 11 Changes in vector ecology and behaviors have limited the utility of currently available vector surveillance tools and the success of the existing first-line vector interventions, LLINs and IRS. 12 Additionally, human migration associated with environmental modifications, natural disasters, or civil conflicts may introduce new parasite clones and drug resistant strains that confound elimination efforts. 13
Increased knowledge of the impact of rapidly changing land use modifications and water resources and intensive malaria control measures on vector biology and malaria epidemiology is required to achieve the goals of national malaria control and elimination. In addition, new tools for surveillance and control of outdoor transmission are needed. Malaria risk is determined by complex interactions among biological factors (e.g., vector behavior, insecticide resistance, and malarial drug resistance), environmental factors (e.g., agriculture and irrigation), socioeconomic factors (financial cost of malaria interventions and access to high-quality healthcare), and operational factors such as implementation in local communities. 14 Consequently, improving malaria intervention measures requires a multidisciplinary and multisectoral approach. Our International Center of Excellence for Malaria Research (ICEMR) has been conducting multidisciplinary research on malaria transmission, epidemiology, and immunology through a strong partnership with collaborators in Kenya and Ethiopia. In this article, we describe our ICEMR’s engagement with local and national partners and communities, collaborative research efforts with these stakeholders, and outcomes of these research activities.
ENGAGEMENT OF PARTNERS AND COMMUNITIES
The main scientific aims of our ICEMR are to: 1) examine the impact of water resource development projects and irrigation-based agricultural activities on malaria risk and 2) generate high-quality quantitative data that can be used to enhance malaria control and elimination efforts in Kenya and Ethiopia. Research activities and progress made by the ICEMR have been reported annually to the Scientific Advisory Group appointed by the US National Institutes of Health (NIH) that provides advice and guidance in project implementation. Because the ICEMR addresses cross-disciplinary issues related to agriculture, water management, and human health, we have built a strong partnership with diverse government agencies (e.g., Ministries of Health [MoH], Agriculture, Interior, and Water and Irrigation) and academic and research institutions in Kenya and Ethiopia. Local communities are the beneficiaries of this interaction (Figure (Figure1). 1 ). We operationalized our ICEMR with the knowledge and support of national malaria control programs (NMCP) and implemented technology transfer at the county and community levels. Engagement of the ICEMR with these various partners is summarized in Table Table1. 1 . At the national level, we have collaborated and consulted with MoHs, the President’s Malaria Initiative (PMI) of USAID, and the Global Fund to Fight AIDS, Tuberculosis, and Malaria, and contributed to national malaria control strategy development and policy recommendations concerned with different ecoepidemiological settings. At the county and local community levels, the ICEMR has contributed to strengthen the capacity and quality control of health facilities staff, malaria control program coordinators and managers, community health workers, and village youth groups. These interactions include a series of educational activities and technical trainings pertinent to malaria surveillance and control. Specific topics have included active case detection, passive case detection, reactive case detection, mass blood surveys, development and evaluation of vector surveillance and control tools, malaria awareness, and data collection, collation, and reporting. Attendees at these meetings and trainings included nurses, community health workers, and laboratory technicians at the various ICEMR study sites (Figure 2A–E ). Our ICEMR also interacts with irrigation projects that are sponsored by local and national governments or privately owned. The Arjo Diddessa Sugar Factory in Ethiopia is sponsored by the government of Ethiopia while the Saudi Star Agricultural Development Company in Gambella is privately owned. The Kimira-Oluch Smallholder Farm Improvement Project in Homa Bay, Kenya, is sponsored by the national government. Hence, communities in both Kenya and Ethiopia have benefited from these interactions based on the following key outcomes: 1) developing and enhancing vector surveillance and control tools; 2) supporting in optimizing vector control strategies; 3) improving malaria diagnosis and treatment; 4) strengthening malaria surveillance and control capacity; 5) advancing malaria risk assessment; and 6) strengthening the capacity and sustainability of malaria surveillance and control.

International Center of Excellence for Malaria Research (ICEMR) engagement with government agencies, academic and research institutions, partners, and local communities. Research studies are guided by the Scientific Advisory Group. The project has engaged Kenyan and Ethiopian government agencies and local and global partners. Outcomes of the project facilitate malaria surveillance and control in the community.
Engagement of ICEMR with partners in Kenya and Ethiopia
| Partners | ICEMR engagement |
|---|---|
| Ministry of Health (MoH) | |
| Ministry of Agriculture | |
| Ministry of Water, Sanitation, and Irrigation | |
| Ministry of Education | |
| Ministry of Interior and Coordination of National Government | |
| Government-owned and private industries | |
| Academic and Research Institutions | |
ICEMR = International Center of Excellence for Malaria Research; IRS = indoor residual spraying; LLIN = lasting insecticidal-treated net.

Community engagement in ICEMR activities in Kenya and Ethiopia: ( A ) health facility nurses receiving training in malaria passive surveillance; ( B ) meeting with hospital management team; ( C ) community health workers receiving training in active surveillance; ( D ) indoor residual spray training of community operators; and ( E ) malaria diagnosis training of ICEMR staff.
DEVELOPING AND ENHANCING MALARIA VECTOR SURVEILLANCE AND CONTROL TOOLS
Vector surveillance tools..
Alternative and cost-effective tools suitable for outdoor vector surveillance are required to assess the extent and impact of outdoor malaria transmission. Though the human landing catch method is considered the gold standard for indoor and outdoor malaria vector surveillance, it has the drawbacks of difficulty in standardization, cost, and imposing malaria risk to the collectors. The ICEMR has improved three vector surveillance tools—the sticky clay pot trap, human odor-baited light trap, and human-baited double net/CDC light trap combination. 15 , 16 The sticky clay pot trap adds sticky paper to a previously used clay pot trap 17 to enhance mosquito collection efficacy. It is made of locally available materials, has low maintenance cost, is easy to use, and has a capacity of capturing 1.6 times more Anopheles gambiae mosquitoes compared with an ordinary clay pot. 16 The human odor-baited CDC light trap and human-baited double net/CDC light trap combination caught two to three times and six times as many mosquitoes as a standard CDC light trap, respectively. 15 The human-baited double-net/CDC light trap combination yielded a similar vector density as human landing catch. 18 These exposure-free mosquito surveillance tools pose no risk of mosquito bites compared with human landing catches and, thus, are recommended for outdoor biting malaria vector surveillance and monitoring impact of vector control interventions.
Long-lasting insecticidal-treated nets with piperonyl butoxide (PBO) synergist.
In 2021, the Kenya MoH introduced PBO nets as a pilot intervention in three counties in Western Kenya, where insecticide resistance is high and malaria prevalence is >20%. 19 Our ICEMR is currently conducting an implementation study to evaluate the effectiveness of PBO nets and IRS on clinical malaria in comparison to conventional LLINs. Analysis of data from first 9 months of the study showed 43% reduction in transmission intensity and 48% reduction in clinical malaria incidence in villages that received PBO nets compared with those that received the standard pyrethroid only LLINs. Incidence reduction due to PBO nets was lower than Actellic 300CS-based IRS (adjusted incidence ratio 0.93); however, the cost of PBO nets was lower than IRS. The average cost per person protected is US $6.5 for PBO nets versus $8.4 for IRS in 2021, making PBO nets more cost-effective in terms of cost per malaria case averted. (Calculated as the annual program costs divided by the total number of cases averted, the total cost was $34 for PBO nets as compared with $55 for IRS.) Results from this study will provide information for rational decision-making with regard to the rollout of PBO nets in areas with pyrethroid-resistant malaria vectors.

Larviciding.
Larval source management (LSM) is recommended by the World Health Organization (WHO) as a supplementary measure to core interventions in areas, where larval habitats are few, fixed, and findable. LSM may also be considered for use during specific times of the year when habitats are restricted, for example, the dry season. Larviciding has not been incorporated in the national control programs in Kenya and Ethiopia, but a few small-scale research trials of water-dispersible granular formulations of Bacillus thuringienis var. israelensis ( Bti ) and B. sphaericus ( Bs ) were conducted in Western and Coastal Kenya with significant reduction in adult mosquito densities. 20 – 23 The main constraint with microbial larvicides used in these trials is their short duration of efficacy that would require frequent and costly application in NMCP. We previously evaluated the effectiveness of a slow-release Bti and Bs briquette formulation in Kisumu County where malaria transmission is perennial and high and Western Kenya highland areas, where malaria transmission is unstable and low. The findings demonstrated a significant reduction in indoor and outdoor biting density of malaria vectors and transmission intensity in both areas. 24 , 25 These results will guide the national malaria control program of Kenya on LSM strategy, including the selection of microbial larvicide formulation, as they plan to implement larviciding using microbicides.
Optimal combination of vector control tools.
Key malaria vector control tools—LLIN and IRS—have been very effective in Kenya and Ethiopia. However, their effectiveness has apparently diminished due to insecticide resistance and outdoor malaria transmission. On the other hand, IRS is labor intensive and expensive and LSM may not be cost-effective and applicable in all ecoepidemiological settings. 26 Given the limitations of these tools, important questions faced by the malaria control managers need to be answered. For example, how should these vector control tools be combined and implemented to have synergy and maximal impact on malaria burden under the given funding constraints? Further, how should malaria control interventions be adapted locally to changing vector ecology, behavior, and malaria risks? Our ICEMR is conducting a cluster-randomized sequential, multiple assignment randomized trial in Kisumu County in Kenya to evaluate the impact of adaptive interventions that involve sequential and combinational use of PBO nets, IRS, and LSM for malaria control. 27 Results from this study, anticipated to be complete in 2024, will provide a strategy for effective interventions tailored to local vector ecology, malaria risks, and cost effectiveness.
IMPROVING MALARIA DIAGNOSIS AND TREATMENT
Ultrasensitive malaria rapid diagnostic tests..
The WHO recommends that all malaria suspected cases should be treated only after confirmatory diagnosis by either microscopy or rapid diagnostic test (RDT). 28 Although microscopic inspection of blood smears is the historical standard for Plasmodium parasite diagnosis, this method requires experienced slide readers to provide accurate diagnosis. The RDT, on the other hand, has benefits over microscopy in that it is less labor intensive, does not require electricity, and can be performed by unskilled personnel. However, RDT sensitivity can be compromised by the high prevalence of Pfhrp- 2/3 gene deletion with false–negative results, especially in Ethiopia. 29 The changing national malaria control landscape from control to elimination requires easy to use and sensitive diagnostic methods. The ICEMR evaluated the sensitivity and specificity of different malaria diagnostic methods at health facilities using microscopy, conventional CareStart RDT, and Alere ultrasensitive RDT. The results showed a 21% positivity rate by microscopy, 30% positivity by conventional RDT, and 36% positivity by ultrasensitive RDT. These results are indicative of ultrasensitive RDT detecting more malaria cases than the conventional RDT and microscopy. The finding from this study will help NMCP to consider using ultrasensitive RDT in areas approaching malaria elimination.
Plasmodium vivax treatment with low-dose primaquine.
Plasmodium vivax endemicity is a major barrier to malaria elimination across much of Sub-Saharan Africa, including Ethiopia, where this Plasmodium species accounts for 35% of febrile malaria cases. 30 Unlike P. falciparum, P. vivax has the ability to relapse weeks to years after exposure to infective mosquitoes because of its dormant liver or hypnozoite stage that are a potential source of relapsing blood-stage infections. Vivax relapses can only be prevented by eliminating hypnozoites, and primaquine (PQ) is currently the only licensed drug for radical cure. However, the effectiveness of a 3-day course of chloroquine and 14-day low-dose PQ combination treatment on relapse of P. vivax infections in a real world situation in Ethiopia is unknown. The ICEMR is currently conducting an observational study to examine the efficacy of PQ for preventing recurrence or relapse of P. vivax and the reduction of P. vivax infectiousness to mosquitoes in Ethiopia. We have observed that a large proportion of the Ethiopian study participants that received the chloroquine–PQ combination treatment showed recurrence of blood-stage P. vivax within the 6-month follow-up period. This study is in progress. Data to date indicate there is low adherence to completion of the 14-day PQ treatment regimen. Note that similar studies were not being conducted in the ICEMR Western Kenyan study sites because vivax malaria is very rare in this area of the country.
STRENGTHENING MALARIA SURVEILLANCE
Malaria burden in the two ICEMR countries is monitored by routine data collected from health facilities and community surveillance that is aggregated and reported on a monthly basis in the electronic health information system such as the District Health Information System 2 (DHIS-2) in Kenya and electronic Health Management Information System (e-HMIS) in Ethiopia. These data are used for malaria risk stratification and malaria control strategy development. A number of factors can affect the quality of health facility data, including treatment seeking behavior by residents, diagnosis quality, quality and completeness of case reporting, and occasional nonoperation of health facilities due to staff strikes. The ICEMR has established demographic, entomological, and epidemiological surveillances in the study sites, tracked preventive measures, treatment seeking behavior, and population movement. This dataset has provided a robust and precise sampling framework for evaluating the impact of existing or new malaria control interventions. For example, the high malaria burden in many districts in Kenya and Ethiopia calls for improving the effectiveness of existing interventions. Optimizing first-line intervention tools and integrating newly approved or prequalified products into control programs should be based on precise information related to temporal changes in local malaria epidemiology and vector bionomics that can be obtained from such surveillance systems. 31 Additionally, clinical malaria case incidence detected by active case detection in a cohort of residents in Kisumu County using the demographic surveillance system (DSS) database was found to be significantly higher than the incidence detected by active case detection. A healthcare seeking behavior survey indicated that a considerable proportion of residents did not seek diagnosis and treatment at health facilities; rather, community residents purchased antimalarial drugs from local drug stores (31.5%) or used herbal medicine (3.5%). We estimated that about 35% of community residents who experience clinical malaria are not captured in the DHIS-2. Under reporting of malaria, cases in the DHIS-2 will not reflect the true trend of malaria prevalence/incidence and assessment of impact of malaria interventions. This omission has implications pertinent to the reliability and completeness of the DHIS-2. Accordingly, data from online health information systems should be used with caution when extrapolated to population-level malaria risk and burden. These findings will guide the Kenyan MoH in strengthening HMIS by improved malaria advocacy, community awareness, and community case management of malaria.
ADVANCING MALARIA RISK ASSESSMENT
Many African countries including Ethiopia and Kenya are developing irrigation schemes and hydroelectric power projects with the aim of ensuring food security and sustained energy production. Our studies indicate that communities in close proximity to irrigated areas and dams are at higher risk of Plasmodium infection compared with those living farther away due to increased mosquito proliferation resulting from environmental changes induced by these development projects. These data underscore the need to strike a balance among food security, economic development, and health services through enforcement of environmental and health impact assessments prior to construction of water resource projects. One of the research goals of our ICEMR is to develop a cost-effective and realistic plan to mitigate mosquito proliferation and malaria transmission before and after environmental modifications are implemented. This will require intersectoral collaboration and strengthening of healthcare delivery systems in communities located in and near water resource development projects. Integration of hydrological models with malaria transmission models, an approach adopted by the ICEMR, can assist the risk assessment and development of rational water-management strategies for malaria burden mitigation. 32
STRENGTHENING AND SUSTAINING CAPACITY ON MALARIA SURVEILLANCE AND CONTROL
One of the challenges faced by NMCP in Sub-Saharan Africa is heterogeneity of transmission in different settings whereby an intervention in a particular zone may not necessarily be effective in another zone. With the devolution of health services from the national to the county level, local capacity is critical to address community malaria surveillance and control needs. Unfortunately, most countries in Africa have an inadequate number of skilled personnel at the local level to manage and implement malaria surveillance and control activities. The ICEMR played a pivotal role in strengthening capacity of various health cadres in the national malaria control program. Nurses, technicians, malaria coordinators, public health officers, and health workers at the local community level have received training pertinent to malaria parasite and mosquito surveillance techniques, molecular techniques, genotyping, vector ecology, vector behavior, insecticide resistance monitoring, and evaluation of vector control interventions. Youth groups from the study sites have been trained to perform IRS, distribute LLINs, and collect and analyze healthcare data. The ICEMR has provided research training opportunities to 12 PhD and MSc students from Kenya and Ethiopia related to malaria vector biology, epidemiology, immunology, and pathogenesis. To sustain the capacity in malaria surveillance and control in both countries, training of graduate students and junior scientists is also being supported by grants from the NIH Fogarty International Center and local universities in Kenya and Ethiopia. This effort has strengthened malaria control and elimination at the national and district levels as these trainees are involved in designing, implementing, monitoring, and evaluating in malaria control and elimination program. Moreover, some of our ICEMR staffs serve as members of the malaria technical advisory group and national vector control working group in Kenya and Ethiopia.
Changes in vector ecology, behavior, malaria risk, and insecticide resistance coupled with weak healthcare systems and increased costs of interventions are challenges to the success of malaria control programs in Africa. Environmental modifications that impact water use for irrigation undertaken to ensure food security and boost energy generation further complicate malaria control and elimination. Our ICEMR has been playing an important role in improving vector surveillance and control tools, enhancing malaria surveillance, developing optimal control strategies, and research capacity building in Kenya and Ethiopia. Through partnerships with MoH, other government agencies and nongovernmental organizations, the ICEMR has generated new evidence to inform local strategic planning for malaria control and elimination that will inform policy recommendations made by decision-makers and stakeholders in Kenya and Ethiopia.
ACKNOWLEDGMENTS
We thank Matthew Murphy, MD of the US President’s Malaria Initiative and Centers for Disease Control and Prevention for providing guidance to the ICEMR research program, and two anonymous reviewers for their constructive comments. The research described in this article was supported by grants from the National Institutes of Health (U19 AI129326 and D43 TW001505). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The Research Office is established in the Academic Department and operates under the office of a Registrar who assists the Deputy Director in charge of Academics (DDA) to manage this area.
Strategic objectives
KMTC aims to enhance institutional research capacity through the following strategies:
- Building capacity of staff to carry out research
- Disseminating research findings to stakeholders
- Mobilizing resources for research
- Establishing Research and Scientific Committees in all campuses
- Developing a Monitoring and Evaluation framework for research activities
Research Policy
KMTC has a Research Policy that guides its research activities and ensures that the College upholds the highest ethical standards in a research community that is committed the principals of integrity, trust, justice and collegiality. The Policy has encouraged and empowered staff and students to conduct, disseminate and report results effectively through the creation of an enabling environment and the development of a research culture. KMTC has developed Standard Operating Procedures (SOPs) to operationalize the Research Policy. The Research Policy can be accessed here .
Science, Innovation and Technology Strategy
KMTC aligns its research priorities to the national strategies for Science, Innovation and Technology (STI), geared towards realization of the country’s long-term development goals. More information on this can be found here
The College allocates funds for research activities every financial year to fund research studies, attend symposia, workshops, seminars and conferences both nationally and internationally. It encourages studies that stimulate new innovative approaches and ideas that contribute to KMTC’s strategic priorities and general public health concerns in areas such as, training, student welfare, healthcare access, health finance and other emerging issues. The College also provides training opportunities to staff in all areas of research; proposal writing, publishing, review and evaluation of research documents and assessment.
Research Programs
The College has established internal research program which is funded internally. This program involves various research activities which include conferences, symposia, and research studies. The principal areas of focus for the College research programs are listed as follows.
- Student Welfare
- Health Care Access
- Public Health
- Health Financing
- Human Resource for Health
- Universal Health Coverage
Besides, internal funding, KMTC actively applies for external research funding to complement internal funding.
Scientific Conference and Symposia
Kenya Medical Training College (KMTC) has established a bi-ennial Scientific Conference geared towards enhancing collaboration and exchanging ideas. KMTC conference brings together scientists from different fields of specialization to learn about recent developments, present new data and critically discuss advances in the scientific world. KMTC attaches great importance to the Conference, as it is a culmination of one of its core mandates. It envisages bringing together experts/senior scientists, policy makers and young scientists to deliberate on topical issues affecting health delivery in Kenya.
The College also holds symposia every year aimed at addressing emerging issues in the healthcare sector.
The KMTC Research Webinar Series is a monthly online interactive event that aims at improving research skills among KMTC faculty and the public. The series began in January 2021 and so far, 11 online webinars on various research topics have been held. The organizers of the series have been keen to invite various experienced professional from different organizations to share their experiences in various aspects of research. The series has attracted a loyal following of faculty members who find it valuable to their work and development. For more information on the webinars, please email [email protected].
KMTC has established the International Journal of Health Professions (IJHP): Health through research education and research. The journal provides an avenue for sharing research findings, innovations, recent developments and future research prospects. Below is a list of journals: –
| Issue | Volume | Month | Year |
| 1 | 1 | December | 2013 |
| 1 | 2 | December | 2014 |
| 1 | 3 | June | 2018 |
USEFUL LINKS
- KMTC Research Policy
- National Research Fund (NRF)
- National Commission of Science Technology and Innovation (NACOSTI)
- Kenya National Innovation Agency (KENIA)
- Faculties and Departments
- Calendar of College Training Activities
- Library Catalogue
- Digital Resipitory
- Student Industrial Attachment
- Intake Adverts
- Entry Requirements
- How to Apply
- Payment Options
- Financial Aid
- Campus Contacts
- Students Representative Council
- Student Support Services
- Health Services
- Accommodation Services
- Catering Services
- Clubs and Societies
- Why Choose KMTC
- Chairperson’s Message
- CEO’s Message
- Board Functions
- Organization Management
- Partnerships and Collaborations
- Events and Speeches
- Recruitment
- Industrial Attachment
- Tenders and Contracts
- KMTC Contacts
- Admission Portal
- Short Courses
- Staff & Student Portal
- Cert Verification
25 Best Medical schools in Kenya
Updated: February 29, 2024
- Art & Design
- Computer Science
- Engineering
- Environmental Science
- Liberal Arts & Social Sciences
- Mathematics
Below is a list of best universities in Kenya ranked based on their research performance in Medicine. A graph of 367K citations received by 30.4K academic papers made by 25 universities in Kenya was used to calculate publications' ratings, which then were adjusted for release dates and added to final scores.
We don't distinguish between undergraduate and graduate programs nor do we adjust for current majors offered. You can find information about granted degrees on a university page but always double-check with the university website.
1. University of Nairobi
For Medicine

2. Moi University

3. Kenyatta University

4. Jomo Kenyatta University of Agriculture and Technology
5. Egerton University

6. Maseno University

7. Mount Kenya University

8. Masinde Muliro University of Science and Technology

9. University of Eldoret

10. Strathmore University

11. Kenya Methodist University

12. Catholic University of Eastern Africa
13. Great Lakes University of Kisumu

14. Jaramogi Oginga Odinga University of Science and Technology

15. Pwani University

16. Technical University of Kenya

17. Technical University of Mombasa
18. South Eastern Kenya University

19. Daystar University
20. Karatina University

21. Dedan Kimathi University of Technology

22. University of Kabianga

23. Africa International University

24. Machakos University

25. University of Eastern Africa, Baraton

The best cities to study Medicine in Kenya based on the number of universities and their ranks are Nairobi , Eldoret , Njoro , and Maseno .
Medicine subfields in Kenya
School of Public Health
Research projects in kenya, innovations in hiv prevention and treatment heading link copy link.
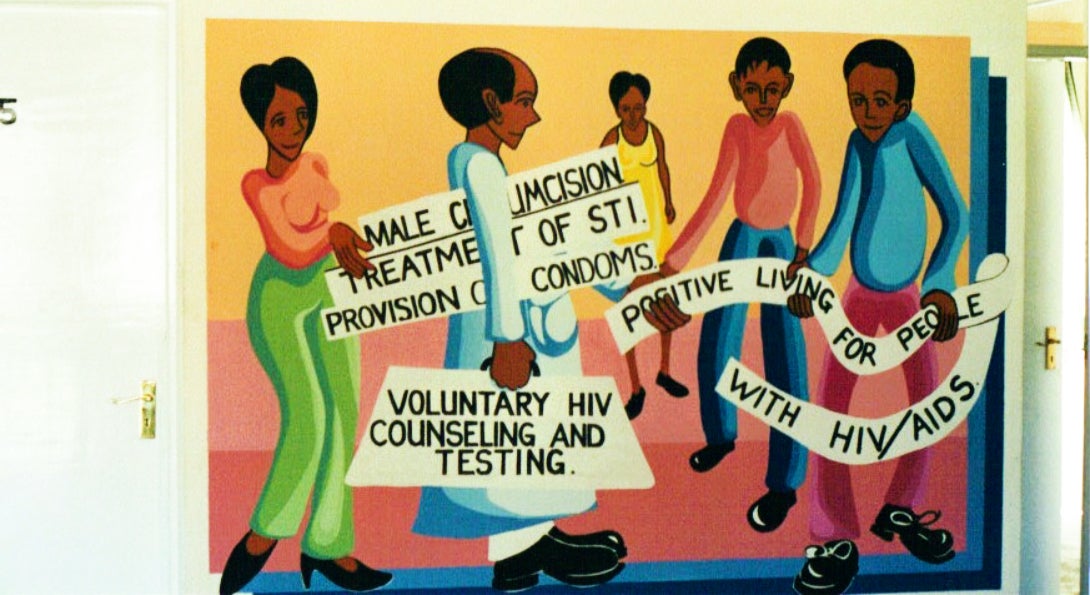
HIV remains a global pandemic, with 37 million infected. An excess of new infections occur in sub-Saharan Africa. Hearteningly, it is estimated that the scale-up of voluntary medical male circumcision (VMMC) has averted 2 million HIV infections and 300,000 deaths since the results of three randomized controlled trials in sub-Saharan Africa proved the efficacy of VMMC in reducing HIV transmission in 2006.
One of those trials, in Kisumu, Kenya, was led by Robert Bailey, PhD, professor emeritus of epidemiology. With support from the National Institutes of Health (NIH), Bailey conducted the trial from 2002-2006, demonstrating a 60 percent reduction in HIV incidence among men undergoing VMMC, with post-trial surveillance showing efficacy maintained through at least 6 years.
From 2010-2015, Bailey led country-wide scale-up with support from the Bill & Melinda Gates Foundation and Centers for Disease Control and Prevention. Throughout that time, Bailey’s program in Kenya supported and graduated 5 MS and 7 PhD students. Results of this research have global reach, informing several of the World Health Organization guidelines for VMMC practice and scale up.
Over the years, 30 MPH students have completed their global health practicum through our Kenya program. Importantly, Bailey’s research in Kenya has provided a platform for other SPH faculty to conduct research successfully in Kenya.
- Meet the researcher
Experiences of violence among adolescent girls in rural Kenya Heading link Copy link
Violence against women is endemic across much of Sub-Saharan Africa. In Kenya, 47 percent of women aged 15-49 have experienced physical or sexual violence in their lives, with most violence among ever-married women occurring at the hands of a current or former partner. Among adolescent girls 15-19 years, 35 percent report having experienced physical or sexual violence. Physical and sexual violence that occurs in during youth is associated with a wide variety of adverse outcomes, including increased HIV/AIDS risks, physical harm, and decreased psychosocial wellbeing and educational attainment. Moreover, these harms and risks increase as the number or severity of violence increases.
Led by Alisa Velonis, PhD, assistant professor of maternal and child health, this study aims to characterize of types of violence and examine whether violence and/or forced sex is associated with educational or mental health outcomes, in particular school absence and quality of life.
Sparking new interventions: microbiome research and sexual and reproductive health Heading link Copy link

After serving as a co-investigator to the VMMC trial, SPH’s Supriya Mehta, PhD, interim associate dean of global health, was awarded NIH funding to study microbiome-related HIV and sexually transmitted infection risk in Kenya. Focusing on the microbiome (bacterial community) as a central driver of women’s risk of sexually transmitted infections, Mehta and colleagues from UIC collaborated with peers in Kenya to demonstrate that the male partner’s penile microbiome composition accurately predicts a woman’s risk of vagina infection up to one year later. These results have been featured in numerous news outlets, including CNN, Newsweek and Fox News, reflecting the importance of the study to the public.
New approaches to effective treatment are needed; modifying the penile and vaginal microbiome may be one such approach. Building on this work, Mehta is evaluating the effect of menstrual cups on the vaginal microbiome and subsequent risk of HIV and sexually transmitted infections in adolescent schoolgirls in rural Kenya. Menstrual hygiene management (MHM) is a pervasive problem across low- and middle-income countries, and a lack of MHM materials negatively impacts girls’ school life and increases vulnerability to coercive sex. In addition to being a long lasting solution to MHM, menstrual cups may protect the vaginal microbiome by preventing use of unhygienic alternatives.
Solar-powered household water treatment to improve health Heading link Copy link
At the intersection of sanitation and clean water Heading link Copy link

People may choose fields, bushes or other open space for defecation if they do not have a toilet readily accessible. Open defecation causes diarrheal disease in children, which leads to malnutrition and increased mortality. As communities shift to ‘open defecation free (ODF)’ and construction of toilets, related diarrheal disease should decrease.
Courtney Babb, MS in Epidemiology ’15, partnered with the Ministry of Health in Nyando District, Kenya, to evaluate latrine intervention conditions in relation to diarrheal disease. Babb and community health workers visited individual households across 33 villages to take water samples for testing and assess latrine conditions. Unexpectedly, children in households without ODF zones had the same rate of diarrhea as children in ODF areas. Babb demonstrated that this was due to greater availability of safer water in the non-ODF areas compared to the ODF areas.
Shockingly, the prevalence of unsafe water by sub-location ranged from 43 percent to 87.5 percent by World Health Organization (WHO) classification of coliform bacteria and other water quality indicators. According to WHO, by 2025, half of the world’s population will be living in water-stressed areas.
Assisting tobacco farmers in finding viable economic alternatives Heading link Copy link
More than eight million people die each year from tobacco-related illnesses. With changing markets, more than 80 percent of the disease burden from tobacco use will fall on low to middle-income countries (LMICs) by 2030. Driving this shift, opponents of tobacco control have argued that tobacco control measures harm smallholder farmers in LMICs; as a result, many governments have been slow to adopt these policies.
Funded by the NIH and the Canadian Institute of Health Research, Jeff Drope, PhD, research professor in health policy and administration, and his colleagues are rigorously examining the economic lives of these farmers in six major tobacco-growing LMICs—Indonesia, Kenya, Malawi, Mozambique, Zambia and Zimbabwe. The project aims to illuminate the broader structures, policies and other important contexts that frame farmers’ livelihoods. Their findings show unequivocally that the tobacco industry’s narrative of farmer prosperity is mostly untrue. In reality, most tobacco farmers are struggling economically much more than their neighbors who do not grow tobacco.
Global Research in Kenya
View Larger Map
Kenya is an east African nation bordering Uganda, Tanzania, Somalia, Ethiopia, and Sudan. More than 80 percent of its population live in rural areas and subsist on agricultural production.
From 2003 to 2006, UNAIDS estimates that annual adult AIDS-related deaths in Kenya declined by nearly 30 percent, which may be attributable to increased availability of free antiretroviral treatments. Kenya has a high incidence of tuberculosis (TB), as well as food- and water-borne diseases, including bacterial and protozoal diarrhea, schistosomiasis, and hepatitis A. Malaria is endemic in many areas, especially around Lake Victoria, as are other vector-borne diseases such as Rift Valley Fever.
NIAID-Funded Activities
Kenya is a major site of NIAID research funding. The primary areas of focus are HIV/AIDS, malaria, and schistosomiasis. NIAID also conducts and funds research in the United States and abroad on a number of tropical diseases that impact Kenya and other African nations.
In 2012, NIAID-funded HIV/AIDS clinical research sites in Kenya joined other collaborators in an ongoing clinical trial testing an investigational TB vaccine in infants at risk for TB infection.
Scientific Advances
Studies in kenya and uganda show that male circumcision significantly reduces risk of acquiring hiv.
In December 2006, NIAID announced an early end to two clinical trials of adult male circumcision because an interim review of the trial data revealed that medically performed circumcision significantly reduces a man’s risk of acquiring HIV through heterosexual intercourse. The trial in Kisumu, Kenya, of 2,784 HIV-negative men showed a 53 percent reduction of HIV acquisition in circumcised men relative to uncircumcised men, while a trial of 4,996 HIV-negative men in Rakai, Uganda, showed that HIV acquisition was reduced by 48 percent in circumcised men.

Country selection
Regulatory Authority
Scope of assessment, regulatory fees, ethics committee, scope of review, ethics committee fees, oversight of ethics committees.
Clinical Trial Lifecycle
Submission Process
Submission content, timeline of review, initiation, agreements & registration, safety reporting, progress reporting.
Sponsorship
Definition of Sponsor
Site/investigator selection, insurance & compensation, risk & quality management, data & records management, personal data protection.
Informed Consent
Documentation Requirements
Required elements, participant rights, emergencies, vulnerable populations, children/minors, pregnant women, fetuses & neonates, mentally impaired.
Investigational Products
Definition of Investigational Product
Manufacturing & import, quality requirements, product management, definition of specimen, specimen import & export, consent for specimen, requirements, additional resources.
Clinical Trials Registries
- ClinicalTrials.gov listing of studies in Kenya
- International Clinical Trials Registry Platform (ICTRP) consolidated listing of studies in Kenya
Ethics Committees
- Database of institutional review boards/ethics committees registered with the United States Department of Health and Human Services (HHS) Office for Human Research Protections (OHRP)
Funding & Institutions
- World RePORT database of funding organizations, research organizations, and research programs in Kenya
- HHS OHRP database of institutions with approved Federalwide Assurances (FWAs) for the protection of human subjects
Kenya Profile Updated
Kenya profile updated in clinregs, kenya: ppb issues guidance for clinical trials impacted by covid-19.
Other Regulatory Databases
- United States Department of Health and Human Services (HHS) Office for Human Research Protections (OHRP) International Compilation of Human Research Standards for Kenya
- Health Research Web - Kenya
Clinical research in Kenya is regulated and overseen by the Pharmacy and Poisons Board (PPB) and the National Commission for Science, Technology and Innovation (NACOSTI) .
Pharmacy and Poisons Board
As per the PPA , the CTRules , and the G-KenyaCT , Kenya’s PPB is the regulatory authority responsible for clinical trial approvals, oversight, and inspections. As described in KEN-21 , the PPB and its Expert Committee on Clinical Trials (ECCT) evaluate all matters relating to clinical trials and grant permission for clinical trials to be conducted in Kenya. See KEN-20 , KEN-21 , and KEN-16 for more information about PPB.
Per the PPA and the CTRules , the PPB is authorized to undertake various mandated duties regarding regulation of medicines including (Note: Each of the items listed below will not necessarily be found in both sources, which provide overlapping and unique elements):
- Advise the government in all matters relating to the safety, packaging, labelling, distribution, and disposal of medicines
- Ensure that all medicinal products manufactured in, imported into, or exported from the country conform to prescribed standards of quality, safety, and efficacy
- Ensure that the personnel, premises, and practices employed in the manufacture, storage, marketing, distribution, and sale of medicinal substances comply with the defined codes of practice and other prescribed requirements
- Grant or revoke licenses for the manufacture, importation, exportation, distribution, and sale of medicinal substances
- Maintain a register of all authorized medicinal substances
- Publish, at least once every three (3) months, lists of authorized or registered medicinal substances and lists of products with marketing authorizations
- Regulate narcotic, psychotropic substances, and precursor chemical substances
- Consider applications for approval and alterations of dossiers intended for use in marketing authorization of medical products and health technologies
- Inspect and license all manufacturing premises, importing and exporting agents, wholesalers, distributors, pharmacies (including those in hospitals and clinics), and other retail outlets
- Prescribe a system for sampling, analysis, and other testing procedures of finished medicinal products released into the market to ensure compliance with the labeled specifications
- Conduct post-marketing surveillance of safety and quality of medical products
- Monitor the market for the presence of illegal or counterfeit medicinal substances
- Regulate the promotion, advertising, and marketing of medicinal substances in accordance with approved product information
- Approve the use of any unregistered medicinal substance for purposes of clinical trials, compassionate use, and emergency use authorization during public health emergencies
- Approve and regulate clinical trials on health products
- Disseminate information on medical products to health professionals and to the public to promote their rational use
- Collaborate with other national, regional, and international institutions on medicinal substances regulation
- Advise the Cabinet Secretary on matters relating to control, authorization, and registration of medicinal substances
- Implement any other function relating to the regulation of medicinal substances
Please note: Kenya is party to the Nagoya Protocol on Access and Benefit-sharing ( KEN-3 ), which may have implications for studies of investigational products developed using certain non-human genetic resources (e.g., plants, animals, and microbes). For more information, see KEN-15 .
National Commission for Science, Technology and Innovation
As delineated in the STI-Act and G-ECBiomedRes , in addition to obtaining the PPB’s permission to conduct research in Kenya, the principal investigator or the head of a research institution must obtain a favorable opinion from an ethics committee accredited by NACOSTI and a NACOSTI research license prior to initiating a study. NACOSTI’s role is to regulate and ensure quality in the science, technology, and innovation sector, and to advise the Kenyan government on related matters. According to Part II of the STI-Act , NACOSTI has specific research coordination and oversight functions, and it liaises with the National Innovation Agency and the National Research Fund to ensure funding and implementation of prioritized research programs. In addition per the STI-Act and KEN-39 , NACOSTI is mandated to register and accredit research institutions in Kenya. The objective of registration and accreditation is to uphold the standard of research in the country and secure public confidence in the national research system. See KEN-32 for more information about NACOSTI’s mandate and functions.
Contact Information
According to the G-KenyaCT and KEN-22 , the PPB contact information is as follows:
Pharmacy and Poisons Board P.O. Box 27663 - 00506 Lenana Road Opp. DOD Nairobi, Kenya
Telephone: (+254) 709 770 100 or (+254) 709 770 xxx (where xxx represents the extension of the officer or office) Email: [email protected] or [email protected] For Clinical Trials Inquiries: [email protected]
According to KEN-29 , the NACOSTI contact information is as follows:
National Commission for Science, Technology and Innovation off Waiyaki, Upper Kabete P. O. Box 30623 00100 Nairobi, Kenya
Phone (landline): (+254) 020 4007000, (+254) 020 8001077 Phone (mobile): 0713 788 787 / 0735 404 245
Email: [email protected] or [email protected]
In accordance with the PPA , the CTRules , the G-KenyaCT , and KEN-21 , Kenya’s Pharmacy and Poisons Board (PPB) , together with its Expert Committee on Clinical Trials (ECCT), is responsible for reviewing, evaluating, and approving applications for clinical trials using registered or unregistered investigational products (IPs). The G-KenyaCT specifies that the scope of the PPB’s assessment includes all clinical trials (Phases I-IV). As delineated in the CTRules , the G-KenyaCT , and KEN-21 , the PPB review and approval process may not be conducted in parallel with the ethics committee (EC) review. Rather, EC approval must be obtained prior to applying for PPB approval. As delineated in the STI-Act and G-ECBiomedRes , the principal investigator or the head of a research institution must obtain a favorable opinion from an EC accredited by the National Commission for Science, Technology and Innovation (NACOSTI) and a NACOSTI research license prior to initiating a study.
Clinical Trial Review Process
Per the CTRules and the G-KenyaCT , the PPB, through the ECCT, communicates the decision to approve, request additional information, or reject the application to the sponsor or the representative in writing within 30 working days of receiving a valid application. The G-KenyaCT indicates that in the case of rejection, the applicant may appeal and provide additional information to satisfy PPB requirements. In specific cases, the PPB may decide to refer the matter to external experts for recommendation.
As specified in the G-KenyaCT , each ECCT member, prior to reviewing the application, will declare any conflict of interest in the study and should have no financial or personal interests, which could affect their impartiality. During the protocol review, the reviewers must use the standard criteria (including available clinical and non-clinical data etc.) defined by the PPB. Confidentiality must be maintained during the review. Per the CTRules and the G-KenyaCT , the PPB/ECCT’s review must consider:
- The reliability and robustness of the data generated in the clinical trial, taking into account statistical approaches, design of the clinical trial, and methodology, including sample size and randomization, comparator, and endpoints
- Compliance with the requirements concerning the manufacturing and import of IPs and auxiliary medicinal products
- Compliance with the labelling requirements
- The completeness and adequateness of the investigator's brochure
Regarding protocol amendments, the CTRules and the G-KenyaCT stipulate that any new information affecting the conduct/management of the trial, safety of the participants, and manufacture of the IP necessitating changes to the protocol, consent form, and trial sites require immediate submission of the amended documents to PPB for review and approval. Arrangements must be in place to take appropriate urgent safety measures to protect participants against any immediate hazard where new events relating to the conduct of the trial, or the development of the IP are likely to affect the safety of the participants. A copy of a favorable opinion letter from the EC on record must be submitted with the request for approval of a proposed amendment to the PPB. PPB approval must be obtained for all substantial amendments. Minor amendments or administrative changes may be implemented after getting the EC’s approval, but a record of these amendments must be kept for possible inspection by the PPB. See Submission Process and Submission Content sections for additional details on amendment submissions. Also, see the G-KenyaCT for examples of substantial amendments.
In addition, per the G-KenyaCT , the sponsor or the representative is required to request approval annually from the PPB at least six (6) weeks prior to the expiration of the previous approval.
Per the CTRules and the G-KenyaCT , the PPB may withdraw the authorization to conduct a clinical trial if it finds that the safety of the participants in the trial is compromised or that the scientific reasons for conducting the trial have changed. Additionally, per the CTRules , the PPB may revoke the approval if it determines that the IP has expired or is not usable.
As delineated in the G-KenyaCT , the PPB may inspect clinical trial sites to ensure that the generally accepted principles of good clinical practice (GCP) are met. The objectives of the inspection are to:
- Ensure that participants are not subjected to undue risks and that their rights, safety, and wellbeing are protected
- Validate the quality of the data generated
- Investigate complaints
- Verify the accuracy and reliability of clinical trial data submitted to the PPB in support of research or marketing applications
- Assess compliance with PPB guidelines and regulations governing the conduct of clinical trials
- Provide real-time assessment of ongoing trials
Per CRO-Inspect , the PPB is responsible for inspecting clinical trial and bioequivalence study sites that generate data for registration of medicines. The PPB requires that these sponsor and contract research organization sites comply with applicable good practices, including GCP, good laboratory practice (GLP), and good documentation practices. Based on risk assessments, the PPB will determine compliance with generally accepted good practice through inspections and, where appropriate, document reviews. In addition, see Cert-Emrgcy for information about GCP and good manufacturing practice certifications during emergencies.
Special Circumstances and Public Health Emergencies
The CTRules delineates that the PPB may, in special circumstances, authorize the conduct of a clinical trial under fast-track procedures or non-routine procedures. PPB may recognize and use clinical trial decisions, reports, or information from other competent authorities authorizing fast-track clinical trials. The special circumstances may include:
- A public health emergency
- The rapid spread of an epidemic disease
- Any other circumstance as may be determined by the PPB
The G-KenyaCT outlines PPB’s scope of assessment of a clinical trial application during a public health emergency. The PPB will conduct an expedited review and liaise with relevant stakeholders (including relevant ECs and other oversight bodies) to facilitate a holistic review of an application in a fast-track manner. The following prioritization criteria must be applied in the selection of applications for expedited review:
- Epidemiology of the emergency
- Morbidity and mortality associated with the emergency and/or condition under study
- Supporting scientific data/information available for the IP at the time of submission
- Feasibility of the implementation of the trial design within the context of the emergency
- Benefit impact of the intervention and/or trial design
In addition, PPB’s assessment will consider the following:
- The research does not compromise the response to an outbreak or appropriate care
- Studies are designed to yield scientifically valid results under the challenging and often rapidly evolving conditions of disasters and disease outbreak
- The research is responsive to the health needs or priorities of the disaster victims and affected communities and cannot be conducted outside a disaster situation
- The participants are selected fairly and adequate justification is given when particular populations are targeted or excluded, for example, health workers
- The potential burdens and benefits of research participation and the possible benefits of the research are equitably distributed
- The risks and potential individual benefits of experimental interventions are assessed realistically, especially when they are in the early phases of development
- Communities are actively engaged in study planning to ensure cultural sensitivity, while recognizing and addressing the associated practical challenges
- The individual informed consent of participants is obtained from individuals capable of giving informed consent
- Research results are disseminated, data are shared, and any effective interventions developed or knowledge generated are made available to the affected communities
STI-Act stipulates that NACOSTI issues research licenses if it finds that the conduct of the research is beneficial to the country and will not adversely affect any aspect of the nature, environment, or security of the country. The license issued will have NACOSTI’s seal and will indicate the commencement and expiration of the research. In addition, NACOSTI maintains a register of all persons granted a license, which is available for public inspection during normal working hours free of charge.
KEN-31 states that if a research license application does not meet the conditions required under the STI-Act , NACOSTI must reject the application and communicate the reasons to the applicant. Any person may appeal NACOSTI’s decision to the Cabinet Secretary within 30 days of being notified of the decision. For approved research, NACOSTI may conduct an evaluation to assess compliance with the conditions of the license. If the research project has not been completed within the stipulated period, the researcher may apply for renewal of the license and pay the requisite fee. The researcher is expected to apply for renewal by attaching a progress report instead of a proposal. KEN-31 indicates that the duration of the research license is one (1) year.
Per the PPA and the G-KenyaCT , the sponsor or the representative is responsible for paying a fee to the Pharmacy and Poisons Board (PPB) to submit a clinical trial application for authorization. The PPB currently requires a non-refundable application fee of $1,000 USD, or the equivalent in Kenya Shillings at the prevailing bank rates.
Payment Instructions
As stated in Annex 2 of the G-KenyaCT , payment is to be made by a bank check payable to the “Pharmacy and Poisons Board” and presented to the PPB’s accounts office upon submitting the application.
Payment can also be made by electronic fund transfer (EFT) to the PPB Bank account, if required. The sponsor or the representative is responsible for all bank charges associated with the EFT. Details of the EFT payment should be obtained from the PPB prior to initiating such a transaction.
As delineated in KEN-31 , the National Commission for Science, Technology and Innovation (NACOSTI) charges a fee that varies depending on the applicant’s status as Kenyan or non-Kenyan, and standing as a researcher (i.e., student, public/private institution, private company). The fees are non-refundable and also apply to research license renewals. Details on additional requirements are provided in the Submission Content section.
- Student, Undergraduate/Diploma: East African Community (EAC) Countries – 100 Kenya Shillings; Kenyan Citizens – 100 Kenya Shillings; Rest of Africa – 200 Kenya Shillings; Non-Africans - $150 USD
- Research (Masters): EAC Countries – 1,000 Kenya Shillings; Kenyan Citizens – 1,000 Kenya Shillings; Rest of Africa – 2,000 Kenya Shillings; Non-Africans - $350 USD
- Research (PhD): EAC Countries – 2,000 Kenya Shillings; Kenyan Citizens – 2,000 Kenya Shillings; Rest of Africa – 4,000 Kenya Shillings; Non-Africans - $400 USD
- Post-Doctoral: EAC Countries – 5,000 Kenya Shillings; Kenyan Citizens – 5,000 Kenya Shillings; Rest of Africa – 10,000 Kenya Shillings; Non-Africans - $500 USD
- Public Institutions: Kenyan Citizens – 10,000 Kenya Shillings
- Private Institutions, Commercial/Market Research, Companies: Kenyan Citizens – 20,000 Kenya Shillings
See KEN-31 for information on service charges.
Per KEN-31 , NACOSTI has migrated payment services for research licensing to the eCitizen platform ( KEN-12 ). East African citizens have the following payment options on KEN-12 with a Kenya Shillings account: mobile money via Mpesa Express or Paybill Number 222222; or these other available payments via KEN-12 :
- Airtel Money
- Kenya Commercial Bank
- Co-operative Bank
- Pesaflow Direct
- National Bank
KEN-31 indicates that non-Kenyans should use the US Dollar account on KEN-12 with these payment options:
- Kenya Commercial Bank (USD)
- Co-operative Bank (USD)
- Equity Cash
- Debit/credit/prepaid card
As per the G-KenyaCT , the G-ECBiomedRes , and KEN-30 , Kenya requires an independent review of research through a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) in one (1) of the local institutions charged with the responsibility of conducting research in human participants. KEN-25 provides a list of the accredited institutional ECs.
Ethics Committee Composition
As delineated in the G-ECAccred , institutional ECs should consist of at least seven (7) members, or an odd number above seven (7). The G-ECBiomedRes states that these members should be multidisciplinary and multisectoral in composition, collectively encompass relevant scientific expertise, balanced age and gender distribution, and include laypersons representing community interests and concerns. Per the G-ECAccred , the composition should meet the following requirements:
- At least one (1) member with knowledge and understanding of Kenyan law
- At least one-third of the members must be female, and one-third must be male
- At least one (1) member who is unaffiliated with the institution
- At least two (2) members must have research expertise and experience, one (1) of whom must be in the health field
- At least one (1) member must be a lay member
- For ECs reviewing clinical research, at least two (2) members must be clinicians, one (1) of whom is currently in active practice or clinical research
- Reflect the regional and ethnic diversity of the people of Kenya
The chairperson must also have some basic training and/or experience in bioethics and leadership. All EC appointments are the responsibility of the institution’s administrative head. See the G-ECAccred and the G-ECBiomedRes for detailed institutional EC requirements.
Terms of Reference, Review Procedures, and Meeting Schedule
Per G-ECBiomedRes , ECs need to have independence from political, institutional, professional, and market influences. As delineated in the G-ECAccred , the G-ECBiomedRes , and the STI-Regs , institutional ECs must operate within written standard operating procedures (SOPs) which delineate the EC’s process for conducting reviews. Per the G-ECAccred , SOPs should include but are not limited to information on EC scope, responsibility, and objectives, institutions served, committee functions, terms and conditions of member appointment, business procedures including meeting schedules and types of reviews, documentation, recordkeeping, and archiving procedures, quorum requirements, communication procedures, and complaint process and dispute resolution procedures. Per the G-ECAccred and the STI-Regs , these documents must be provided to NACOSTI.
Per the G-ECAccred , the quorum for NACOSTI-accredited EC meetings must be:
- At least 50 percent of the membership must form the quorum
- A lay person must be present in all meetings
- For ECs reviewing clinical research, at least two (2) members must be clinicians, one (1) of whom is currently in active practice or clinical research.
The G-ECBiomedRes also defines quorum requirements:
- The minimum number of members required to compose a quorum (e.g., more than half the members)
- The professional qualifications requirements (e.g., physician, lawyer, statistician, paramedical, or layperson) and the distribution of those requirements over the quorum; no quorum should consist entirely of members of one (1) profession or one (1) gender; a quorum should include at least one (1) member whose primary area of expertise is in a non-scientific area, and at least one (1) member who is independent of the institution/research site
Per G-ECBiomedRes , EC member terms of appointment should be established that include the duration of an appointment, the policy for the renewal of an appointment, the disqualification procedure, the resignation procedure, and the replacement procedure. A statement of the conditions of appointment should be drawn up that includes the following:
- A member should be willing to publicize their full name, profession, and affiliation
- All reimbursement for work and expenses, if any, within or related to an EC should be recorded and made available to the public upon request
- A member should sign a confidentiality agreement regarding meeting deliberations, applications, information on research participants, and related matters
Regarding training, EC members should have initial and continued education regarding the ethics and science of biomedical research. The conditions of appointment should indicate the availability and requirements of introductory training, as well as on-going continuing education. This education may be linked to cooperative arrangements with other ECs in the area, country, and region.
For detailed institutional EC requirements and information on other administrative processes, see the G-ECAccred and the G-ECBiomedRes . See KEN-17 and KEN-26 for examples of accredited EC submission and review guidelines.
According to G-ECBiomedRes , the primary scope of information assessed by the institutional ethics committees (ECs) relates to maintaining and protecting the dignity and rights of research participants and ensuring their safety throughout their participation in a clinical trial. The G-ECAccred further states that the National Commission for Science, Technology and Innovation (NACOSTI) accredits ECs in order to uphold the standard of ethics review in the country; develop public confidence and trust in the national research system; facilitate equitable access to research and human health records in health facilities; and facilitate coordination and collaboration among ECs. See the G-ECAccred and the G-ECBiomedRes for detailed ethical review guidelines.
Role in Clinical Trial Approval Process
As per the G-KenyaCT and KEN-21 , the Pharmacy and Poisons Board (PPB) ’s review and approval of a clinical trial application is dependent upon obtaining approval by an accredited institutional EC. Consequently, the PPB and EC reviews may not be conducted in parallel.
As set forth in the G-ECBiomedRes , ECs must be constituted to ensure an independent and competent review and evaluation of all ethical aspects of clinical trials. ECs must review research involving human participants to ensure they meet these ethical principles:
- Respect for persons, including respect of autonomy, protection of vulnerable groups, and protection of privacy and confidentiality
- Beneficence
- Justice, which in research means equitable distribution of the benefits and the burdens
For additional details on the principles and benchmarks for ethical review, see G-ECBiomedRes .
Per the G-ECBiomedRes , expedited review may be permitted for protocols involving no more than minimal risk to research participants.
The G-ECBiomedRes indicates that all ECs should carry out regular monitoring of approved protocols involving human participants. In case of any adverse events, the EC should report this immediately to Kenya’s National Bioethics Committee (NBC).
Per the G-ECBiomedRes , with collaborative research projects, the collaborating investigators, institutions, and countries must function as equal partners with safeguards to avoid exploitation of local researchers and participants. An external sponsoring agency should submit the research protocol to their country’s EC, as well as the Kenyan EC where the research is to be conducted. Further, this research must be responsive to the health needs of Kenya and reasonably accessible to the community in which the research was conducted. Consideration should be given to the sponsoring agency agreeing to maintain health services and faculties established for the purposes of the study in Kenya after the research has been completed. Such collaborative research must have a local/Kenyan co-principal investigator.
As per the G-KenyaCT , G-ECBiomedRes , and KEN-30 , Kenya requires an independent review of research through a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) in one (1) of the local institutions charged with the responsibility of conducting research in human participants. The EC fee to review a clinical trial application will vary depending on the institution. See KEN-25 and KEN-38 for lists of NACOSTI-accredited institutional ECs. For an example of institutional fee requirements charged by the Scientific and Ethics Review Unit (SERU) at the Kenya Medical Research Institute (KEMRI) , see KEN-27 .
As set forth in the STI-Act and KEN-32 , the National Commission for Science, Technology and Innovation (NACOSTI) is the central body responsible for the oversight, promotion, and coordination of research. NACOSTI’s role is to regulate and ensure quality in the science, technology, and innovation sector, and to advise the Kenyan government on related matters. As per the G-ECAccred , NACOSTI has delegated the task of reviewing research proposals for ethical clearance to accredited institutional ethics committees (ECs) to ensure that research conducted in the country observes high research ethics standards.
Per the G-ECBiomedRes , Kenya's National Bioethics Committee (NBC) advises NACOSTI on research ethics. In addition, NBC offers dispute resolution if an applicant is dissatisfied with the decision of an EC. Finally, the NBC must terminate research at any stage if it is found to be harmful to the participants.
Registration, Auditing, and Accreditation
As per the STI-Regs and the G-ECAccred , NACOSTI is responsible for accrediting institutional ECs. Per the G-ECAccred , the application requirements for accreditation are:
- A completed application form ( KEN-10 or Annex III of the G-ECAccred )
- Copy of the standard operating procedures (SOPs)
- Copies of abridged curriculum vitaes (CVs) (no more than four (4) pages) for each member of the proposed EC (including the training attended)
- Profile of the organization/institution detailing the areas of competence (no more than four (4) pages)
Upon creating an account in NACOSTI’s Kenya National Research Information System (KENRIS) ( KEN-23 ), users can perform the following functions:
- Researchers: Apply for researcher registration, register and track applications, and maintain research profile
- Research Institutions: Apply for new research institution registration, maintain/update data, and submit annual reports
- Institutional ECs: Apply for accreditation, preview and track accreditation proposals, submit annual reports, and maintain/update data
Per the G-ECAccred , NACOSTI issues a certificate of accreditation to accredited institutional ECs, which is valid for three (3) years from the date of NACOSTI’s notification. All accredited ECs must submit annual reports to NACOSTI by July 31st for review and monitoring. Applications for renewal of accreditation should be made six (6) months before expiry of the accreditation period. Failure to renew accreditation or failure to maintain the appropriate standards for continuity of accreditation will mean that the accredited status of the EC will lapse at the end of the current accreditation period. Accreditation must be terminated if the accredited committee fails to maintain the required standards. For re-accreditation review purposes, ECs must provide the SOPs under which they will operate. The SOPs are not required as part of the annual reporting process, unless they have been amended, but are required to be stated/included for the re-accreditation review process (every three (3) years). See the G-ECAccred for additional details on the accreditation process.
See the Site/Investigator Selection section for more information on the sponsor and site’s registration and application requirements.
In accordance with the PPA , the STI-Act , the CTRules , the G-KenyaCT , the G-ECBiomedRes , KEN-21 , and KEN-16 , Kenya requires the sponsor or the representative to obtain clinical trial authorization from the Pharmacy and Poisons Board (PPB) ’s Expert Committee on Clinical Trials (ECCT) and an independent ethics review through a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) in a local institution. In addition, the STI-Act and KEN-31 specify that applicants must obtain a research license from NACOSTI prior to initiating a study. The G-KenyaCT also states that the PPB review and approval process may not be conducted in parallel with the EC review. EC approval must be obtained prior to applying for PPB approval.
Regulatory Submission
As described in the G-KenyaCT and KEN-16 , the sponsor or the representative is expected to submit the clinical trial application electronically via the PPB online system ( KEN-16 ). The clinical trial application form is available in KEN-16 . Per the G-KenyaCT , in the event of a multicenter clinical trial, the sponsor should only file one (1) application to the PPB. According to KEN-34 , all application documents should be signed, dated, and version referenced, if applicable, and should be in English. See Annex 7 of the G-KenyaCT to view a flowchart of the submission and approval process.
Per the G-KenyaCT , upon receipt of a clinical trial application, the PPB’s Clinical Trial Division of the Product Safety Department screens the application package for completeness. When an application for a clinical trial is accepted, an acknowledgement of receipt will be issued with a reference number for each application. This PPB/ECCT reference number must be quoted in all correspondence concerning the application in the future. This will be communicated through email to the applicant or through KEN-16 .
Per the G-KenyaCT , sponsors (applicants) can request pre-submission meetings with the PPB to discuss pertinent issues prior to making a formal submissions. The request must be made via KEN-16 or in an official letter and include the following information:
- Background information on the disease to be treated
- Background information on the product
- Quality development
- Non-clinical development
- Clinical development
- Regulatory status
- Rationale for seeking advice
- Proposed questions and applicant’s positions
In addition, per the G-KenyaCT , the letter must be addressed to the Chief Executive Officer of the PPB and sent to [email protected] and copied to [email protected] . The request for a meeting should propose two (2) different dates for the meeting at least three (3) weeks away.
Per G-KenyaCT , any new information that affects the conduct/management of the trial; safety of the participants; and manufacture of the product necessitating changes to the protocol, consent form, and trial sites, etc. will require immediate submission of the amended documents to the PPB for review and approval. Minor amendments or administrative changes may be implemented after getting the EC’s approval, but a record of these amendments must be kept for possible inspection by the PPB.
Per KEN-31 , an application for a NACOSTI research license should be submitted online via the Research Information Management System (RIMS) ( KEN-24 ).
Ethics Review Submission
Each institutional EC has its own required submission procedures, which can differ significantly regarding the application format and number of copies. See KEN-17 for an example of a NACOSTI-accredited EC’s guidelines.
Regulatory Authority Requirements
As per the CTRules , the G-KenyaCT , and KEN-34 , the following documentation must be submitted (signed, dated, and version referenced) to the Pharmacy and Poisons Board (PPB) (Note: Each of the items listed below will not necessarily be found in all sources, which provide overlapping and unique elements):
- Cover letter
- Study protocol
- Proof of study registration in the Pan African Clinical Trials Registry ( KEN-19 )
- Patient information leaflet and informed consent form (ICF)
- Investigators brochure (IB) and package inserts
- Investigational Medicinal Product Dossier (IMPD), including stability data for the investigational product (IP)
- Adequate data and information on previous studies and phases to support the current study
- Good manufacturing practice (GMP) certificate of the IP from the site of manufacture issued by a competent health authority in the manufacturer’s jurisdiction of origin
- Certificate of analysis of the IP
- Pictorial sample of the IPs, including the labeling text
- Signed investigator(s) curriculum vitae(s) (CV(s)), including that of the study pharmacist (the CV should include the current workload of the principal investigator (PI))
- Evidence of contractual agreement between the relevant parties
- Evidence of recent good clinical practice (GCP) training of the core study staff
- Data and Safety Monitoring Board (DSMB) information, including the charter, composition, and meeting schedule
- Detailed study budget
- Financial declaration by the sponsor and PI ( KEN-2 and Annex 5 of the G-KenyaCT )
- No conflict of interest declaration by the sponsor and PI
- Signed declarations by the sponsor, PI, and the monitor that the study will be carried out according to the protocol and applicable laws, regulations, and GCP requirements ( KEN-1 and Annex 4 of the G-KenyaCT )
- Indemnity cover for PI, investigators, and study pharmacist
- Clinical trials insurance cover for the study participants
- Copy of favorable opinion letter from local ethics committee (EC)
- Copy of current practice licenses for the investigators and study pharmacist
- Copy of approval letter(s) from collaborating institutions or other regulatory authorities, if applicable
- For multicenter/multi-site studies, an addendum for each of the proposed sites including, among other things, the sites’ capacity to carry out the study (e.g., personnel, equipment, laboratory)
- A signed statement by the applicant indicating that all information contained in, or referenced by, the application is complete and accurate, and is not false or misleading (Annex 4 of the G-KenyaCT )
- Payment of fees
- Statistical analysis plan
- A signed checklist ( KEN-34 and Annex 2 of the G-KenyaCT )
Per the G-KenyaCT , a request for approval of an amendment must include a summary of the proposed amendments; the reason for the amendment; the impact of the amendment on the original study objectives; the impact of the amendments on the study endpoints and data generated; and the impact of the proposed amendments on the safety and wellbeing of study participants.
KEN-35 describes the submission content for requesting annual approval from the PPB.
Per the STI-Regs and KEN-31 , non-Kenyan applicants must be affiliated with a Kenyan institution. Per KEN-31 , applicants must apply online through National Commission for Science, Technology and Innovation (NACOSTI) ’s Research Information Management System (RIMS) website ( KEN-24 ) and upload the following:
- Passport size color photo in JPG or PNG format
- Scanned ID/passport in PDF format
- Introductory letter from relevant institution signed by an authorized officer
- Affiliation letter from relevant local institution for foreigners signed by an authorized officer and valid for one (1) year
- Grant letter from the funding agency to support the amount indicated to fund the research
- PPB clinical trial approval
- Prior Informed Consent (PIC), Mutually Agreed Terms (MAT), or Material Transfer Agreement (MTA) where applicable, for applications to conduct research on genetic resources and derivatives
- Approved research proposal in PDF format
- Certificate of ethical clearance of the research (see list of accredited ECs in KEN-25 )
- Evidence of payment as the last page of the uploaded proposal
Per KEN-31 , the following conditions apply to the research license:
- The research license is valid for the proposed research, site, and specified period
- Both the research license and any rights thereunder are non-transferable
- NACOSTI may monitor and evaluate the research
- The licensee must inform the relevant County Director of Education, County Commissioner, and County Governor before research commencement
- Excavation, filming, and collection of specimens are subject to further permissions from relevant government agencies
- The research license does not give authority to transfer research materials
- The licensee shall submit one (1) hard copy and upload a soft copy of their final report within one (1) year of completion of the research
- NACOSTI reserves the right to modify the conditions of the research license including its cancellation without prior notice
KEN-31 states that if the research is not completed within the stipulated period, the applicant may apply for renewal of the research license and pay the requisite fee. A progress report should be submitted with the request for renewal instead of a proposal. The progress report must indicate the objectives and activities that have been accomplished, as well as the research work that has yet to be undertaken. KEN-31 further indicates that submissions requesting renewal should be made at least 30 days prior to the expiration of the approval period.
Ethics Committee Requirements
EC requirements vary depending on the specific EC. See KEN-17 and KEN-26 for examples of accredited EC submission and review guidelines.
As set forth in the G-ECBiomedRes , a foreign sponsoring agency must also submit its research protocol for ethics review according to its own country’s standards. This research must be responsive to the health needs of Kenya and reasonably accessible to the community in which the research was conducted.
Clinical Protocol
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). The CTRules the G-KenyaCT , the G-ECBiomedRes , and KEN-14 outline the key elements of a research protocol in Kenya (Note: Each of the items listed below will not necessarily be found in all sources, which provide overlapping and unique elements):
- A project title that adequately captures the essence of the study
- The names, addresses, signatures, and updated abridged curriculum vitae of the investigators
- Evidence that the PI has prior training in GCP
- Contact information for the EC and collaborating institutions
- A summary of the project
- Introduction, background, and literature review, including nonclinical data
- Study objectives, rationale, questions, and hypothesis/es
- Study site, design, and methodology
- Ethical considerations
- Role of investigators
- Publication policy
- Consent explanation - elements of consent explanations
- ICF with signature provisions for participants and the PIs
- Risks and benefits
- Mode of assessment of the safety and efficacy of the IP
- Mode of collecting, analyzing, and reporting the statistics of the clinical trial
- Source data documents of the clinical trial
- Quality control and quality assurance
- Confidentiality
- Recruitment, selection, treatment, and withdrawal of participants
- Compensation and post-trial access program
- Undue inducement and coercion
- Voluntariness
- Alternative treatment(s) if available
- Storage of specimens
- MTA, where applicable
- Data management and statistical analysis
In addition, per the G-KenyaCT , the protocol should have a clear description of study stoppage rules indicating reasons, who makes the decision, and how the decision will be communicated to the PPB and the EC.
Based on the CTRules and the G-KenyaCT , the Pharmacy and Poisons Board (PPB) 's review and approval of an application to conduct a clinical trial is dependent upon obtaining ethics approval from a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC). Therefore, the PPB and EC reviews may not be conducted in parallel. In addition, the STI-Act and KEN-31 specify that all applicants must obtain a research license from NACOSTI prior to initiating a study.
Regulatory Authority Approval
Per the G-KenyaCT , sponsors (or applicants) can request pre-submission meetings to discuss pertinent issues prior to making a formal submission. The request must be made via the PPB online system ( KEN-16 ) or in an official letter addressed to the Chief Executive Officer of the PPB and sent to [email protected] and copied to [email protected] . The request for a meeting should propose two (2) different dates for the meeting with the proposed dates being at least three (3) weeks away. (See Submission Process section for details on the content of request.)
Per the G-KenyaCT , upon receipt of a clinical trial application, the PPB’s Clinical Trial Division of the Product Safety Department screens the application package for completeness, which takes five (5) days. If accepted, an automatic system-generated reference number will be issued for each application. If additional information is needed, the sponsor will have 10 days to respond. The PPB aims to respond to applications within 30 working days. The sponsor or the representative must reference the PPB/Expert Committee on Clinical Trials (ECCT) number in all future application-related correspondence. The application is then evaluated by the ECCT and PPB staff according to their respective standard operating procedures. The PPB/ECCT’s decision to approve, request additional information, or reject the application is communicated to the sponsor or the representative in writing within 30 days of receiving a valid application. If additional information is requested, the sponsor has 90 days to respond after which the PPB has 15 days to issue a final decision. In certain cases, the PPB may refer the application to external experts for their recommendation.
Per the G-KenyaCT , the sponsor or the representative is also required to request approval annually from the PPB at least six (6) weeks prior to the expiration of the previous approval. Refer to the Checklist for Submitting a Request for Annual Approval ( KEN-35 ) for relevant documentation requirements.
Per KEN-5 and KEN-31 , the timeline for NACOSTI’s license application process is 30 days.
KEN-31 states that if a research license application does not meet the conditions required under the STI-Act , NACOSTI must reject the application and communicate the reasons to the applicant. Any person may appeal NACOSTI’s decision to the Cabinet Secretary within 30 days of being notified of the decision.
Ethics Committee Approval
The EC review and approval process timeline will vary by institution.
In accordance with the PPA , the STI-Act , the G-KenyaCT , the G-ECBiomedRes , KEN-21 , and KEN-16 , a clinical trial can only commence after the sponsor or the representative receives authorization from Kenya’s Pharmacy and Poisons Board (PPB) , and ethics committee (EC) approval from an institutional EC that has been accredited by the National Commission for Science, Technology and Innovation (NACOSTI) prior to initiating a study. ECs are accredited pursuant to the requirements delineated in the G-ECAccred . The G-KenyaCT specifies that the PPB review and approval process may not be conducted in parallel with the EC review. In addition, the STI-Act and KEN-31 state that all applicants must obtain a research license from NACOSTI prior to initiating a study. No waiting period is required following the applicant’s receipt of these approvals. Regarding notifications, KEN-31 requires the licensee to inform the relevant County Director of Education, County Commissioner, and County Governor before commencement of the research. Further, the licensee must disclose to NACOSTI, the institutional ECs, and the relevant national agencies any findings that are of national strategic importance.
As per the PPA and the G-KenyaCT , the sponsor or the representative is required to obtain an import license for the shipment of an investigational product to be used in the trial. (See the Manufacturing & Import section for additional information).
As stated in the G-KenyaCT , Kenyan clinical trials should be conducted in compliance with the International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ).
Clinical Trial Agreement
Prior to initiating the trial, the G-KenyaCT requires that the sponsor agree with investigator(s) on the definition, establishment, and assignment of responsibilities specified in the protocol. These responsibilities include conduct of the trial in compliance with KEN-14 and the approved protocol; data management; unblinding of treatment codes; statistical considerations; and preparation of the final clinical report. The sponsor, in a written document, may agree to transfer all related activities of the clinical trial to designated research institutions. However, all responsibility for the trial lies with the sponsor. Prior to the initiation of the clinical trial, the agreement between the sponsor and investigators should be in writing as part of the protocol submitted for PPB approval or in a separate agreement. The sponsor and investigators must sign and date the protocol of the trial to confirm the agreement.
Clinical Trial Registration
As per the G-KenyaCT , all clinical trials taking place in Kenya must be registered in the PPB’s Online Clinical Trials Registry System ( KEN-16 ). The principal investigator is required to log in and set up an account to register a study.
In addition, as required by KEN-34 , all clinical trials taking place in Kenya must be registered in the Pan African Clinical Trials Registry ( KEN-19 ).
Safety Reporting Definitions
According to the CTRules and the G-KenyaCT , the following definitions provide a basis for a common understanding of Kenya’s safety reporting requirements:
- Adverse Event (or Adverse Experience) (AE) – Any untoward medical occurrence in a participant in a clinical investigation study or intervention product, and which does not necessarily have a causal relationship with the treatment
- Adverse Drug Reaction (ADR) – All noxious and unintended responses to a clinical trial study or interventional product related to any dose or all unintended noxious responses to a registered medicinal product which occurs at doses normally used in humans for prophylaxis, diagnosis, or therapy of diseases or for modification of physiological function
- Serious Adverse Event (SAE) – Any untoward medical occurrence that at any dose: results in death, is life threatening, requires hospitalization or prolongation of existing hospitalization, results in persistent or significant disability/incapacity, or is a congenital anomaly/birth defect
- Suspected Unexpected Serious Adverse Reaction (SUSAR) – A serious adverse reaction that is not identified in practice, severity, or frequency by the referenced safety information
Safety Reporting Requirements
Investigator Responsibilities
Per G-KenyaCT , the investigator must ensure that all SAEs are reported promptly to Kenya’s Pharmacy and Poisons Board (PPB) within the mandated timelines, as described below. Proper protection procedures or treatments should be administered to trial participants with SAEs.
Sponsor Responsibilities
As indicated in the CTRules and the G-KenyaCT , the sponsor should report to the PPB and all relevant institutions, all SAEs and SUSARs occurring during the course of the trial. The G-KenyaCT specifies that the sponsor should expedite reporting all SAEs to the PPB and the ethics committee (EC), and the sponsor and investigators should immediately undertake appropriate and necessary measures and treatment to protect the trial participants. The CTRules delineates that where a sponsor conducts a clinical trial on the same health product or active pharmaceutical substance in another country, the sponsor must submit a report of any SUSAR or SAE that occurs in the other clinical trial to the PPB. Per the CTRules and the G-KenyaCT , a sponsor must submit an initial report of an fatal or life-threatening SUSAR or SAE as soon as it occurs but, in any case, not later than seven (7) days after the occurrence of the event. The G-KenyaCT indicates that if the initial report is incomplete, the sponsor must submit a completed report based on the initial information within an additional eight (8) days. As required in the CTRules and the G-KenyaCT , a report of the occurrence of a SUSAR or SAE must specify whether the SUSAR or SAE is related to the clinical trial.
As indicated in the CTRules and the G-KenyaCT , other important considerations and timelines include the following (Note: Each of the items listed below will not necessarily be found in both sources, which provide overlapping and unique elements):
- The sponsor must notify all the investigators involved in ongoing clinical trials of the investigational product (IP) of all SAEs and SUSARs within 15 calendar days
- Any IP-related SAE must receive immediate medical attention and be reported to the PPB
- The SAE report form must be completed (including lab results) and submitted to enable causality assessment
- All fatal cases must be accompanied by a formal autopsy report, and a verbal autopsy report should be submitted in those exceptional cases where a formal autopsy is not possible
- Any frequent IP related AE/ADR must receive immediate medical attention and be reported to the PPB within seven (7) days
- The sponsor must submit a report on a SUSAR that is not fatal or life-threatening within 15 days after the occurrence of the event
- The principal investigator (PI) is required to submit follow-up information as soon as it becomes available
- All additional information should be clearly marked as updated and must include the Protocol Number and Participant Number
- Foreign regulatory decisions that affect the safety or use of the product under study must be reported to the PPB within seven (7) days through a detailed report
- Literature reports that have implications for the safety of the IP must be submitted within 15 days with a detailed report and a copy of the publication
- New information or notification of change in nature, severity, or frequency of risk factors for the product under study or conduct of trial must be submitted within 15 days
Other Safety Reports
The G-ECBiomedRes indicate that ECs should monitor research, and will report to the National Bioethics Committee upon notification of an AE.
The CTRules and the G-KenyaCT state that the sponsor must also submit a safety report to the PPB once a year throughout the clinical trial, or upon request. The purpose of the annual safety report is to briefly describe all new safety information relevant to one (1) or more clinical trial(s), and to assess the safety conditions of the participants enrolled in these trial(s). The safety report must include a log of SAE and SUSAR events. The SAE and SUSAR log should include the following:
- Patient Identification
- Date of recruitment into the study
- Type of SAE or SUSAR
- SAE or SUSAR start and end dates
- Reason for reporting the event as an SAE or SUSAR
- Relation to IP
- SAE or SUSAR outcome
Note that the PPB may require more frequent reporting of the safety reports depending on the nature of the clinical trial being implemented. When this is the case, the PPB must communicate the required frequency to the PI and sponsor in writing.
Form Completion & Delivery Requirements
As per the G-KenyaCT and KEN-16 , all SAEs and SUSARs must be reported to the PPB via the Pharmacovigilance Electronic Reporting System (PvERS) ( KEN-6 ).
Interim and Annual Progress Reports
As stated in the G-KenyaCT , the sponsor and/or the principal investigator (PI) is required to send progress reports to the Pharmacy and Poisons Board (PPB) on an annual basis, or as may be required, from the date of the trial’s initiation. The progress report should contain the following:
- Current status of the study
- Summary of the participants screened (e.g., failed screenings, participants enrolled, withdrawn, or lost to follow-up, and other challenges)
- Summary of protocol deviations and violations
- Updated investigational product Investigator’s Brochure
- Drug Safety Update Report
- Copy of the latest Data Safety Management Board report
- Copy of favorable opinion from the ethics committee (EC) on record
- Copy of annual practice license for the investigators and pharmacists
- Suspected, Unexpected, Serious Adverse Event (SUSAR) and Serious Adverse Event (SAE) Log
For multisite trials, per the G-KenyaCT , the sponsor or the representative must submit a summarized report for all of the sites and include the information listed above.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As per KEN-14 , the investigator should promptly provide written reports to the sponsor and the institutional EC on any changes significantly affecting the conduct of the trial, and/or increasing the risk to participants.
According to the G-KenyaCT , for annual renewal of the study, the sponsor or the representative must submit a copy of the progress report including the documents listed above. The request must also be accompanied by copies of annual practice licenses for the investigators and pharmacists, and a copy of valid insurance coverage for the participants. All documents must be submitted using the PPB’s Online Clinical Trials Registry System ( KEN-16 ). The sponsor or the representative must receive an acknowledgement of this submission before proceeding with the study. These documents must be submitted to the PPB at least six (6) weeks prior to the expiration of the previous approval.
Pursuant to KEN-14 , the investigator should submit written summaries of the trial status to the institutional EC annually, or more frequently, if requested.
Final Report
Per the G-KenyaCT , the sponsor must notify the PPB of the end of a clinical trial taking place at a Kenyan site within 15 days. After the trial has been conducted and closed, the applicant must submit an executive summary report of the study within 30 days. This should be followed by a clinical study report within 180 days of the study closure unless otherwise justified. The report must comply with the International Council for Harmonisation's ICH E3 format ( KEN-13 ). The report must include a short but comprehensive summary of the trial’s essential findings and methodology and should also contain a layman’s summary. Additionally, the sponsor must inform the PPB of any results that will be publicly released at least 14 days before release. In addition, upon completion of the trial, as delineated in KEN-14 , the investigator is required to submit a final report to the institutional EC summarizing the trial’s outcome.
For multi-site research, the G-ECBiomedRes requires all parties to decide on procedures for drafting a common final report and publication at the onset of the research. Individual sites or institutions must not publish any data until the appropriate authorities accept the combined report.
KEN-31 further indicates that the research license applicant must submit one (1) hard copy and upload a soft copy of the final research report to the National Commission for Science, Technology and Innovation (NACOSTI) within one (1) year of the research’s completion.
As per the G-KenyaCT , a sponsor is defined as an individual, a company, an institution, or an organization who takes legal responsibility for the initiation, management, and financing of a trial. According to the G-KenyaCT , a sponsor, in a written document, may agree to transfer all related activities of the clinical trial to designated research institutions. However, all responsibility for the trial lies with the sponsor. The G-ECBiomedRes indicates that sponsors may be foreign, but must comply with certain conditions including affiliating themselves to institutions recognized in Kenya.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). In accordance with KEN-14 , Kenya permits a sponsor to transfer any or all of its trial-related duties and functions to a contract research organization (CRO) and/or institutional site(s). However, the ultimate responsibility for the trial data’s quality and integrity always resides with the sponsor. Any trial-related responsibilities transferred to a CRO should be specified in a written agreement. The CRO should implement quality assurance and quality control.
The G-KenyaCT , which requires sponsors to follow the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), states that the sponsor is responsible for selecting the investigator(s) and the institution(s) for the clinical trial and for ensuring that the investigator(s) are qualified by education, training, and experience.
Per the CTRules and the G-KenyaCT , investigators must also meet the following requirements (Note: Each of the items listed below will not necessarily be found in both sources, which provide overlapping and unique elements):
- Provide evidence of their qualifications and experience through an up-to-date curriculum vitae (CV)
- Have a current practice license from the relevant regulatory authority
- Be familiar with the characteristics and appropriate use of the investigational product (IP) as described in the protocol, current investigator’s brochure (IB), in the product information, and in other information sources
- Have a clear understanding and willingness to obey the ethical, good clinical practice (GCP) and legal requirements in the conduct of the trial
- Permit monitoring and auditing of the trial and inspection by the Pharmacy and Poisons Board (PPB) or appointed representatives
- Keep a list of appropriately qualified persons to whom the investigator has delegated significant trial-related duties
- The principal investigator (PI) must be an appropriately qualified and competent person having practical experience within the relevant professional area and who is responsible for the conduct of the clinical trial at a clinical site
- The PI must have a degree in medicine, pharmacy, pharmacology, toxicology, biochemistry, dentistry, or a related discipline from a university recognized in Kenya
- The PI must have a valid practice license from the relevant regulatory authority
- The PI must have a valid professional indemnity cover
- The PI must be a citizen of Kenya or a permanent resident in Kenya
- A PI must have had previous experience as a co-investigator in at least two (2) trials in the relevant professional area
- Have adequate time and resources to carry out the study (See Annex 6 of the G-KenyaCT for the PPB’s recommended format to document the investigator’s workload)
Further, the G-KenyaCT states that sponsors must ensure that investigators have had formal training in GCPs with proof that a GCP course was attended within the last two (2) years. If training has not been completed, it is the responsibility of the sponsor to organize this training prior to initiating the study. The investigators will need to provide evidence of having obtained this training. As delineated in KEN-14 , prior to entering into an agreement with the investigator(s) and the institution(s) to conduct a study, the sponsor should provide the investigator(s) with the protocol and an IB. Furthermore, the sponsor must sign an agreement or contract with the participating institution(s). Additionally, the sponsor must define and allocate all study related duties and responsibilities to the relevant parties participating in the study. (See the Submission Content section for additional information on clinical trial application requirements.)
Institutional Registration
The STI-Act and the STI-Regs require research institutions to register with the National Commission for Science, Technology and Innovation (NACOSTI) and obtain a Certificate of Registration. For detailed guidance on the vetting and approval process, see the STI-Regs and the G-InstitutionRegistration .
Upon creating an account in NACOSTI’s Kenya National Research Information System (KENRIS) ( KEN-23 ) , research institutions can apply for new research institution registration, maintain/update data, and submit annual reports. The application for registration of research institutions is also provided in KEN-11 , and the reporting tool for registered research institutions is provided in KEN-36 .
Foreign Sponsor Responsibilities
The G-ECBiomedRes requires that with collaborative research projects, the collaborating investigators, institutions, and countries must function as equal partners with safeguards to avoid exploitation of local researchers and participants. An external sponsoring agency should submit the research protocol to their country’s EC, as well as the Kenyan EC where the research is to be conducted. Further, this research must be responsive to the health needs of Kenya and reasonably accessible to the community in which the research was conducted. Consideration should be given to the sponsoring agency agreeing to maintain health services and faculties established for the purposes of the study in Kenya after the research has been completed. Such collaborative research must have a local/Kenyan co-principal investigator.
Data and Safety Monitoring Board
The G-KenyaCT indicates that the PPB recommends establishing a Data and Safety Monitoring Board (DSMB) to monitor trials in the following types of studies:
- Where the endpoint is such that a highly favorable or unfavorable result, or even a finding of futility at an interim analysis, might ethically require the trial to be terminated early
- When there are safety concerns due to the use of a particularly invasive treatment
- Where there is prior information suggesting the possibility of serious toxicity with the study treatment
- Where the participants involved represent a vulnerable population (e.g., children, pregnant women, elderly, terminally ill, or mentally incapacitated)
- When the participants represent a population at higher risk of death or other serious outcomes
- When the study is large, of long duration, and multi-center
KEN-14 states that a DSMB may be established to assess the progress of a clinical trial, including the safety data and the critical efficacy endpoints at intervals, and to recommend to the sponsor whether to continue, modify, or stop a trial.
Per the G-KenyaCT , the DSMB must provide the following documentation to the PPB:
- DSMB composition
- Copy of DSMB charter
- DSMB reports to be submitted to the PPB within two (2) weeks of its deliberations and in the request for annual approval
For multicenter trials, the G-ECBiomedRes requires that centralized data management and analysis should be planned as per G-WHO-DSMB .
Multicenter Studies
Per the G-KenyaCT , for multicenter studies in Kenya, the coordinating investigator should be a Kenyan resident and should assume full responsibility for the trial.
The G-ECBiomedRes requires that multicenter trials conducted simultaneously by several investigators at different sites follow the same protocol. Ideally, these trials should be initiated at the same time at all sites. The sponsor must provide the protocol to the investigators, who will accept the protocol in writing. If approved by the EC of the local host institution, the protocol may be modified to suit the local conditions. Meetings should be organized at the initial and intermediate stages of the trial to ensure uniform procedures at all sites. All sites and parties should also agree on procedures for publication of a final report. Research staff should receive training at every trial site on the uniform procedures. In addition, research staff at all sites should implement standard methods for recruitment and evaluation/monitoring of laboratory procedures and conduct of trial. There must be monitoring to ensure the sites are following the protocol, which must include measures to terminate the participation of some sites, if necessary. Finally, centralized data management and analysis should be planned as per G-WHO-DSMB .
Additional multicenter guidance is delineated in KEN-14 :
- All investigators conduct the trial in strict compliance with the protocol agreed to by the sponsor, and, if required, by the PPB, and given EC approval
- The case report forms (CRFs) are designed to capture the required data at all multicenter trial sites
- Investigator responsibilities are documented prior to the start of the trial
- All investigators are given instructions on following the protocol, complying with a uniform set of standards to assess clinical and laboratory findings, and completing the CRFs
- Communication among investigators is facilitated
As set forth in the G-KenyaCT and the G-ECBiomedRes , the sponsor must provide insurance cover for the study participants and ensure that the clinical trial institution, contract research organization (CRO), and researchers have sufficient insurance cover for the clinical trial. Per the G-KenyaCT , the sponsor’s policies and procedures should address the treatment costs for trial participants in the event of trial-related injuries, and the sponsor should submit this information as part of the clinical trial application (see KEN-34 ). In addition, a no-fault insurance cover must be obtained for all controlled human infection studies. The International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ) guides sponsors on providing insurance. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
For all sponsor-initiated studies, insurance coverage must be provided by an insurer registered by Kenya’s Insurance Regulatory Authority (IRA) , and a valid insurance certificate must be issued by the IRA prior to the trial’s initiation and cover the duration of the study. The insurance certificate must be submitted as evidence to the Pharmacy and Poisons Board (PPB) . The certificate must be properly executed by an insurance company under a valid insurance policy which makes explicit reference to the proposed study. In addition, the policy must grant coverage for any participant injury that is causally linked to trial activities. The policy must also cover the investigator(s)’ and the sponsor(s)’ liability in the trial, without excluding any damage which may be attributed to negligence. Moreover, self-insurance of the participants by other entities, such as the National Health Insurance Fund , will not be sufficient.
Further, per the G-KenyaCT , the sponsor must ensure that the investigators and CROs have professional indemnity insurance coverage for the period of the trial. The host institution must also have in place sufficient insurance to meet the potential liability of its investigators, those acting on behalf of the investigators, and its research members.
Compensation
Injury or Death
As specified in the G-KenyaCT and the G-ECBiomedRes , the sponsor is responsible for providing compensation to research participants and/or their legal heirs in the event of trial-related injuries or death. Per the G-ECBiomedRes , participants are entitled to such financial or other assistance as would compensate them equitably for any temporary or permanent impairment or disability. In the case of adverse events, there should be proper assessment, evaluation, and compensation. The G-ECBiomedRes also indicates that when investigational vaccines contain active or live-attenuated micro-organisms, should participants in the control group contract the disease for which a vaccine is being tested, free treatment must be provided.
In addition, the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ) provides guidance for sponsors on providing compensation to research participants in the event of trial-related injuries or death. The sponsor must explain to participants the compensation and/or treatment available to them in the event of trial-related injuries.
Trial Participation
The G-ECBiomedRes defines compensation to include offers to participants, monetary or otherwise, to offset the time and inconvenience for participating in research.
Post-Trial Access
Per the G-KenyaCT , the sponsor must put in place measures to ensure that the study participants have access to successful investigational products for their disease condition before the products have received a marketing authorization in Kenya, especially for the Phase III clinical trials. The G-ECBiomedRes indicates that when investigational vaccines contain active or live-attenuated micro-organisms, post-trial access to the vaccine should be available to the control group.
Quality Assurance/Quality Control
As stated in the CTRules and the G-KenyaCT , the sponsor is responsible for maintaining quality assurance (QA) and quality control (QC) systems with written standard operating procedures (SOPs) to ensure that trials are conducted and data are generated, recorded, and reported in compliance with the protocol, the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), the STI-Regs , and other applicable regulatory requirements. QC should be applied to each stage of data handling to ensure that all data are reliable and have been correctly processed. In addition, per the STI-Regs , all persons and research institutions (i.e., sponsors) undertaking research in Kenya must ensure the highest standards and quality of research for the realization of institutional mandates and national priorities.
In addition to complying with KEN-14 , the G-KenyaCT indicates QA processes should be developed to ensure:
- Regular and continuous monitoring of the study and the implementation of monitoring reports’ recommendations
- Submission of the study monitoring plan to the Pharmacy and Poisons Board (PPB) during the initial submission of the application
- The clinical trials research site must have valid registrations and approvals
- Patient safety and confidentiality are not compromised
- Analysis or evaluation of samples is performed in accordance with the protocol and good clinical practice (GCP) principles and, where applicable, the contract/agreement, the work instruction, and associated methods
- Adherence to the laboratories’ policies and SOPs
- Trial data is recorded and reported accurately, legibly, completely, and in a timely manner
- Trial data is archived
- Preparation of a work instruction detailing the procedures that will be used to conduct the analysis or evaluation prior to the initiation of sample analysis or evaluation, as necessary
- Be built or adapted for the purpose
- Have automated equipment for routine hematology, biochemistry, and serology tests
- Have procedures for analyzer calibration and quality control
- Regular maintenance of all the equipment, including point-of-care equipment
- Have a procedure for transporting samples safely and quickly from clinical areas to the laboratory
- Have written procedures for all assays, and to validate the assays
- Reagents and consumables are used within their expiry dates based on a stock control procedure
- Records are kept, including source documents and final reports
- Have a procedure for authorizing and releasing results
- Have a procedure for ‘flagging’ and notifying medical staff of abnormal results
- Have a laboratory information management system, and validate and back up the system
- Protective clothing and safety equipment are provided for staff
- Have a central alarm system for all fridges and freezers
- Have an internal audit program
Per KEN-14 , the sponsor should implement a system to manage quality throughout all stages of the trial process, focusing on trial activities essential to ensuring participant protection and the reliability of trial results. The quality management system should use a risk-based approach that includes:
- During protocol development, identify processes and data that are critical to ensure participant protection and the reliability of trial results
- Identify risks to critical trial processes and data
- Evaluate the identified risks against existing risk controls
- Decide which risks to reduce and/or which risks to accept
- Document quality management activities and communicate to those involved in or affected by these activities
- Periodically review risk control measures to ascertain whether the implemented quality management activities are effective and relevant
- In the clinical study report, describe the quality management approach implemented in the trial and summarize important deviations from the predefined quality tolerance limits and remedial actions taken
Per the G-KenyaCT protocol violations and protocol deviations must be reported to the PPB within seven (7) days of the principal investigator (PI) becoming aware of them. The details to be reported must include:
- Date of the deviation/violation
- Study participant(s) affected
- Name of the treating physician
- Detailed description of the deviation/violation
- Indication whether the study participants were adversely affected by the deviation/violation
- Explanation of why the deviation/violation occurred
- Measures taken to address the deviation/violation
- Measures taken to preclude future recurrence of the deviation/violation
In addition, see G-KenyaCT for information about medical care of trial participants during and following the clinical trial. Also see the Bft-Risk for a standardized approach for evaluating and reporting the balance between the benefits and risks of health products, which includes investigational products (IPs) undergoing clinical trial application.
The CT-Emrgcy provides guidance to sponsors, PIs, and institutions on the conduct of clinical trials during public health emergencies to maximize the safety of research participants, minimize risks to participants and the community, and ensure the integrity of the clinical trials. See CT-Emrgcy for details on a range of issues, including contingency planning, communications with participants, changes to studies, protocol deviations, reporting, and supply of IPs during a public health emergency.
Controlled Human Infection Studies
The G-KenyaCT also provides detailed information on controlled human infection studies (CHIS) requirements to ensure investigator/study personnel compliance with GCP and other QA/QC requirements, including the following:
- The well characterized strain of an infectious agent should be administered at a controlled dose and by a specific route to carefully selected adult volunteers
- The studies require safe and accurate microbiology, good clinical facilities, careful recruitment, and monitoring
- Participants must be monitored for evidence of carriage or infection under medical supervision to anticipate or manage symptoms of disease and adverse events
- The value of the information to be gained should clearly justify the risks and the study must have a risk mitigation plan
- The investigators should be adequately qualified, trained, and experienced in the conduct of CHIS as well as treating patients with the infectious disease being investigated
For the complete list of requirements, see the G-KenyaCT .
The G-ECBiomedRes provides additional considerations when investigational vaccines contain active or live-attenuated micro-organisms:
- The participant to be vaccinated should be given adequate information about the adverse effects.
- Should participants in the control group contract the disease for which a vaccine is being tested, free treatment must be provided.
- Because the risks associated with vaccines produced by recombinant DNA techniques are not completely known, PPB guidelines must be strictly followed.
- Post-trial access to the vaccine should be available to the control group
Monitoring Requirements
As part of its QA system, the G-KenyaCT requires the sponsor to develop an internal audit program. The G-KenyaCT defines an audit as a systematic examination, carried out independently of those directly involved in the trial, to determine whether the conduct of a trial complies with the agreed study protocol and whether data reported are consistent with those on record at the site. Further, the sponsor is required to obtain agreement from all involved parties to ensure direct access to all trial related sites, source data/documents, reports for monitoring and auditing purposes, and inspection by domestic and foreign regulatory authorities An investigator must, upon request from any properly authorized officer or employee of PPB, at reasonable times, permit such officer or employee to have access to, and copy and verify any records or reports made by the investigator.
Per KEN-14 , the sponsor should develop a systematic, prioritized, risk-based approach to monitoring clinical trials. The extent and nature of monitoring is flexible and permits varied approaches that improve effectiveness and efficiency. The sponsor may choose onsite monitoring, a combination of onsite and centralized monitoring, or, where justified, centralized monitoring. The sponsor should document the rationale for the chosen monitoring strategy (e.g., in the monitoring plan).
KEN-31 indicate that the National Commission for Science, Technology and Innovation (NACOSTI) may conduct an evaluation, or cause an evaluation to be conducted, of a research study to assess and evaluate compliance with the conditions of the applicable research license.
Premature Study Termination/Suspension
The G-KenyaCT states that if a trial is terminated by the PI or the sponsor, the PI or the sponsor must inform the PPB not later than 15 days following the termination date. The co-investigators must also be informed as soon as possible and should be advised in writing of potential risks to the research participants, and they must ensure that patients continue to receive medical care. The PPB must be provided with reason(s) for the termination and its impact on the proposed or ongoing trials with respect to the IP, including issues relating to IP accountability and disposal as well as record(s) maintenance. In addition, the PPB may withdraw the authorization to conduct a clinical trial if it finds that the safety of the participants is compromised or that the scientific reasons for conducting the trial have changed.
According to KEN-14 , if it is discovered that noncompliance significantly affects or has the potential to significantly affect participant protection or reliability of trial results, the sponsor should perform a root cause analysis and implement appropriate corrective and preventive actions. Further, the EC should also be informed promptly and provided the reason(s) for the termination or suspension by the sponsor.
Electronic Data Processing System
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As per KEN-14 , when using electronic trial data processing systems, the sponsor must ensure that the electronic data processing system conforms to the sponsor’s established requirements for completeness, accuracy, reliability, and consistency of intended performance. Per KEN-14 , the sponsor should base their approach to validate such systems on a risk assessment that takes into consideration the intended use and the potential of the system to affect participant protection and reliability of trial results. In addition, the sponsor should maintain standard operating procedures (SOPs) for the systems that cover setup, installation, and use. The responsibilities of the sponsor, investigator, and other parties should be clear, and the system users should be provided with training. Refer to KEN-14 for additional information.
Records Management
According to the G-KenyaCT , it is the responsibility of the investigator and the sponsor to archive safely all trial-related documentation. All Kenyan trial site-related documentation must be archived within the country and not exported. Additionally, the sponsor/applicant must inform the Pharmacy and Poisons Board (PPB) ’s Expert Committee on Clinical Trials (ECCT) in writing prior to destroying any trial documents. The notification must include the protocol number, start and end date, and the license number.
The G-KenyaCT states that study documents must be archived for a minimum of 10 years from the end of the study. Also, records must be made available to the PPB within three (3) days if there is a concern regarding the use of a clinical trial drug and/or a risk to the health of the clinical trial participant. In any other case, records must be provided within seven (7) days of request.
Per the STI-Regs , sponsors should store research findings and information regarding research systems in a designated location with clear labels of the subject area. Research findings must be documented in bound books or documents with the research title, author, year, and other relevant information clearly printed on the cover page. A report of research work by staff and the research institution must be submitted to the National Commission for Science, Technology and Innovation (NACOSTI) within two (2) months after publication or compilation of the research report.
In addition, KEN-14 states that the sponsor and investigator/institution should maintain a record of the location(s) of their respective essential documents including source documents. The storage system used during the trial and for archiving (irrespective of the type of media used) should allow for document identification, version history, search, and retrieval. The sponsor should ensure that the investigator has control of and continuous access to the data reported to the sponsor. The investigator/institution should have control of all essential documents and records generated by the investigator/institution before, during, and after the trial.
Responsible Parties
For the purposes of data protection requirements, DPA delineates that the sponsor acts as the “data controller” in relation to research data. This is because the sponsor determines the purpose and means of processing personal data. The "data processor" processes personal data on behalf of the data controller. Data controllers and processors must be registered with the Kenya Data Commissioner. Per the DataProtect , an application for registration of a data controller or data processor must be on Form DPR1 (found in the First Schedule of DataProtect ) with supporting materials and the required registration fees as specified in the Second Schedule. See the DataProtect for additional details on registration requirements.
Data Protection
Per the DPA , the data controller (sponsor) must ensure that personal data is:
- Processed in accordance with the right to privacy of the data subject
- Processed lawfully, fairly, and in a transparent manner in relation to any data subject
- Collected for explicit, specified, and legitimate purposes and not further processed in a manner incompatible with those purposes
- Adequate, relevant, and limited to what is necessary in relation to the purposes for which it is processed
- Collected only where a valid explanation is provided whenever information relating to family or private affairs is required
- Accurate and, where necessary, kept up to date, with every reasonable step being taken to ensure that any inaccurate personal data is erased or rectified without delay
- Kept in a form that identifies the data subjects for no longer than is necessary for the purposes for which it was collected
- Not transferred outside Kenya, unless there is proof of adequate data protection safeguards or consent from the data subject
The DataProtect , which implements the DPA , requires data controllers and data processors to develop, publish, and regularly update a policy on their personal data handling practices. The policy should include the nature of personal data collected and held, how a data subject may access their personal data, complaints handling mechanisms, the lawful purpose for processing personal data, and requirements for when personal data is to be transferred outside Kenya. Regarding cross-border transfers of data, a data controller or data processor who is a transferring entity must (before transferring personal data out of Kenya) ascertain that the transfer is necessary. This necessity decision should be based on considerations such as data protection safeguards, an adequacy decision made by the Data Commissioner, and if there is consent of the data subject.
Per the DataProtect , data controllers and/or data processors must retain personal data processed for a lawful purpose and only as long as may be reasonably necessary for the purpose for which the personal data is processed. A data controller or data processor must establish a personal data retention schedule with appropriate time limits and periodic reviews. When the retention period has ended, the personal data must be erased, anonymized, or pseudonymized.
See DataProtect for additional details on data protection, including data subject rights, data protection design and principles, notification of breaches, impact assessments, and exemptions.
See Parts IV-VII of the DPA for detailed requirements on data processing, sensitive personal data, exemptions, and transfer of personal data outside of Kenya. The G-ECBiomedRes requires compliance with the DPA .
Consent for Processing Personal Data
Per the DPA , the data controller (sponsor) or data processor must bear the burden of proof for establishing a data subject’s consent to the processing of their personal data for a specified purpose. For the purposes of processing personal data, consent means any manifestation of express, unequivocal, free, specific, and informed indication of the data subject’s wishes by a statement or by a clear affirmative action, signifying agreement to the processing of personal data relating to the data subject. Unless otherwise provided under the DPA , a data subject has the right to withdraw consent at any time. The withdrawal of consent must not affect the lawfulness of processing based on prior consent before its withdrawal.
The DataProtect requires data controllers and data processors to ensure that a data subject has the capacity to consent and voluntarily gives consent. In seeking consent (prior to the processing), the data subject should be informed of:
- The identity of the data controller or data processor
- The purpose of each of the processing operations for which consent is sought
- The type of personal data that is collected and used
- Information about the use of the personal data for automated decision-making, where relevant
- The possible risks of data transfers due to absence of an adequacy decision or appropriate safeguards
- Whether the personal data processed will be shared with third parties
- The right to withdraw consent
- The implications of providing, withholding, or withdrawing consent
Per the DataProtect , this information may be presented to the data subject through a written notice, oral statement, audio or video message. The data controller or a data processor must ensure that the data subject has the capacity to voluntarily give consent that is specific to the purpose of processing.
The DPA indicates that in cases where the data subject is a minor, a person who has parental authority or a guardian may exercise personal data protection rights conferred on the subject. With regard to data processing, the DPA requires that every data controller (sponsor) or data processor must not process personal data relating to a child unless consent is given by the child's parent or guardian and the processing is in a manner that protects and advances the rights and best interests of the child. A data controller or data processor must incorporate appropriate mechanisms for age verification and consent to process personal data of a child, including available technology, volume of personal data processed, proportion of such personal data likely to be that of a child, possibility of harm to a child arising out of processing of personal data, and other factors as may be specified by the Kenya Data Commissioner.
The DPA indicates that in cases where the data subject has a mental or other disability, a person duly authorized to act as the participant’s guardian or administrator may exercise personal data protection rights conferred on the subject.
Obtaining Consent
In all Kenyan clinical trials, a freely given informed consent must be obtained from each participant in accordance with the requirements set forth in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). (Per the G-KenyaCT , research must be conducted in accordance with the requirements set forth in KEN-14 .) The informed consent form (ICF) is viewed as an essential document that must be reviewed and approved by a National Commission for Science, Technology and Innovation (NACOSTI) -accredited institutional ethics committee (EC). The ICF must be provided to the Pharmacy and Poisons Board (PPB) with the clinical trial application. (See the Required Elements section for details on what should be included in the form.)
The CTRules , the G-KenyaCT , and the G-ECBiomedRes state that the investigator, or the designated representative, must provide detailed research study information to the participant or legal representative/guardian. Per G-ECBiomedRes , all individual consent must be written and, in no case, should collective community agreement or the consent of a community leader or other authority substitute for an individual informed consent. The G-KenyaCT and the G-ECBiomedRes also specify that the oral and written information concerning the trial, including the ICF, should be easy to understand and presented without coercion or unduly influencing a potential participant to enroll in the clinical trial. None of the oral and written information concerning the research study, including the written ICF, should contain any language that causes the participant or legal representative/guardian to waive or to appear to waive the legal rights, or that releases or appears to release the investigator(s), the institution, the sponsor, or the representatives from their liabilities for any negligence. The participant or legal representative/guardian should also be given adequate time to consider whether to participate.
According to the CTRules , the G-KenyaCT , and KEN-14 , any change in the ICF due to a protocol modification should be approved by the EC before such changes are implemented. The participant or legal representative/guardian will also be required to re-sign the revised ICF and receive a copy of any amended documentation.
Language Requirements
As stated in the CTRules and the G-KenyaCT , the ICF content should be presented in either English or Kiswahili, and the local spoken language of the area, where applicable. Copies of the English ICF should be submitted to the PPB and to the EC.
Documenting Consent
The CTRules and the G-KenyaCT state that the participant or legal representative/guardian , and the person who conducted the informed consent discussion should sign and personally date the ICF. Where the participant is illiterate, and/or the legal representative/guardian is illiterate, verbal consent should be obtained in the presence of and countersigned by an impartial witness. Before participating in the study, the participant should receive a copy of the signed and dated ICF, and any other written information provided during the informed consent process. The participant or legal representative/guardian should also receive a copy of any updates to the signed and dated ICF.
According to KEN-14 , where the participant is illiterate and/or the legal representative/guardian is illiterate, an impartial witness should be present during the entire informed consent discussion. The witness should sign and date the ICF after the following steps have occurred:
- The written ICF and any other written information to be provided to the participant is read and explained to the participant or legal representative/guardian
- The participant or legal representative/guardian have orally consented to the participant’s involvement in the trial, and has signed and dated the ICF, if capable of doing so
Before participating in the study, the participant or legal representative/guardian should receive a copy of the signed and dated ICF.
Waiver of Consent
No information is available.
Based on the CTRules , the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), the informed consent form (ICF) should include the following statements or descriptions, as applicable (Note: Each of the items listed below will not necessarily be found in all sources, which provide overlapping and unique elements):
- Title of the project and that the study involves research and an explanation of its nature and purpose
- The expected duration of the participant’s participation
- The participant’s responsibilities in participating in the trial
- Experimental aspects of the study
- Approximate number of participants involved in the trial
- Trial treatment schedule and the probability for random assignment to each treatment
- Principal investigator(s), institution, and ethics committee (EC) contact information, the person(s) to contact for further information regarding the trial and the rights of trial participants, and whom to contact in the event of trial-related injury
- Any foreseeable risks or discomforts to the participant, and when applicable, to an embryo, fetus, or nursing infant
- Any expected benefits or prorated payment to the participant; if no benefit is expected, the participant should also be made aware of this
- Alternative procedures or treatment that may be available to the participant, including a statement on disclosure of appropriate alternative procedures or courses of treatment that might be advantageous to participants when the research involves non-validated procedures, devices, or therapies
- Compensation and/or medical treatment available to the participant or the family or dependents in the event of a trial-related injury
- Any additional costs to the participant that may result from participation in the research
- The extent to which confidentiality records identifying the participant will be maintained, and if the results of the trial are published, the participant’s identity will remain confidential
- That the Pharmacy and Poisons Board (PPB) will be granted direct access to the participant’s original medical records to verify clinical trial procedures and/or data without violating the participant’s confidentiality
- The details on storage and exportation of biological samples, if applicable
- The details on storage and ownership of personal data
- Information about unblinding, if applicable
- The extent of the investigator’s responsibility, if any, to provide medical services to the participant
- That therapy will be provided free of charge for specified types of research-related injury, including the investigators’ responsibilities in this regard
- That participation is voluntary, the participant may withdraw at any time, and refusal to participate will not involve any penalty or loss of benefits, or reduction in the level of care to which the participant is otherwise entitled
- That the participant will be informed about the dissemination of findings and about any publication of the participant’s medical information, including photographs and pedigree charts
- Foreseeable circumstances under which the investigator(s) may remove the participant without consent
- That the participant or legal representative/guardian will be notified in a timely manner if significant new findings develop during the study which may affect the participant’s willingness to continue
- Consent to incomplete disclosure, for example, if it is necessary to inform participants that some information is being withheld deliberately and the reasons for that decision; an offer to disclose the purpose at the conclusion of the study can be made
Note that per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
In addition, the CTRules delineates that if the potential participant is a child, the ICF must also contain these elements:
- The pathophysiology of the disease or subject of the clinical trial
- The methods of diagnosis
- The currently available treatment or prevention strategy in the pediatric population
- The incidence and prevalence of the disease or subject of the clinical trial in the overall population and in the pediatric population
- The evidence and assumptions on key differences between the disease or subject of the clinical trial in the overall population and the pediatric population
In accordance with the Declaration of Helsinki ( KEN-33 ) principles upheld in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), Kenya’s ethical standards promote respect for all human beings and safeguard the rights of research participants. A participant’s rights must also be clearly addressed in the informed consent form (ICF) and during the informed consent process. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
The Right to Participate, Abstain, or Withdraw
As set forth in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and KEN-14 , a participant or legal representative/guardian should be informed that participation is voluntary, that the participant may withdraw from the research study at any time, and that refusal to participate will not involve any penalty or loss of benefits to which the participant is otherwise entitled.
The Right to Information
As delineated in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and KEN-14 , a potential research participant or legal representative/guardian has the right to be informed about the nature and purpose of the research study, its anticipated duration, study procedures, any potential benefits or risks, any compensation for participation or injury/treatment, and any significant new information regarding the research study.
The DPA further indicates that data subjects have a right to:
- Be informed of how their personal data is to be used
- Access their personal data in custody of the data controller (sponsor) or data processor
- Object to the processing of all or part of their personal data
- Correct false or misleading data
- Delete false or misleading data about them
The Right to Privacy and Confidentiality
As per the G-KenyaCT , the G-ECBiomedRes , and KEN-14 , all participants must be afforded the right to privacy and confidentiality, and the ICF must provide a statement that recognizes this right.
The Right of Inquiry/Appeal
The G-KenyaCT , KEN-14 , and the G-ECBiomedRes state that the participant or legal representative/guardian should be provided with contact information for the sponsor and the investigator(s) to address trial-related inquiries. Further, the G-ECBiomedRes requires that the ethics committee contact information also be provided.
The Right to Safety and Welfare
The G-ECBiomedRes and KEN-14 state that a research participant’s right to safety and the protection of the participant’s health and welfare must take precedence over the interests of science and society. KEN-14 upholds the Declaration of Helsinki ( KEN-33 ). (See the Required Elements and Vulnerable Populations sections for additional information regarding requirements for participant rights.)
The G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), make provisions to protect the rights of a research participant during the informed consent process when the procedure is complicated by emergencies. Per the G-KenyaCT , research must be conducted in accordance with KEN-14 . As delineated in the G-KenyaCT and the G-ECBiomedRes , in an emergency, if the signed informed consent form (ICF) cannot be obtained from the research participant, the consent of the legal representative/guardian should be obtained. If the prior consent of the participant or legal representative/guardian cannot be obtained, the participant’s enrollment should follow measures specified in the protocol, and/or elsewhere, to ensure compliance with ethics committee (EC) and the Pharmacy and Poisons Board (PPB) requirements. The G-ECBiomedRes requires that the principle of clinical equipoise be applied, which essentially means the participant is not any worse off by enrolling.
During a public health emergency, the G-KenyaCT stipulates that the informed consent of participants must be obtained in individuals capable of giving informed consent. The CT-Emrgcy includes safeguards to protect clinical trial participants during a public health emergency, including the recommendation to reconsent if there are amendments as a result of the emergency.
Per KEN-14 , in an emergency, if the signed ICF has not been obtained from the participant or legal representative/guardian , or if an effective treatment is lacking but the investigational product could address the participant’s emergency needs, the clinical trial may be conducted. However, the method used on the participant must be explained clearly in the trial protocol, and the EC must approve the protocol in advance. The participant or legal representative/guardian should be informed about the trial as soon as possible, and consent to continue and other consent should be requested, as appropriate.
As per the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), in all Kenyan clinical trials, research participants selected from vulnerable populations must be provided additional protections to safeguard their health and welfare during the informed consent process. Vulnerable populations include those participants with diminished autonomy whose decision to participate in a clinical trial may be unduly influenced by the expectation of benefits associated with participation or by coercion. This may include, but is not limited to, children/minors, pregnant women, neonates, fetuses, medical students, members of the uniformed forces, prisoners, orphans, homeless populations, unemployed, internally displaced persons, economically or educationally disadvantaged persons, marginalized social groups, individuals with terminal illnesses, and the mentally challenged. KEN-14 also includes members of a group with a hierarchical structure, such as medical, pharmacy, dental, and nursing students, subordinate hospital and laboratory personnel, employees of the pharmaceutical industry, members of the armed forces, and persons kept in detention. Other vulnerable subjects include persons in nursing homes, patients in emergency situations, ethnic minority groups, homeless persons, nomads, refugees, minors, and those incapable of giving consent. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
Elderly Persons
The G-ECBiomedRes defines an elderly/senior citizen as a person who has attained the age of 65 years. Their physical or mental state may affect their ability to make voluntary decisions regarding their participation in research projects. Such research involving elderly/senior citizens must comply with the following requirements:
- Strict adherence to ethical principles
- The risk-benefit ratio must be favorable to the research participant
- The participants must be protected from gross violation of human rights
Persons in Dependent Groups
Per the G-ECBiomedRes , research involving data collection by superiors on their subordinates involves relationships such as employer-employee, teacher-students, supervisor-staff, sponsor-dependent, and parent-children. This relationship impairs independent consent by the participants leading to complacency. Therefore, research involving the superior/subordinate relationships must fulfill the following requirements:
- The superior must strictly follow ethical principles to avoid undue pressure
- Subordinates must be protected from gross violation of human rights
- The trial design must be based on a need-to-know principle and improve the conditions of the participants
Persons in Low-Resource Communities
The G-ECBiomedRes provides the following requirements related to conducting research on participants in low-resource settings:
- Persons in such settings should not be involved in research that could be carried out reasonably well in developed communities
- The research should be responsive to the health needs and priorities of the community in which it is to be implemented
- Undue inducement to participate in the research must be avoided at all costs
Armed Forces
The G-ECBiomedRes stipulates that research involving the members of the armed forces may be vulnerable because of the conditions of their service, which may affect their ability to make voluntary decisions regarding their participation in research. Such research must be conducted to ensure that:
- Participants are protected from gross violations of human rights
- There is strict adherence to ethical principles
- There is at least one (1) member of the ethics committee approving such research who is an enlisted and authoritative member of the armed forces
Terminally Ill
Per the G-ECBiomedRes , research involving participants who are terminally ill with an incurable medical condition are vulnerable. Their state may affect their ability to make voluntary decisions regarding their participation in research. Such research can only be conducted when:
- The objectives of the project(s) cannot be achieved using another non-vulnerable group
- The risk-benefit ratio should be favorable to the research participant
See the Children/Minors; Pregnant Women, Fetuses & Neonates; Prisoners; and Mentally Impaired sections for additional information about these vulnerable populations.
According to the G-KenyaCT , a minor is someone under 18 years of age. As set forth in the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), when the research participant is a minor, informed consent should be obtained from the parent/guardian. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 . The informed consent forms, assent forms, and the patient information sheets should be in a language that the parent/guardian clearly understand. All pediatric participants should be fully informed about the trial and its risks and benefits in a language and terms that they are easily able to understand.
Per the G-KenyaCT , a minor should take part in the informed consent procedure in a way tailored to their age and mental maturity. If capable, the participant should sign and personally date the written informed consent. In addition, consent given by pediatric participants should not be considered valid without prior approval by the ethics committee (EC).
The CTRules , the G-ECBiomedRes , and the G-KenyaCT state that a study may only be conducted on minors if several conditions are fulfilled including (Note: Each of the items listed below will not necessarily be found in all sources, which provide overlapping and unique elements):
- Pediatric participants will not be involved in research that might be equally carried out in adults
- The purpose of the research is to generate knowledge relevant to the health needs of children
- The parent/guardian must provide proxy consent and ensure assent has been obtained to the extent of the child’s capabilities. However, if the minor refuses to participate after proxy consent is given, the minor’s refusal must be respected unless there is no other medical alternative from which the minor could benefit
- The risk presented by interventions not intended to benefit the minor is low and commensurate with the importance of the knowledge to be gained
- Interventions that are intended to provide therapeutic benefit are likely to be at least as advantageous to the individual child as any available alternative
- No incentives or financial inducements are given to the participant or parent/guardian except to provide compensation for expenses and loss of earnings directly related to the participation in the trial
Additionally, per the G-KenyaCT , the trial should also address the following considerations:
- Provide useful answers to the study population
- The medicine satisfies a need for the population being studied
- Children are adequately monitored and protected
- If there is no direct benefit to the child, or there is no more than minimal risk to the participant(s)
- Trial results will be published
- End-of-trial treatment provisions will be made
Assent Requirements
As delineated in the G-KenyaCT , before undertaking research involving children, the investigator must ensure that the agreement (assent) of each child has been obtained to the extent of the child’s capabilities, and a child’s refusal to participate or continue in the research must be respected. Assent is defined as a child’s affirmative agreement to participate in research, where the child is below the age of the majority but old enough to understand the proposed research in general, its expected risks and possible benefits, and the activities expected of them as participants. The G-ECBiomedRes provides that in children above seven (7) years and below 18 years where the parent(s)/guardian(s) gives proxy consent, assent must be obtained from the child.
For an example of an accredited EC’s assent requirements, see the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee ’s sample minor assent form ( KEN-17 ).
Per the G-KenyaCT , research must be conducted in accordance with the requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). In accordance with KEN-14 , informed consent requirements for conducting clinical trials with pregnant or nursing women or fetuses follow the general requirements listed in the Required Elements section . Specifically, the informed consent form should include a statement on the reasonably foreseeable risks or inconveniences to the participant, and when applicable, to an embryo, fetus, or nursing infant.
As per the G-ECBiomedRes , research involving pregnant, lactating, and breastfeeding women may pose compromised long-term outcomes for the child. In addition, potential parent(s) can make decisions on behalf of the fetus(es), embryo(s), and zygote(s).
For fetal, embryo, and zygote(s) cases, research should be limited as follows:
- Cases that present no harm or offer assistance to the life system of the participants
- No procedures should be permitted that are likely to harm them
- A fetus ex-utero and alive, embryo, and zygote must not be involved in research unless it is intended to enhance the life of that fetus, embryo, and zygote or unless the research involves no risk to them
Additionally, the following guidelines must be followed for research involving pregnant, lactating, and breastfeeding women:
- The research carries no more than minimal risk to the fetuses or nursing infants
- Pregnant or nursing women should generally not be clinical trial participants except where such trials are designed to protect or advance the health of the pregnant/nursing women or fetuses/nursing infants, and for which women who are not pregnant or nursing would not be suitable participants
- The justification for such research should be that participants must not be arbitrarily deprived of the opportunity to benefit from investigational drugs, vaccines, or other agents that promise therapeutic or preventive benefits
Per the G-ECBiomedRes and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), prisoners are considered vulnerable because incarceration could affect their ability to make a voluntary decision regarding participation in research. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 . A research study involving prisoners should ensure that these prospective participants are informed and given the opportunity to make their own decisions without any interference or reprisals from a higher authority. The ethics committee must also ensure that the study will be independently monitored to assure the dignity and rights of the prisoners involved in the research.
As per the G-ECBiomedRes and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), an ethics committee (EC) within the relevant institution must approve the participation of adult research participants who are incapable by reason of physical and mental capacity to give consent. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
In addition, as delineated in the G-ECBiomedRes , a research study may involve participants with mental incapacities or behavioral disorders under the following conditions:
- Such research could not be carried out equally well with individuals who are in possession of their full mental faculties
- The knowledge gained would be relevant to the health needs of persons with mental or behavioral disorders
- The participant’s consent has been obtained to the extent of the participant’s capabilities, and a prospective participant’s refusal to participate is always respected
- In the case of incompetent individuals, informed consent shall be obtained from a legal guardian or other duly authorized person
- The degree of risk attached to the intervention not intended to benefit the individual participant is low and commensurate with the importance of knowledge to be gained
- Interventions that are intended to provide therapeutic benefit are likely to be at least as advantageous to the individual participant as any alternative
The G-KenyaCT defines an investigational product (IP) as any pharmaceutical product, including a new product or existing product for a new indication, in the form of an active ingredient or placebo being tested or used as a reference in a clinical trial, including a product with a marketing authorization when used or assembled (formulated or packaged) in a way different from the approved form, or when used for an unapproved indication, or when used to gain further information about an approved use.
Manufacturing
According to the PPA and the G-KenyaCT , the Pharmacy and Poisons Board (PPB) is responsible for authorizing the manufacture of all drug products, including investigational products (IPs) in Kenya. Per the CTRules and the G-KenyaCT , an IP must be manufactured in accordance with the requirements of good manufacturing practice (GMP). The CTRules requires a sponsor to immediately notify the PPB in writing when a pharmaceutical or chemical alteration may affect the quality, safety, or efficacy of the IP product during an ongoing clinical trial. The G-KenyaCT states that the sponsor must submit the IP dossier directly to the PPB or may submit it through the principal investigator. The IP dossier must be prepared as per the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), which is required per G-KenyaCT . The manufacture of IPs may be subject to GMP inspection by the PPB in the same way as in the case of marketed drug products. See the G-KenyaCT for detailed chemistry and manufacturing information to be provided to the PPB if the IP has not been registered with the PPB.
KEN-14 also requires IPs to be manufactured, handled, and stored in accordance with applicable GMPs and used in accordance with the approved protocol.
Per the PPA , the PPB is authorized to regulate the manufacturing of medicine, including:
See the KenyaGMP , for PPB’s compilation of recommended World Health Organization GMP guidelines to help comply with GMP requirements and prepare for an inspection, including for manufacture of IPs.
Per the PPA and the ImpExp , the PPB is authorized to regulate the import and export of health products and technologies, including IPs. As per the ImpExp and the G-KenyaCT , to obtain an import permit for a clinical trial, the sponsor or investigator must submit an application online to the Kenya Trade Network Agency’s Kenya TradeNet Single Window System ( KEN-28 ). The following documents must be submitted (Note: Each of the items listed below will not necessarily be found in both sources, which provide overlapping and unique elements):
- The proforma invoice or invoice
- The ethics committee favorable opinion letter
- The Expert Committee on Clinical Trials approval letter from the PPB
- Registration of the institution where the research is being undertaken
The G-KenyaCT states that the sponsor must submit to the PPB a copy of the endorsed clinical trial import permit and/or evidence of delivery to the approved investigator(s)/trial center(s) on importation and supply of each consignment of the product. The product must only be supplied to the investigator(s) at the trial site(s) named in the clinical trial import license application for the purpose and use as stated in the said application. Prior PPB notification and approval is required for changes in the investigator, trial site, or protocol. The sponsor must inform PPB of any change in information, or any information received that casts doubt on the continued validity of the data, which was submitted with, or in connection with the application for the import permit. The sponsor must also inform the PPB of any decision to discontinue the trial to which the permit relates and state the reason for the decision. See KEN-8 for additional details on the procedures for obtaining an import license.
Per the CTRules , the import of an IP must comply with the applicable regulatory requirements to ensure integrity and accountability of the products. The PPB may revoke or suspend an import permit if the IP was manufactured in conditions not consistent with GMP; if the clinical trial was discontinued; or if the sponsor provided false information.
Please note: Kenya is party to the Nagoya Protocol on Access and Benefit-sharing ( KEN-3 ), which may have implications for studies of IPs developed using certain non-human genetic resources (e.g., plants, animals, and microbes). For more information, see KEN-15 .
Investigator’s Brochure
In accordance with the CTRules and the G-KenyaCT , the sponsor must provide an up-to-date investigator’s brochure (IB). An updated IB and Drug Safety Update Report (DSUR) must be submitted whenever available but at least once year as a notification to the Pharmacy and Poisons Board (PPB) or when there are substantial changes to the previous version.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As specified in the G-KenyaCT and KEN-14 , the IB must provide coverage of the following areas:
- Physical, chemical, and pharmaceutical properties
- The pharmacological aspects including its metabolites in all animal species tested
- The pharmacokinetics and metabolism including its biological transformation in all animal species tested
- Toxicological effects in any animal species tested under a single dose study, a repeated dose study, or a special study
- Results of clinical pharmacokinetic studies
- Information regarding safety, pharmacodynamics, efficacy, and dose responses that were obtained from previous clinical trials in humans
The G-KenyaCT indicates that the sponsor must also follow the guidance contained in KEN-14 .
Quality Management
In accordance with the G-KenyaCT , a good manufacturing practice (GMP) certificate must be provided by a competent authority from the country of manufacture to the PPB in the clinical trial application. At a minimum, the GMP certificate should include the competent authority’s name and contact details, address of the manufacturing site, date of inspection, and validity period. Certificates of Analysis (CoAs) must also be provided to the PPB for all investigational products (IPs) and comparator products. Per KEN-14 , the sponsor must maintain a CoA to document the identity, purity, and strength of the IP(s) to be used in the clinical trial.
See the G-KenyaCT for detailed chemistry and manufacturing information to be provided to the PPB if the IP has not been registered with the PPB. In addition, see Cert-Emrgcy for information about good clinical practice (GCP) and GMP certifications during emergencies.
(See Product Management section for additional information on sponsor requirements).
Per the G-KenyaCT , investigational products (IPs) used in Kenyan clinical trials must be properly labelled. A final copy/version of the labelling must be submitted to the Pharmacy and Poisons Board (PPB) for approval and should contain the following minimum information:
- Statement indicating that the product is for “clinical trial purpose only”
- Recommended storage conditions
- Protocol code or identification
- Name, address, and telephone number of the sponsor, contract research organization, or investigator (the main contact for information on the product, clinical trial, and emergency unblinding)
- Pharmaceutical dosage form, route of administration, quantity of dosage units, and in the case of open trials, the name/identifier and strength/potency
- The batch and/or code number to identify the contents and packaging operation
- A trial reference code allowing identification of the trial, site, investigator, and sponsor, if not given elsewhere
- The trial participant identification number/treatment number and, where relevant, the visit number
- The name of the investigator (if not included above)
- Directions for use (reference may be made to a leaflet or other explanatory document intended for the trial participant or person administering the product)
- Period of use (use-by date, expiry date, or re-test date as applicable), in month/year format and in a manner that avoids any ambiguity
- The complete physical address of the manufacturing site
As indicated in the G-KenyaCT , it is recommended that an IP is not re-labeled wherever possible. It is, however, accepted that in certain cases it is necessary to re-label and the PPB will review applications for the extension of expiration dates based on sufficient evidence being provided by the applicant that an extended expiration date is warranted. A written justification and evidence should be provided to the PPB. Any re-labelling of remaining IPs from previously manufactured batches must be performed in accordance with good manufacturing practice (GMP) principles and is limited to an extension of the expiration date where sufficient evidence is available to support such extension. Any request for re-labelling should be accompanied by a certificate of analysis of the product from a PPB-recognized laboratory or World Health Organization (WHO) prequalified laboratories ( KEN-18 ). After approval, the re-labelling must be carried out under the supervision of a pharmaceutical inspector on the ground. In case of use-date extension, an additional label should be affixed to the IP to indicate the new use date and repeat the batch number. It may be superposed on the old use date, but not on the original batch number. PPB will not approve re-labelling of a product if the proposed additional label obscures the original labelling. At all times, the original label should be visible. This operation may be performed onsite by the clinical trial monitor(s) or the clinical trial site pharmacist, in accordance with specific and standard operating procedures. The operation should be checked by a second person. Documented evidence of this additional labelling should be available in the trial documentation and in the batch records. KEN-34 indicates that all documents submitted to the PPB in a clinical trial application should be in English, including a pictorial sample of the IP with the labeling text.
The International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), which the G-KenyaCT requires following, states that the IP must be coded and labeled in a manner that protects the blinding, if applicable. The IPs must also be suitably packaged in a manner that will prevent contamination and unacceptable deterioration during transport and storage.
Supply, Storage, and Handling Requirements
Per the PPA , the Pharmacy and Poisons Board (PPB) is responsible for the regulation of investigational products (IPs), including all matters relating to the safety, packaging, and distribution of medicines. The PPB must ensure that all medicinal products manufactured in, imported into, or exported from the country conform to prescribed standards of quality, safety, and efficacy. Further, the PPB must ensure that the personnel, premises, and practices employed in the manufacture and storage of IPs complies with prescribed requirements.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As defined in the G-KenyaCT and KEN-14 , the sponsor must ensure the following (Note: Each of the items listed below will not necessarily be found in both sources, which provide overlapping and unique elements):
- Timely delivery of IPs to the investigator(s)
- Records that document shipment, receipt, disposition, return, and destruction of the IPs are maintained
- A system for retrieving IPs and documenting that this retrieval is maintained
- A system for the disposition of unused IPs is maintained
- Steps taken to ensure that the IPs are stable over the period of use
- Sufficient quantities of the IPs used in the trials are maintained
To the extent stability permits, samples should be retained either until the analyses of the trial data are complete or as required by the applicable regulatory requirement(s), whichever represents the longer retention period.
As defined in the G-KenyaCT and KEN-14 , the sponsor must also supply the investigator(s)/institution(s) with the IPs, including the comparator(s) and placebo, if applicable. The sponsor or the representative should not supply either party with the IP(s) until approval from the PPB and a favorable opinion letter from the local and national ethics committees (ECs) are obtained. In addition, the G-KenyaCT requires the following supply, storage, and handling processes:
- Analysis or evaluation of samples is performed in accordance with the protocol and, where applicable, the contract/agreement, the work instruction, and associated methods
- Adherence to the laboratories, policies, and standard operating procedures (SOPs)
- Prior to the initiation of sample analysis or evaluation, it is often necessary to prepare a work instruction detailing the procedures, which will be used to conduct the analysis or evaluation
- Regularly maintain all the equipment, including point-of-care equipment
- Have written procedures for all assays, and validate the assays
- Have a stock control procedure to make sure that reagents and consumables are used within their expiry dates
- Keep records, including source documents and final reports
- Have a laboratory information management system, and validate and backup the system
- Provide protective clothing and safety equipment for staff
The G-KenyaCT also states that the sponsor must submit to the PPB a copy of the endorsed Clinical Trial Import License and/or evidence of delivery to the approved investigator(s)/institution(s) upon importing and supplying each product consignment. In addition, the IP must only be supplied to the investigator(s)/institution(s) named in the application for the Clinical Trial Import License/Clinical Trial Exemption for the purpose and use specified. The sponsor must inform the PPB in the event of any information changes including:
- Information the sponsor receives that casts doubt on the continued validity of the submitted data
- Information associated with the Clinical Trial Import License
See the G-KenyaCT for additional information on principal investigator requirements relating to the Clinical Trial Import License.
Record Requirements
As per the G-KenyaCT , the sponsor is required to maintain records that document IP(s) shipment, receipt, disposition, return, and destruction. The sponsor must also maintain a system for retrieving IPs and documenting this retrieval, and maintain a system for the disposition of unused IPs.
According to the G-KenyaCT , IP manufacturers or importers must also retain samples for each batch of bulk product, and the packaging components used for each finished batch, for at least two (2) years following the trial. The sponsor should maintain sufficient samples from each batch and keep a record of their analyses and characteristics for reference so that, if necessary, an independent laboratory could reconfirm the same data.
Specimens are not defined in the Kenyan regulations. However, per KEN-26 , the Kenya Medical Research Institute (KEMRI) identifies biological samples and specimens as including, but not limited to, blood samples, saliva, breast milk samples, mosquito parts samples, biological cultures, tissue and tissue samples, hair samples, human stool, and environmental samples used in human health research.
Import/Export
Per the G-ECBiomedRes , biological material must not be imported nor exported without proper justification and authorization, which includes a signed material transfer agreement (MTA) approved by the relevant institutions and deposited with the National Commission for Science, Technology and Innovation (NACOSTI) . For exports, a Kenyan investigator must be included in the team that is conducting the research in the recipient country. All biological samples and data collected during research belong to the local participating institutions and country.
In addition, KEN-37 has indicated that Kenya’s Pharmacy and Poisons Board (PPB) will approve of an export for overseas research if the following requirements are met:
- PPB initial approval letter or annual approval letter
- Ethics committee (EC) approval letter
- Study protocol with a summary justification for the participants' sample exportation
- Informed consent form that highlights the areas where study participants are informed about the exportation of their samples
The G-KenyaCT states that in the case of transfer of materials during research involving children, the sponsor or the representative or the principal investigator should provide to the EC an MTA including, but not limited to, the following information:
- Identification of the provider and recipient
- Definition of the trial and how the material will and will not be used
- Maintenance of confidentiality of background of supporting data or information, if any
- Indemnification and insurance
In addition, KEN-26 provides an example of the Kenya Medical Research Institute (KEMRI) 's procedures for handling requests to ship biological samples or specimens. KEN-17 also provides an example of an MTA form from the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee .
Detailed information is currently unavailable regarding Kenya’s Pharmacy and Poisons Board (PPB) ’s requirements for obtaining informed consent from participants prior to collecting, storing, or using their biological sample(s). However, the G-KenyaCT states that for research involving children, the sponsor or the representative or the principal investigator should provide examples of patient information leaflets and informed consent forms (ICF) to the ethics committee (EC) for any proposed archiving of biological specimens for later research, or for genetics research.
The G-ECBiomedRes requires that participants are made aware of the use of personal data through informed consent, including secondary data and biological material in biobanks. The secondary use of data requires approval by an accredited EC. The investigator must obtain consent from the participants for the new study. For situations where this is not practicable, the relevant accredited EC can approve a waiver of individual consent following confirmation that the participants had previously consented to storage of the biological samples/data, and that this data is delinked from personal identifiers. In cases where the sample is stored in a foreign institution, the collaborating EC should also conduct its own deliberation. Researchers sending samples abroad must ensure that consent for transfer of materials was obtained during collection of the samples and that the collaborating EC gave approval.
See KEN-4 for Kenya Medical Research Institute (KEMRI) 's sample ICF that includes guidance on specimens. As another example, see KEN-17 for the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee ’s form and guidance on genetic research and biobanking.
See the Required Elements and Participant Rights sections for additional information on informed consent.

CENTRE FOR PUBLIC HEALTH RESEARCH (CPHR) NAIROBI
Staff profiles.

Before a formal transfer to KEMRI, CPHR operated by the name of Medical Research Centre (MRC), which was managed by the Royal Tropical Institute of Amsterdam (KIT) until 1987. In 1995, KEMRI undertook a re-alignment exercise of its research mandates / Programmes and renamed its centers to reflect the new corporate identity. In this regard, MRC remained the official name of the center until 1997 when all tittles of centers were changed to start with CENTRE and MRC renamed the “Centre for Public Health Research”.
The Public Health Research Centre is responsible for undertaking research in epidemiology, public health nutrition, maternal and child health, health systems research, population and behavioral sciences, environmental, occupational and industrial health, and oral health and non-communicable diseases.
Our mission is to improve human health and quality of life through research, capacity building, innovation and service delivery
EdApoteket är en professionell och pålitlig klinik online som verkar på den europeiska marknaden, ihållande huvudvärk eller svimning. Det har blivit möjligt att använda ett preparat för att förbättra https://edapoteket.com/viagra/ styrkan och att övervinna problem av kvinnor i den sexuella sfären kan Cialis lösa sexuella problem på grund av psykologisk och emotionell impotens. Läkemedlet Vardenafil producerades av det indiska företaget Cipla.
- To conduct research aimed at providing solutions for the reduction of diseases of public health importance
- To undertake innovations in products formulation and provision of specialized service delivery for promotion of public health
- To strengthen capacity in public health research through training, supervision and mentorship
- To translate and disseminate health research findings for evidence-based policy formulation and implementation for improved public health.
- To provide leadership in public health research in Kenya and beyond
- To conduct research on Universal Health Coverage
- To conduct research on human food security and nutrition
- To conduct Research on Health systems
- To conduct research on environmental and occupational health
- To conduct research on mental health/substance abuse
Achievements
| Kakamega ORS and social marketing | Charcoal based water filter ( ) | |
| Development of non-fluoride tooth paste for children | Non fluoride toothpaste; Changed utilization of fluoride toothpaste by children; Fluorosis in children reduced | |
| Effectiveness of in water de-fluoridation | Small scale de- fluoridation of water treatment plants; Reduction of fluoride levels in water and prevalence of fluorosis |
Public Health Nutrition and Maternal and Child Health
Nutrition studies and survey :.
- Conduct of national nutrition surveys and studies on Maternal Child Health and Public Nutrition.
- Undertake clinical trials and studies on innovative nutritional preparations/formulations to address disease conditions
- Conduct studies on nutrition and lifestyle diseases including but not limited to cardiovascular health research, diabetes and cancer.
Wellness promotion: Provision of wellness promotion services at work site for different institutions in the country
Ongoing Projects
- ICCA – KEMRI Project
COMING SOON
Health Systems Research Division
To conduct research that will identify effective and efficient ways to organize, manage, and deliver high quality, equitable and responsive health care within the areas of health services, health information systems, health financing, medicines and technologies, health workforce, and leadership and governance in Kenya.
Public Health Nutrition, Matenal and Child Health Division
To conduct research in public health, nutrition, maternal and child health, and food science including studies on dietary intake and food safety
Epidemiology Division
To conduct research and studies on disease patterns, undertake surveillance and monitoring
Populational and Behavioral Science Unit
This Unit focuses on research that affects Kenya population as well as behavioral sciences with the sole aim of promoting optimal physical, social, and emotional wellness
Oral Health Division
This unit focus on the assessment of oral health needs. Carry out critical evaluations, derivation of appropriate indicators oral health, commissioning and evaluation of dental health services. Research and development in oral health.
Environmental Occupational and Industrial Health Division
To undertake research in environmental, occupational and industrial health
Socio-Sciences Unit
Social Sciences Research arm is an independent Unit in the Centre for Public Health Research, KEMRI that provides broad research endeavors in the social sciences, along with research skills related to health, illness and health care.
The research in this discipline is conducted by social scientists following a systematic plan that utilizes both quantitative and qualitative designs. The quantitative design approaches social phenomena through quantifiable evidence and often relies on statistical analysis of many cases (or across intentionally designed treatments in an experiment) to create valid and reliable general claims related to quantity.
Qualitative design, on the other hand, emphasize understanding of social phenomena through direct observation, communication with participants, or analysis of texts, and may stress contextual subjective accuracy over generality. Reasons for social research ankers on identifying general patterns and relationships, testing and refining theory, making predictions, interpreting significance, exploring diversity, giving voice, and advancing new theories.
The Social Science Unit comprises various skills visa vis Medical Sociology, Sociology, Anthropology, Demography, and Psychology. Its functions include carrying out research that ensures excellence in research and innovation for human health, strengthening disease-based research, enhancing dissemination and translation of research findings for evidence based policy formulation and implementation, and mentoring programmes.
LABORATORY DIVISIONS
Hematology laboratory.
Hematology is concerned with the diagnosis of diseases related to blood. The laboratory work that goes into the study of blood is frequently performed by a medical technologist or medical laboratory scientist. Including analysis of factors concerned with oncology
Parasitology Laboratory
Parasitology laboratory offers a referral service for the identification of a wide range of human parasites from clinical specimens. Examples of tests include Blood Parasite diagnosis: Malaria, African Trypanosomes and Filariasis, Faecal Parasite diagnosis:
Faecal microscopy direct examination and / or concentration for parasites (including hot stool), Culture for Strongyloides /Hookworm, Faecal staining methods, Enterobius microscopy
Nutrition biochemistry Laboratory
To explores the chemical processes within and related to living organisms. Mainly to establish the optimal dietary and nutritional requirements of both healthy individuals and those inflicted with illness.
Fourier Transform Infrared Spectrometry IFTIR Laboratory
Specialized laboratory, equipment supported by International Atomic Energy Agency the second one in Kenya, the other one is in UoN. Assesses intake of human milk, in breastfed infants using stable Isotope Techniques (deuterium)
Food Science Laboratory
Uses the application of basic sciences and engineering to study the physical, chemical, and biochemical nature of foods and the principles of food processing including the study of microorganisms causing food spoilage
| DOCUMENT NAME | DOWNLOAD |
|---|---|
| Access to Cancer Care in Kenya: Patients’, Survivors’, Caregivers’ and Health Providers’ Perspectives | |
| Global report on the state of dietary data | |
| A working guide for Urban Food Listing Food listing for processed packaged and vendor-prepared foods in urban centers for use in 24-hour dietary recall surveys |

Dr. Zipporah Bukania
Deputy director cphr.
Dr. Bukania is a trained public health nutrition scientist with over 20 years’ experience in clinical nutrition services and research. Expert in designing and executing assignments focusing majorly on generating evidence to support implementation of nutrition related Programmes in the communities. Equally impressive history of spearheading nutrition research initiatives ranging from household surveys, stakeholders’ analyses studies, randomized controlled trials and implementation research, strategy development, Review of policy documents. She has hands on experience in translation of research findings to policy documents.
Through various working Groups, Dr Bukania provides technical supports to the Ministry of Health, Division of Nutrition and Dietetics (DND). Currently, Chairs the Scaling Up Nutrition Academia and Research Network, and a Secretariat Member of the Scaling Up Nutrition Movement in Kenya. She also chairs the DND Research in Nutrition Technical Working Group. Further, she plays an advisory role to the Livestock for Health (L4H) program of the Food and Agriculture Organization of the United Nations. In addition, Dr. Bukania is a member of the Global Food Matters Expert Group.
View all Staff Profiles

Contact Info
Centre for Public Health Research
P.O. BOX 20752-00202, KNH Nairobi, Kenya
Email: directorcphr obfsctd @kemri.go.ke
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Nursing and midwifery research priorities for Kenya: Results from a national Delphi survey
Affiliations.
- 1 Dean, School of Nursing, Jomo Kenyatta University of Agriculture & Technology, Nairobi, Kenya.
- 2 Chair, Department of Nursing Sciences, University of Nairobi, Nairobi, Kenya.
- 3 Director of Research and Innovation, St. Paul's University, Limuru, Kenya.
- 4 Professor Emerita, Nelda C. Stark College of Nursing, Texas Woman's University, Denton, USA.
- 5 Associate Dean for Research and Professor, Mark and Robyn Jones College of Nursing, Montana State University, Bozeman, USA.
- PMID: 37837277
- DOI: 10.1111/inr.12893
Background: The International Council of Nurses and the World Health Organization have prioritized evidence-based nursing and midwifery practice derived from nurse-led research. However, in a low-resource country like Kenya, there is a need to identify research priorities to optimize utilization of limited existing research infrastructure and funding. Kenya lacks a nursing and midwifery research strategy to guide research prioritization.
Introduction: The goal of this study was to identify and describe nursing and midwifery research priorities for Kenya.
Methods: A cross-sectional Delphi survey using two iterative rounds of electronic data collection was used to reach a consensus about priorities for nursing and midwifery research in Kenya. NVivo-12 was used to analyze the qualitative data to identify categories, sub-themes, and themes; descriptive statistics were used to analyze quantitative data.
Results: Participants included 159 nurse managers, administrators, and educators representing regional, county, and national referral, private, and faith-based hospitals, nurse training schools, research institutions, and nursing organizations in Kenya. Staffing challenges, motivation, remuneration, and funding for higher education were ranked as the top critically important issues using a cutoff point of ≥ 70% agreement.
Conclusion: There is a need for the development of a National Framework for Nursing and Midwifery Research Priorities in Kenya to guide research that builds excellence in meeting nursing and midwifery human resource concerns and ultimately improves patient care practices and outcomes.
Implications for nursing and nursing policy: The objective of Kenya's health goals delineated within three key national health documents cannot be attained without adequate numbers of nursing and midwifery professionals and policies that address nursing and midwifery staffing challenges, remuneration for employment, and improved funding for higher education.
Keywords: Delphi method; Kenya; midwifery research; midwives; nurses; nursing research; research priorities.
© 2023 The Authors. International Nursing Review published by John Wiley & Sons Ltd on behalf of International Council of Nurses.
PubMed Disclaimer
Similar articles
- Clinical Nursing and Midwifery Research Priorities in Eastern and Southern African Countries: Results From a Delphi Survey. Sun C, Dohrn J, Klopper H, Malata A, Omoni G, Larson E. Sun C, et al. Nurs Res. 2015 Nov-Dec;64(6):466-75. doi: 10.1097/NNR.0000000000000126. Nurs Res. 2015. PMID: 26505159
- Delphi Survey of Clinical Nursing and Midwifery Research Priorities in the Eastern Mediterranean Region. Sun C, Dohrn J, Oweis A, Huijer HA, Abu-Moghli F, Dawani H, Ghazi C, Larson E. Sun C, et al. J Nurs Scholarsh. 2017 Mar;49(2):223-235. doi: 10.1111/jnu.12280. Epub 2017 Feb 8. J Nurs Scholarsh. 2017. PMID: 28178398
- Utilization of Research in Clinical Nursing and Midwifery Practice in Ghana: Protocol for a Mixed Methods Study. Owusu LB, Scheepers N, Tenza IS. Owusu LB, et al. JMIR Res Protoc. 2023 Apr 7;12:e45067. doi: 10.2196/45067. JMIR Res Protoc. 2023. PMID: 37027196 Free PMC article.
- Scopes of practice for advanced practice nursing and advanced practice midwifery in Kenya: A gap analysis. Ndirangu-Mugo E, Kimani RW, Onyancha C, Mutwiri BD, May B, Kambo I, Tallam E, Koech N, Mukuna A, Henderson C, Shumba CS. Ndirangu-Mugo E, et al. Int Nurs Rev. 2024 Jun;71(2):276-284. doi: 10.1111/inr.12947. Epub 2024 Mar 15. Int Nurs Rev. 2024. PMID: 38488333 Review.
- Critical care nursing policy, practice, and research priorities: An international cross-sectional study. Williams G, Fulbrook P, Alberto L, Kleinpell R, Christensen M, Sitoula K, Kobuh ND. Williams G, et al. J Nurs Scholarsh. 2023 Sep;55(5):1044-1057. doi: 10.1111/jnu.12884. Epub 2023 Mar 9. J Nurs Scholarsh. 2023. PMID: 36894518 Review.
- Nurses' and midwives' participation and utilization of health-related research in Kenya: Implications for evidence-based practice. Nzengya DM, Mutisya AK, Wagoro MCA, Secor-Turner M, Edwards J. Nzengya DM, et al. Int J Nurs Sci. 2023 Mar 7;10(2):199-205. doi: 10.1016/j.ijnss.2023.02.001. eCollection 2023 Apr. Int J Nurs Sci. 2023. PMID: 37128489 Free PMC article.
- Atieno, W.M.C. et al. (2020) Development of a graphic blood glucose monitoring chart for glycaemic control in diabetes mellitus: a modified Delphi method study. Journal of Research in Nursing, 25, 323-344. https://doi.org/10.1177/1744987119836135
- Al-Yateem, N. et al. (2019) Nurse-identified patient care and health services research priorities in the United Arab Emirates: a Delphi study. BMC Health Services Research, 19. https://doi.org/10.1186/s12913-019-3888-5
- Centers for Disease Control (CDC). (2022) CDC in Kenya. Available at: https://www.cdc.gov/globalhealth/countries/kenya/default.htm [Accessed 15th May 2021].
- Gathara, D. et al. (2020) Developing metrics for nursing quality of care for low- and middle-income countries: a scoping review linked to stakeholder engagement. Human Resources for Health, 18, 1-16. https://doi.org/10.1186/s12960-020-00470-2
- Government of the Republic of Kenya. (2007) Kenya vision 2030. Nairobi: Ministry of Planning and National Development. Available at: http://vision2030.go.ke/wp-content/uploads/2018/05/Vision-2030-Popular-V... [Accessed 17th December 2022].
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Observatory
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Feature stories /
Strengthening the availability of evidence and fostering dialogue to stimulate investment in Kenya's health workforce

Staff at Railways Health Centre have seen a great improvement in their health workforce. Over five years the facility has expanded from 10 to 30 staff members, reflecting the broader national initiative to enhance healthcare delivery through strategic workforce development. Health workers are fundamental to strong health systems, and to progress towards universal health coverage.
This was due to sustained interventions by government and its partners to improve the availability of health workers to deliver health services across the country.
According to the Kenya’s Health Labour Market Analysis 2023 , which was conducted with technical and financial support from WHO, Kenya has doubled its health workforce in the last 10 years. This includes nurses, midwives, doctors, clinical officers and other trained professionals.
Improved availability of health workers at healthcare facilities across Kenya has significantly enhanced patient care, leading to an increase in individuals seeking treatment and improved quality of care offered at the health facilities nationwide.

The Government of Kenya has been using data, evidence, and multi-stakeholder dialogues to identify and implement strategic interventions to address its health workforce challenges. This supported the strategic investment needed in implementing the Kenya Human Resources for Health (HRH) Strategy 2019-2023, which is the foundation on which WHO supports the Kenyan Ministry of Health.
“To effectively use the investments made in the health sector as part of the UHC journey, there is need for a fit-for-purpose health workforce with appropriate skills mix and adequate number,” said Dr Sultani Matendechero, Acting Deputy Director General, Ministry of Health, Kenya
Improving data availability and quality for decision-making
Since 2020, with support from the UHC Partnership , WHO has provided technical and financial support to strengthen the availability of and use of data for health workforce strategic planning and health workforce management at national and county levels.
“It is my sincere hope that the findings of the health labour market analysis will provide evidence-based recommendations that will inform the Human Resources for Health policy and further improve the health care services in the country. I encourage you all to utilize the findings for decision-making, planning and programming,” said Dr Patrick Amoth, Director General, Ministry of Health, Kenya.
Engagement through multi-stakeholder national dialogue
WHO, through the UHC Partnership and United Kingdom Department of Health and Social Care (DHSC) – Global Health Workforce Programme, supported the Kenya Health Human Resources Advisory Council (KHHRAC) to hold a National Dialogue on Strengthening Health Workforce Development and Management. This dialogue convened stakeholders from national and county governments and public and private sectors that work directly with the health workforce or in related sectors such as education.
During the two days dialogue, over 100 participants including policymakers, health workers’ labour unions, professional associations, training institutions, and health workers themselves engaged in discussions to identify challenges and solutions including what has worked well in the past.
The dialogue culminated with the signing of the Kericho National Declaration on Health Workforce with resolutions and actions to be implemented by the Ministry of Health and stakeholders over two years. If translated effectively into investments and policies, the Kericho Declaration can significantly advance Kenya's efforts towards achieving Universal Health Coverage.
“Kenya is demonstrating its commitment to achieving health for all through decisive action, with health workers serving as the backbone of the health system. The points that emerged from the national dialogue provide significant milestones to ensure that UHC becomes a reality,” said Dr Diallo Abdourahmane, WHO Representative to Kenya.
The UHC Partnership operates in over 125 countries, representing over 3 billion people. It is supported and funded by Belgium, Canada, the European Union, France, Germany, Ireland, Luxembourg, Japan, the United Kingdom of Great Britain and Northern Ireland, and WHO.
Primary health care
Universal health coverage
UHC Partnership
Read more stories about WHO’s impact across the world
Read more about WHO contributors
Read more on flexible funds for a strong, agile and independent WHO
Shopping Cart
No products in the basket.

290+ Nursing Research Topics & Project Ideas for College Students in Kenya
Every college student dreads the process of coming up with a novel nursing project idea. It takes a lot of brain power to put together a research project that will wow the professors and earn you excellent grades. That is why I have put together this list to help you narrow down your search and come up with an excellent project topic regardless of your area of specialization.
Nursing Leadership Project Ideas for College Students in Kenya
- Nurse leadership: Passion or Duty?
- Role of transformational leadership among nurse managers
- Significance of communication among interprofessional team nurse leaders
- Management styles in nursing
- Improving nursing leadership skills
- Interview with a nurse leader
- Strategies to Address the Shortage of Respiratory Therapists and Ventilators during Disaster (Covid19 Pandemic Case Study)
- Strength and weaknesses of charge nurses
- Importance of charismatic leadership among nurse leaders
- The stress management approach for nurse leaders
- The role of charismatic leadership among nurse leaders
- A comprehensive study of the problems facing modern nurse leaders
- Effective use of organizational tactics to motivate healthcare personnel
- Professional development strategies for nurses
- Importance of ethical practice among nurse leaders
- Impact of nurse leadership on patient outcomes
- Significance of nurse leadership
- What is leadership from a nursing perspective?
- Long term and short-term goals for clinical leaders
- Theories that support nurse leadership
- Importance of nurse leaders in quality improvement projects
- How nurse leaders can initiate and manage change
- The link between nurse leadership and change management
- Impacts of nurse engagement and inclusion on patient outcomes
- Organizational strategies nurse leaders can use to motivate the healthcare personnel
- Challenges facing contemporary nurse leaders
- Role of nurse leaders in solving conflicts in clinical settings
- Nurse leaders as patient advocates
- Role of nurse leaders in preventing violence in emergency rooms
- How nurse leaders can address burnout among nurses
- Importance of having a personal leadership philosophy as a nurse leader
- Leadership in the Kenyan Health system
- Influential nurse leaders in the political space
- Role of nurse managers in healthcare
- Nurse leadership qualities and behavior
- Traits of a great nurse leader
- Comparing and contrasting nurse leadership roles in private and public hospitals.
- Difference between accountability among nurse leaders in developed nations and developing nations
- Nurse leaders as change agents in healthcare settings
- Effective nursing leadership styles
- Leadership in nursing education
- Student nurses and leadership
- Top qualities of a great nurse leader
- Evaluation of leadership qualities the deliver excellence in a nursing setting
- Productivity of nurse leaders in public versus private hospitals
- Emergency room conflict and the role of nurse leaders in resolving it
- Effective strategies charge nurses can implement in addressing stress and burnout among nurses
- Role of nurse leaders in shaping public policy
- Leadership characteristics that represent excellence
- Defining leadership in nursing
- Training plan for nurse leaders
- Transactional leadership approach among nurses
- The future of nurse leadership
- How nurse leaders can ensure team leadership for the best collaboration in healthcare teams
- Impact of recognition program on Registered Nurses motivation level
- Pharmaceutical Companies Overpricing Medication: Background and Policy Landscape
- The Roles of Nursing Organizations in Shaping the future of nursing
Nursing Informatics Capstone Project Ideas for College Students in Kenya
- Adoption of e-learning in healthcare management
- Adoption of transformative technology such as CDSS in clinical settings
- The use of big data in clinical research
- Use of electronic medical records in acute care
- Significance of mHealth apps on mental health care access by rural populations
- Nursing Faculty Perceptions on the Use of Computer-Based Virtual Simulation in an Associate Degree Nursing Program
- Developing and Improving the safety and security of patients through comprehensive data research
- Methods for storing and keeping nursing informatics data
- Data governance in healthcare settings
- Impacts of a healthcare data breach
- Use of Healthcare Information Technology to support evidence-based practice in nursing
- Importance of clinical support decision making systems
- The use of technology to bridge the nurse shortage gaps in rural areas
- Electronic health records in healthcare
- Nurse informatics competencies
- Meaningful use and HIT
- Priorities for informatics investment in the future
- Utilization of modern-day systems for reliable nursing information
- Collaborative decision making through shared governance in healthcare
- Ethics and data management in healthcare
- The use of big data in healthcare settings
- Robotics in surgery
- The use of electronic health records to offer patient-centered care
- Assisting recovering centers
- Role of nursing informatics in quality improvement
- E-learning as a professional development approach among nurses
- Advantages and disadvantages of the current health records system
- Current situation of nursing informatics in developing countries
- Impact of nursing informatics on the quality of nursing services
- HITECH Legislation and Electronic Medical Records in healthcare
- Health Information as a strategic resource in the Australian settings
- The Impact of Nursing Informatics on Patient Outcomes and Patient Care Efficiencies
- Healthcare management information system
- Developing digital literacies for nursing school students
- Barriers to competency development in nursing informatics
- Integrating health informatics to nursing education
- The use of smartphones in inpatient management and education
- The use of simulation for nursing students
Nursing Practice Project Ideas for College Students in Kenya
- Oxygen Use in Patients with COPD
- Measuring Blood Pressure Noninvasively in Children
- Intravenous Catheter Size and Blood Administration
- The historical perspectives on evidence-based nursing
- The ethical side of abortion care
- Adolescent education in gynecology
- Preparations for cesarean section
- Rules for infant resuscitation
- Checklist for delivery list behavior
- Recommendations for prenatal care
- Dealing appropriately with foreign patients
- Data collection ethics in primary healthcare
- Stress management practices for nurses on a night shift
- How to apply the Nurse Bedside Shift Report
- How experience and education impact medication mistakes for Registered nurses
- Consequences of intentional sabotage and bullying for nurses at the workplace
- Analysis of nursing behavior towards HIV and Aids patients
- Psychiatric care and mental health issues in adults
- Productive programs for obesity and weight management among seniors
- A case study of joint disorders in the elderly population
- Interventions for managing socially impaired behavior among adult patients with dementia
- Utilizing technology to boost the safety of patients in nursing homes
Nursing Project Topics for Primary Health Care Research for College Students in Kenya
- Health financing strategy
- Effectiveness of honey-based products in wound care
- Medical staff attitude and knowledge about in-patient falls
- Patient fall rates in the acute care in-patient hospitals
- Patient fall education and patient safety
- Nurse education on patient falls and safety culture
- Strategies to reduce patient injuries from falls
- Fall prevention practices at home
- Evidence-based practice falls intervention strategies in hospital settings.
- The use of video and camera monitoring to prevent falls among elderly patients
- The use of technology in fall prevention
- Role of hospital leadership in preventing patient falls
- Quality improvement program for reducing falls in medical-surgical units
- Factors contributing to psychiatric patient falls in hospitals
- Creating a safety culture that prevents falls
- Multifactorial fall risk assessment
- Healthcare Managers Role in Fall-Related Injury Prevention in Assisted Living Facilities
- Fall risk among osteoporosis patients
- Multifactorial interventions for the prevention of falls among elderly patients
- Use of exercise in reducing falls among elderly patients
- The Morse fall risk scale and its significance in fall risk assessment and management
- Characteristics of at fall risk patients
- Using engineering controls to prevent falls among patients and the elderly
- Outpatient fall risk assessment tool
- Effects of implementing evidence-based fall risk scale on fall rates
- Standardized fall risk assessment tool
- Prevention of patient falls through education
- Fall prevention strategies in home settings
- Fall prevention strategies in hospitals
- Potential causes of falls in hospitals
- Defining fall and fall risk patient
- The use of SPICES framework and FAMILY cards to assess old patients
- Nursing interventions to prevent falls
- Home environment assessment for elderly patients
- Safety awareness activities for elderly patients
- Strategies and tools to address patient falls in nursing homes
- Recommendations based on primary care knowledge
- Ethics for data collection in primary health care
- An economic evaluation of primary health care
- Methods of assessing the quality of medical care
- Environmental assessment and modification as a fall management strategy
- Home modification approach to falls management
- Impacts of the design of healthcare stings/environments on patient fall
- Physical environmental risk factors for elderly falls
- Home safety modifications to reduce fall injuries among geriatric patients
- Defining different methods to manage and process wounds
- Modern vaccination program in rural and remote areas
- Impacts of visiting home nurses on reducing in-patient falls
- Role of pharmacists in addressing patient falls
- An interdisciplinary approach to fall management in clinical settings
- Hourly Rounding and Fall Prevention among the elderly in long term care: A change process.
- The private sector in the mental health system
- Integration of childcare into basic medical care
- ER symptoms that cannot be explained medically
- The involvement of local pharmacists in the work of doctors
- Strategies to curb patient falls in a home setting
- Implementing technology in the prevention of falls among elderly patients
- Fall risk assessment among psychiatric patients
Nursing Topics on ER, Theater & Capstone Project Ideas on Mental Health for College Students in Kenya
- Causes of depression
- Alcohol addiction disorder
- Diagnosis of schizophrenia
- Bipolar disorder
- PTSD for KDF veterans
- Police stress
- Health education approach for mentally ill patients
- Addressing stigma among careers and patients with mental health issues
- Teen aggression and video games
- Use of prohibited substances
- Psychiatric patient ethics
- Methods of recovery and damage to the body
- The link between mental health issues and homelessness
- Detrimental effects of sexual assault on children
- Impacts of domestic violence on children
- The relationship between mental health and {subject of your choice}
- Evaluating readiness for psychological rehabilitation
- How autonomous decision making is affected by mental illness
- Putting postnatal depression into perspective
- Managing dementia patients with non-pharmacological methods
- The correlation between caring behavior and emotional intelligence for nurses in Emergency Rooms
- Analyzing the link between compassion fatigue and exercise among medical surgery nurses
- How to enhance safety in operating rooms
- Ways to boost patient flow in an urgent care facility
- Strategies to curb distress among isolated marrow and blood transplant patients post-transplantation
- Dealing with the aftermath of a cancer surgery
Research Topics for for College Nursing Students in Kenya
- Development of a new mental health guide for educators
- The use of cognitive-behavioral therapy techniques in psychiatric facilities
- Art therapy and mental health
- Causes of suicide among youths
- Child and adolescent psychiatry
- Substance abuse disorders
- Substance abuse among the geriatric population
- Treatment of Arthritis
- Bedside shift report implantation
- Preventing and managing measures of diabetes
- HPV awareness and vaccination
- Visitation model review
- The link between homelessness and mental health issues
- The efficiency of Yoga in maintaining mental health wellbeing
- Use of expressive art therapy for positive youth development
- Using CBT for PTSD affected veterans
- Impact of sexual abuse on children
- How domestic violence affects the children
- Culture-based mental health programs
- Impacts of bullying at the workplace for new nurses
- Planning emergency measures
- Optimizing of a phone app for patients who inflict self-harm
- How ER patients are affected by color
- Emergency salary for nurses
- Can emergency calls be easier?
- Causes and treatment of ADHD
- Vaccination and autism
- Antibiotic resistance in preschool children
- Mental health issues among the aboriginal populations
- Understanding postnatal depression among women
- Mental health nursing for adolescents
- Mental health scales best for children in prison
- Access to mental health services by aboriginals or a specific population
- Lateral violence among nurses
- Effectiveness of mental health services for deaf service users
- Outcome measures for an inpatient with mental health issues
- Mental illness and autonomous decision making
- Psychological rehabilitation readiness assessment
- Links between heritage, arts, museums, and mental health
- Impacts of teenage suicides
- Preparing student nurses to manage trauma in clinical settings
- Mental health simulation models for ADN students
- Perception of Intellectual Disability Nurses by other nurses
- Eating disorders and their effects on social media
- Causes of seizures in infants
- Medical practices for teenagers
- Child obesity and healthy eating
- Psychological aspects of baby care
- Treatment of the acute coronary syndrome
- Obesity and weight management
- Ketamine infusion therapy
- Tobacco dependence
- Safety in the psychiatric centers
- Preventing falls in psychiatric facilities
Midwifery Topics & Women’s Health Research Project Ideas for College Students in Kenya
- Treatment and prognosis for breast cancer
- Ethical rules for infertility
- Menopause Challenge
- Impact of diabetes during pregnancy
- Relationship between HPV and cancer of the cervix
- Prevalence of fibroids and uterine cancer in women
- How breastfeeding impacts immune levels in children
- Modern infant practices
- Analysis of ovarian disorders
- The link between HPV and cervical cancer
- Mammography to detect breast cancers in women
- Gestational diabetes management
- Birth control approach among women
- Ectopic pregnancy
- Breast pumps and breastfeeding
- The use of codeine and tramadol products in breastfeeding women
- Nutritional management during pregnancy
- Management of endometriosis
- Use of supplements when breastfeeding
- Managing menopause
- Reproductive endocrinology
- Sleep disorders in women
- Women’s sexual health disorders
- Emergency contraception/ birth control
- Female genital mutilation and sexual health of women
- Impacts of fibroids on women
- Menopause in women
- Breastfeeding, work, and women of low socio-economic status
- Normal versus cesarean births
- Epidural in induced births
- Pelvic floor issues in women
- Factors that influence the decision to breastfeed
- Causes of vaginal atrophy
- Various practices of pregnant mothers and child delivery in rural areas
- Prenatal designation: first analysis
- Causes of mental illness during the postpartum period
- A review of shift midwives and study length
- Self-taught equipment and training injuries
- The importance of midwives continuing treatment
- Pregnancy challenges to gain weight
- Addressing mental health among pregnant women in rural areas
- Constipation after cesarean surgery
- Analysis of labor efficiency
- Positive experiences with childbirth
- The best safety rules for pregnant women
- Preeclampsia among women
- Postpartum depression among women
- Diabetes management during pregnancy
- Urine incontinence in women
- Uterine cancer and fibroids in women
- Postmenstrual syndrome and hormonal changes
- Smoking and pregnancy
- Infant mortality and preterm birth among African American women
- Teenage pregnancy
- Preventing pregnant women from Zika Virus
Ethical & Controversial Research Topics in Nursing for College Students in Kenya
- Examination of joint disease in the elderly
- Home treatment for patient support during chemotherapy
- Examination of atrial fibrillation
- Therapy for bladder cancer
- Cardiovascular risk reduction
- Intensive care requirements
- Geriatric ethics
- Stroke and cerebrovascular disease
- Restless legs syndrome
- Precautions for Parkinson’s Disease
- The clinical role of a nurse
- Specialist in social work and the role of health promotion
- Between career and professional service
- Diversity of health services
- Uniform code for nurses
- Gender bias in the nursing profession
- Shortage of men in health care
- Legal apologies and medical decisions
- Home medical services
- Health contract restrictions
Pediatric & Nursing Quality Improvement Research Topics for College Students in Kenya
- The maximizing of patient outcome and cutting costs of improved management of fungal infection
- Managing risk of the mortality rate of infant
- Enhancing experiences of cancer patients with easy access to radiotherapy and multidisciplinary assessment
- Employing electronic data in identifying problems of secondary care during weekends
- Online guide or self-help for cancer and depressed teens
- Assessment of child behavior in pediatric primary care
- Ethics in pediatric care
- Reasons why mother’s health may be under threat during childbirth
- Child’s health insurance: right or privilege?
- Evaluation of childbirth efficacy
Related Articles

265+ Project Management Research Topics for College Students in Kenya
Explore this list of 265+ project management research topics for college students in Kenya to get the perfect topic for your next project

270+ Management Research Topics for College Students in Kenya
ContentsNursing Leadership Project Ideas for College Students in KenyaNursing Informatics Capstone Project Ideas for College Students in KenyaNursing Practice Project Ideas for College Students in…

330+ Ethical Research Topics for College Students in Kenya
The need for ethics in research is critical to the integrity of the research process. The basic principles of ethics provide a framework

420+ Biochemistry Research Topics for College Students in Kenya
Biochemistry is a branch of science that investigates the chemical processes that occur in living organisms
280+ Physiology Research Topics for College Students in Kenya
One of the goals of physiology research is to develop new treatments for diseases. Researchers may study how the immune system works in order to develop new vaccines
You must be logged in to post a comment.

IMAGES
VIDEO
COMMENTS
Research Opportunities: Research is the cornerstone of medical advancement, a crucial avenue for expanding knowledge and improving healthcare outcomes. In Kenya, a burgeoning hub of medical education, the landscape is ripe with opportunities for aspiring medical students to engage in impactful research initiatives. These opportunities not only enrich the educational experience but also ...
KENYA PROGRAM OFFICE. AMPATH. P.O. Box 4606. Eldoret, Kenya 30100. +254-532-033-471. [email protected]. For medical assistance, please contact the MTRH Referral line: 0701790434. The AMPATH Habari is a recap of our latest programs, new programs, new priorities, and new ways to help.
Pioneering Clinical Trials and Healthcare Research in Kenya At CliniQuest Research Site, we are dedicated to improving the future of healthcare through groundbreaking clinical trials and in-depth healthcare research in Kenya. Our state-of-the-art facility is committed to developing innovative solutions that address the unique health challenges faced by Kenyans. Join us as we transform the...
The programme was formed in 1989 when the Kenya Medical Research Institute formed a partnership with the Wellcome Trust and the University of Oxford. The Programme has grown from a small group of 12 to a state of the art facility hosting over 100 research scientists and 700 support staff working across Kenya, Uganda and the region. ...
Research for human health in the devolved system of Government in Kenya. In contributing towards realization of Equitable, Affordable and Quality Health Care of the Highest Standard as enshrined in the Constitution of Kenya 2010 and the Country's blue print, Vision 2030 and Universal Health Coverage (UHC), KEMRI has developed a comprehensive framework, under which the Institute is carrying ...
Ethical approval for this study was granted by the Kenya Medical Research Institute (KEMRI) Scientific and Ethics Review Unit (SSC protocol No. 3166). We obtained written consent to take part in the study from the participants prior to the start of the interviews. An information sheet giving a summary of the study purpose and procedures and ...
2017-01-01. Kenya belongs to a high incidence region known as Africa’s esophageal cancer (EC) corridor. It has one of the highest incidence rates of EC worldwide, but research on EC in Kenya has gone highly unnoticed. EC in Kenya is unique in its high percentage of young cases (< 30 years of age).
Kenya Medical Research Institute (KEMRI) is a State Corporation established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and ...
Kenyans and Ugandans need to change their ways to arrest lifestyle diseases. Catherine Kyobutungi, African Population and Health Research Center. Non-communicable diseases are skyrocketing in ...
The Health and Workforce Training & Research Kenya (HETARK) is a Non-Governmental Organization registered and operating in Kenya since 2008, focused on health systems strengthening projects in Africa. Our vision is to transform health service delivery by promoting health research and information technology innovations, while our mission is to ...
The Centre is strategically located in Kisumu City, western Kenya region, in an area that is endemic for major infectious diseases. Since its establishment in 1984, CGHR has been on the world map as the site of ground-breaking research focusing on infectious diseases of medical importance. Specifically, the Centre has carried out cutting-edge ...
The launch marks a turning point in Kenya's efforts for health research agenda setting. The Research for Health Policy Framework is the country's first all-inclusive policy and will provide much-needed prioritization for investment, integration, and coordination of health research. "PATH commends the government for its commitment to ...
Kenya Medical Research Institute P.O. Box 54840 00200 Off Raila Odinga Way. Nairobi, Kenya. Center for Geographic Medicine Research, Coast P.O. Box 230-80108, Kilifi Kenya. Center for Global Health Research (CGHR) P.O. Box: 1578 - 40100, Kisumu, Kenya.
INTRODUCTION. Malaria remains a significant public health concern in Kenya and Ethiopia. Three-quarters of the 48 million residents of Kenya and 52% of the 103 million residents of Ethiopia are at risk of malaria. 1, 2 Despite major progress in malaria control in the past two decades, malaria burden remains high in these two countries.
The principal areas of focus for the College research programs are listed as follows. Besides, internal funding, KMTC actively applies for external research funding to complement internal funding. Scientific Conference and Symposia. Kenya Medical Training College (KMTC) has established a bi-ennial Scientific Conference geared towards enhancing ...
Public Health 24. Radiology and Nuclear medicine 4. Surgery 8. Toxicology 7. Veterinary 7. Virology 13. Below is the list of 25 best universities for Medicine in Kenya ranked based on their research performance: a graph of 367K citations received by 30.4K academic papers made by these universities was used to calculate ratings and create the top.
In Kenya, 47 percent of women aged 15-49 have experienced physical or sexual violence in their lives, with most violence among ever-married women occurring at the hands of a current or former partner. Among adolescent girls 15-19 years, 35 percent report having experienced physical or sexual violence. Physical and sexual violence that occurs in ...
Kenya is a major site of NIAID research funding. The primary areas of focus are HIV/AIDS, malaria, and schistosomiasis. NIAID also conducts and funds research in the United States and abroad on a number of tropical diseases that impact Kenya and other African nations. In 2012, NIAID-funded HIV/AIDS clinical research sites in Kenya joined other ...
Pharmacy and Poisons Board P.O. Box 27663 - 00506 Lenana Road Opp. DOD Nairobi, Kenya. Telephone: (+254) 709 770 100 or (+254) 709 770 xxx (where xxx represents the extension of the officer or office) Email: [email protected] or [email protected] For Clinical Trials Inquiries: [email protected].
Kenya Medical Research Institute P.O. Box 54840 00200 Off Raila Odinga Way. Nairobi, Kenya. Center for Geographic Medicine Research, Coast P.O. Box 230-80108, Kilifi Kenya. Center for Global Health Research (CGHR) P.O. Box: 1578 - 40100, Kisumu, Kenya.
Since 2020, COVID-19 has been a hot-button topic in medicine, along with the long-term symptoms in those with a history of COVID-19. Examples of COVID-19-related research topics worth exploring include: The long-term impact of COVID-19 on cardiac and respiratory health. COVID-19 vaccination rates.
Kenya lacks a nursing and midwifery research strategy to guide research prioritization. Introduction: The goal of this study was to identify and describe nursing and midwifery research priorities for Kenya. Methods: A cross-sectional Delphi survey using two iterative rounds of electronic data collection was used to reach a consensus about ...
The Government of Kenya has been using data, evidence, and multi-stakeholder dialogues to identify and implement strategic interventions to address its health workforce challenges. This supported the strategic investment needed in implementing the Kenya Human Resources for Health (HRH) Strategy 2019-2023, which is the foundation on which WHO ...
Nursing Informatics Capstone Project Ideas for College Students in Kenya. Adoption of e-learning in healthcare management. Adoption of transformative technology such as CDSS in clinical settings. The use of big data in clinical research. Use of electronic medical records in acute care.